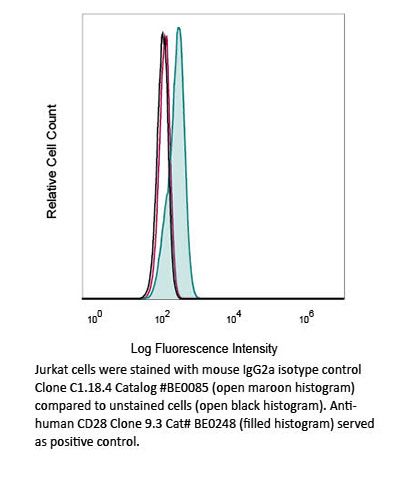
Catalog #BP0085
InVivoPlus mouse IgG2a isotype control, unknown specificity
Clone
C1.18.4
Product Citations
22
Isotype
Mouse IgG2a, κ
You may also be interested in: