InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase
Product Description
Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107775 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
Goschl, L., et al (2018). "A T cell-specific deletion of HDAC1 protects against experimental autoimmune encephalomyelitis" J Autoimmun 86: 51-61.
PubMed
Multiple sclerosis (MS) is a human neurodegenerative disease characterized by the invasion of autoreactive T cells from the periphery into the CNS. Application of pan-histone deacetylase inhibitors (HDACi) ameliorates experimental autoimmune encephalomyelitis (EAE), an animal model for MS, suggesting that HDACi might be a potential therapeutic strategy for MS. However, the function of individual HDAC members in the pathogenesis of EAE is not known. In this study we report that mice with a T cell-specific deletion of HDAC1 (using the Cd4-Cre deleter strain; HDAC1-cKO) were completely resistant to EAE despite the ability of HDAC1cKO CD4(+) T cells to differentiate into Th17 cells. RNA sequencing revealed STAT1 as a prominent upstream regulator of differentially expressed genes in activated HDAC1-cKO CD4(+) T cells and this was accompanied by a strong increase in phosphorylated STAT1 (pSTAT1). This suggests that HDAC1 controls STAT1 activity in activated CD4(+) T cells. Increased pSTAT1 levels correlated with a reduced expression of the chemokine receptors Ccr4 and Ccr6, which are important for the migration of T cells into the CNS. Finally, EAE susceptibility was restored in WT:HDAC1-cKO mixed BM chimeric mice, indicating a cell-autonomous defect. Our data demonstrate a novel pathophysiological role for HDAC1 in EAE and provide evidence that selective inhibition of HDAC1 might be a promising strategy for the treatment of MS.
Clemente-Casares, X., et al (2016). "Expanding antigen-specific regulatory networks to treat autoimmunity" Nature 530(7591): 434-440.
PubMed
Regulatory T cells hold promise as targets for therapeutic intervention in autoimmunity, but approaches capable of expanding antigen-specific regulatory T cells in vivo are currently not available. Here we show that systemic delivery of nanoparticles coated with autoimmune-disease-relevant peptides bound to major histocompatibility complex class II (pMHCII) molecules triggers the generation and expansion of antigen-specific regulatory CD4(+) T cell type 1 (TR1)-like cells in different mouse models, including mice humanized with lymphocytes from patients, leading to resolution of established autoimmune phenomena. Ten pMHCII-based nanomedicines show similar biological effects, regardless of genetic background, prevalence of the cognate T-cell population or MHC restriction. These nanomedicines promote the differentiation of disease-primed autoreactive T cells into TR1-like cells, which in turn suppress autoantigen-loaded antigen-presenting cells and drive the differentiation of cognate B cells into disease-suppressing regulatory B cells, without compromising systemic immunity. pMHCII-based nanomedicines thus represent a new class of drugs, potentially useful for treating a broad spectrum of autoimmune conditions in a disease-specific manner.
Sell, S., et al (2015). "Control of murine cytomegalovirus infection by gammadelta T cells" PLoS Pathog 11(2): e1004481.
PubMed
Infections with cytomegalovirus (CMV) can cause severe disease in immunosuppressed patients and infected newborns. Innate as well as cellular and humoral adaptive immune effector functions contribute to the control of CMV in immunocompetent individuals. None of the innate or adaptive immune functions are essential for virus control, however. Expansion of gammadelta T cells has been observed during human CMV (HCMV) infection in the fetus and in transplant patients with HCMV reactivation but the protective function of gammadelta T cells under these conditions remains unclear. Here we show for murine CMV (MCMV) infections that mice that lack CD8 and CD4 alphabeta-T cells as well as B lymphocytes can control a MCMV infection that is lethal in RAG-1(-/-) mice lacking any T- and B-cells. gammadelta T cells, isolated from infected mice can kill MCMV infected target cells in vitro and, importantly, provide long-term protection in infected RAG-1(-/-) mice after adoptive transfer. gammadelta T cells in MCMV infected hosts undergo a prominent and long-lasting phenotypic change most compatible with the view that the majority of the gammadelta T cell population persists in an effector/memory state even after resolution of the acute phase of the infection. A clonotypically focused Vgamma1 and Vgamma2 repertoire was observed at later stages of the infection in the organs where MCMV persists. These findings add gammadelta T cells as yet another protective component to the anti-CMV immune response. Our data provide clear evidence that gammadelta T cells can provide an effective control mechanism of acute CMV infections, particularly when conventional adaptive immune mechanisms are insufficient or absent, like in transplant patient or in the developing immune system in utero. The findings have implications in the stem cell transplant setting, as antigen recognition by gammadelta T cells is not MHC-restricted and dual reactivity against CMV and tumors has been described.
Grinberg-Bleyer, Y., et al (2015). "Cutting edge: NF-kappaB p65 and c-Rel control epidermal development and immune homeostasis in the skin" J Immunol 194(6): 2472-2476.
PubMed
Psoriasis is an inflammatory skin disease in which activated immune cells and the proinflammatory cytokine TNF are well-known mediators of pathogenesis. The transcription factor NF-kappaB is a key regulator of TNF production and TNF-induced proinflammatory gene expression, and both the psoriatic transcriptome and genetic susceptibility further implicate NF-kappaB in psoriasis etiopathology. However, the role of NF-kappaB in psoriasis remains controversial. We analyzed the function of canonical NF-kappaB in the epidermis using CRE-mediated deletion of p65 and c-Rel in keratinocytes. In contrast to animals lacking p65 or c-Rel alone, mice lacking both subunits developed severe dermatitis after birth. Consistent with its partial histological similarity to human psoriasis, this condition could be prevented by anti-TNF treatment. Moreover, regulatory T cells in lesional skin played an important role in disease remission. Our results demonstrate that canonical NF-kappaB in keratinocytes is essential for the maintenance of skin immune homeostasis and is protective against spontaneous dermatitis.
Park, H. J., et al (2015). "PD-1 upregulated on regulatory T cells during chronic virus infection enhances the suppression of CD8+ T cell immune response via the interaction with PD-L1 expressed on CD8+ T cells" J Immunol 194(12): 5801-5811.
PubMed
Regulatory T (Treg) cells act as terminators of T cell immuniy during acute phase of viral infection; however, their role and suppressive mechanism in chronic viral infection are not completely understood. In this study, we compared the phenotype and function of Treg cells during acute or chronic infection with lymphocytic choriomeningitis virus. Chronic infection, unlike acute infection, led to a large expansion of Treg cells and their upregulation of programmed death-1 (PD-1). Treg cells from chronically infected mice (chronic Treg cells) displayed greater suppressive capacity for inhibiting both CD8(+) and CD4(+) T cell proliferation and subsequent cytokine production than those from naive or acutely infected mice. A contact between Treg and CD8(+) T cells was necessary for the potent suppression of CD8(+) T cell immune response. More importantly, the suppression required cell-specific expression and interaction of PD-1 on chronic Treg cells and PD-1 ligand on CD8(+) T cells. Our study defines PD-1 upregulated on Treg cells and its interaction with PD-1 ligand on effector T cells as one cause for the potent T cell suppression and proposes the role of PD-1 on Treg cells, in addition to that on exhausted T cells, during chronic viral infection.
Ellis, G. T., et al (2015). "TRAIL+ monocytes and monocyte-related cells cause lung damage and thereby increase susceptibility to influenza-Streptococcus pneumoniae coinfection" EMBO Rep 16(9): 1203-1218.
PubMed
Streptococcus pneumoniae coinfection is a major cause of influenza-associated mortality; however, the mechanisms underlying pathogenesis or protection remain unclear. Using a clinically relevant mouse model, we identify immune-mediated damage early during coinfection as a new mechanism causing susceptibility. Coinfected CCR2(-/-) mice lacking monocytes and monocyte-derived cells control bacterial invasion better, show reduced epithelial damage and are overall more resistant than wild-type controls. In influenza-infected wild-type lungs, monocytes and monocyte-derived cells are the major cell populations expressing the apoptosis-inducing ligand TRAIL. Accordingly, anti-TRAIL treatment reduces bacterial load and protects against coinfection if administered during viral infection, but not following bacterial exposure. Post-influenza bacterial outgrowth induces a strong proinflammatory cytokine response and massive inflammatory cell infiltrate. Depletion of neutrophils or blockade of TNF-alpha facilitate bacterial outgrowth, leading to increased mortality, demonstrating that these factors aid bacterial control. We conclude that inflammatory monocytes recruited early, during the viral phase of coinfection, induce TRAIL-mediated lung damage, which facilitates bacterial invasion, while TNF-alpha and neutrophil responses help control subsequent bacterial outgrowth. We thus identify novel determinants of protection versus pathology in influenza-Streptococcus pneumoniae coinfection.
Meisen, W. H., et al (2015). "The Impact of Macrophage- and Microglia-Secreted TNFalpha on Oncolytic HSV-1 Therapy in the Glioblastoma Tumor Microenvironment" Clin Cancer Res 21(14): 3274-3285.
PubMed
PURPOSE: Oncolytic herpes simplex viruses (oHSV) represent a promising therapy for glioblastoma (GBM), but their clinical success has been limited. Early innate immune responses to viral infection reduce oHSV replication, tumor destruction, and efficacy. Here, we characterized the antiviral effects of macrophages and microglia on viral therapy for GBM. EXPERIMENTAL DESIGN: Quantitative flow cytometry of mice with intracranial gliomas (+/-oHSV) was used to examine macrophage/microglia infiltration and activation. In vitro coculture assays of infected glioma cells with microglia/macrophages were used to test their impact on oHSV replication. Macrophages from TNFalpha-knockout mice and blocking antibodies were used to evaluate the biologic effects of TNFalpha on virus replication. TNFalpha blocking antibodies were used to evaluate the impact of TNFalpha on oHSV therapy in vivo. RESULTS: Flow-cytometry analysis revealed a 7.9-fold increase in macrophage infiltration after virus treatment. Tumor-infiltrating macrophages/microglia were polarized toward a M1, proinflammatory phenotype, and they expressed high levels of CD86, MHCII, and Ly6C. Macrophages/microglia produced significant amounts of TNFalpha in response to infected glioma cells in vitro and in vivo. Using TNFalpha-blocking antibodies and macrophages derived from TNFalpha-knockout mice, we discovered TNFalpha-induced apoptosis in infected tumor cells and inhibited virus replication. Finally, we demonstrated the transient blockade of TNFalpha from the tumor microenvironment with TNFalpha-blocking antibodies significantly enhanced virus replication and survival in GBM intracranial tumors. CONCLUSIONS: The results of these studies suggest that FDA approved TNFalpha inhibitors may significantly improve the efficacy of oncolytic virus therapy.
Beug, S. T., et al (2014). "Smac mimetics and innate immune stimuli synergize to promote tumor death" Nat Biotechnol 32(2): 182-190.
PubMed
Smac mimetic compounds (SMC), a class of drugs that sensitize cells to apoptosis by counteracting the activity of inhibitor of apoptosis (IAP) proteins, have proven safe in phase 1 clinical trials in cancer patients. However, because SMCs act by enabling transduction of pro-apoptotic signals, SMC monotherapy may be efficacious only in the subset of patients whose tumors produce large quantities of death-inducing proteins such as inflammatory cytokines. Therefore, we reasoned that SMCs would synergize with agents that stimulate a potent yet safe “cytokine storm.” Here we show that oncolytic viruses and adjuvants such as poly(I:C) and CpG induce bystander death of cancer cells treated with SMCs that is mediated by interferon beta (IFN-beta), tumor necrosis factor alpha (TNF-alpha) and/or TNF-related apoptosis-inducing ligand (TRAIL). This combinatorial treatment resulted in tumor regression and extended survival in two mouse models of cancer. As these and other adjuvants have been proven safe in clinical trials, it may be worthwhile to explore their clinical efficacy in combination with SMCs.
DeBerge, M. P., et al (2014). "Soluble, but not transmembrane, TNF-alpha is required during influenza infection to limit the magnitude of immune responses and the extent of immunopathology" J Immunol 192(12): 5839-5851.
PubMed
TNF-alpha is a pleotropic cytokine that has both proinflammatory and anti-inflammatory functions during influenza infection. TNF-alpha is first expressed as a transmembrane protein that is proteolytically processed to release a soluble form. Transmembrane TNF-alpha (memTNF-alpha) and soluble TNF-alpha (solTNF-alpha) have been shown to exert distinct tissue-protective or tissue-pathologic effects in several disease models. However, the relative contributions of memTNF-alpha or solTNF-alpha in regulating pulmonary immunopathology following influenza infection are unclear. Therefore, we performed intranasal influenza infection in mice exclusively expressing noncleavable memTNF-alpha or lacking TNF-alpha entirely and examined the outcomes. We found that solTNF-alpha, but not memTNF-alpha, was required to limit the size of the immune response and the extent of injury. In the absence of solTNF-alpha, there was a significant increase in the CD8(+) T cell response, including virus-specific CD8(+) T cells, which was due in part to an increased resistance to activation-induced cell death. We found that solTNF-alpha mediates these immunoregulatory effects primarily through TNFR1, because mice deficient in TNFR1, but not TNFR2, exhibited dysregulated immune responses and exacerbated injury similar to that observed in mice lacking solTNF-alpha. We also found that solTNF-alpha expression was required early during infection to regulate the magnitude of the CD8(+) T cell response, indicating that early inflammatory events are critical for the regulation of the effector phase. Taken together, these findings suggest that processing of memTNF-alpha to release solTNF-alpha is a critical event regulating the immune response during influenza infection.
Walsh, K. B., et al (2014). "Animal model of respiratory syncytial virus: CD8+ T cells cause a cytokine storm that is chemically tractable by sphingosine-1-phosphate 1 receptor agonist therapy" J Virol 88(11): 6281-6293.
PubMed
The cytokine storm is an intensified, dysregulated, tissue-injurious inflammatory response driven by cytokine and immune cell components. The cytokine storm during influenza virus infection, whereby the amplified innate immune response is primarily responsible for pulmonary damage, has been well characterized. Now we describe a novel event where virus-specific T cells induce a cytokine storm. The paramyxovirus pneumonia virus of mice (PVM) is a model of human respiratory syncytial virus (hRSV). Unexpectedly, when C57BL/6 mice were infected with PVM, the innate inflammatory response was undetectable until day 5 postinfection, at which time CD8(+) T cells infiltrated into the lung, initiating a cytokine storm by their production of gamma interferon (IFN-gamma) and tumor necrosis factor alpha (TNF-alpha). Administration of an immunomodulatory sphingosine-1-phosphate (S1P) receptor 1 (S1P1R) agonist significantly inhibited PVM-elicited cytokine storm by blunting the PVM-specific CD8(+) T cell response, resulting in diminished pulmonary disease and enhanced survival. IMPORTANCE: A dysregulated overly exuberant immune response, termed a “cytokine storm,” accompanies virus-induced acute respiratory diseases (VARV), is primarily responsible for the accompanying high morbidity and mortality, and can be controlled therapeutically in influenza virus infection of mice and ferrets by administration of sphingosine-1-phosphate 1 receptor (S1P1R) agonists. Here, two novel findings are recorded. First, in contrast to influenza infection, where the cytokine storm is initiated early by the innate immune system, for pneumonia virus of mice (PVM), a model of RSV, the cytokine storm is initiated late in infection by the adaptive immune response: specifically, by virus-specific CD8 T cells via their release of IFN-gamma and TNF-alpha. Blockading these cytokines with neutralizing antibodies blunts the cytokine storm and protects the host. Second, PVM infection is controlled by administration of an S1P1R agonist.
Perng, O. A., et al (2014). "The degree of CD4+ T cell autoreactivity determines cellular pathways underlying inflammatory arthritis" J Immunol 192(7): 3043-3056.
PubMed
Although therapies targeting distinct cellular pathways (e.g., anticytokine versus anti-B cell therapy) have been found to be an effective strategy for at least some patients with inflammatory arthritis, the mechanisms that determine which pathways promote arthritis development are poorly understood. We have used a transgenic mouse model to examine how variations in the CD4(+) T cell response to a surrogate self-peptide can affect the cellular pathways that are required for arthritis development. CD4(+) T cells that are highly reactive with the self-peptide induce inflammatory arthritis that affects male and female mice equally. Arthritis develops by a B cell-independent mechanism, although it can be suppressed by an anti-TNF treatment, which prevented the accumulation of effector CD4(+) Th17 cells in the joints of treated mice. By contrast, arthritis develops with a significant female bias in the context of a more weakly autoreactive CD4(+) T cell response, and B cells play a prominent role in disease pathogenesis. In this setting of lower CD4(+) T cell autoreactivity, B cells promote the formation of autoreactive CD4(+) effector T cells (including Th17 cells), and IL-17 is required for arthritis development. These studies show that the degree of CD4(+) T cell reactivity for a self-peptide can play a prominent role in determining whether distinct cellular pathways can be targeted to prevent the development of inflammatory arthritis.
Weinlich, R., et al (2013). "Protective roles for caspase-8 and cFLIP in adult homeostasis" Cell Rep 5(2): 340-348.
PubMed
Caspase-8 or cellular FLICE-like inhibitor protein (cFLIP) deficiency leads to embryonic lethality in mice due to defects in endothelial tissues. Caspase-8(-/-) and receptor-interacting protein kinase-3 (RIPK3)(-/-), but not cFLIP(-/-) and RIPK3(-/-), double-knockout animals develop normally, indicating that caspase-8 antagonizes the lethal effects of RIPK3 during development. Here, we show that the acute deletion of caspase-8 in the gut of adult mice induces enterocyte death, disruption of tissue homeostasis, and inflammation, resulting in sepsis and mortality. Likewise, acute deletion of caspase-8 in a focal region of the skin induces local keratinocyte death, tissue disruption, and inflammation. Strikingly, RIPK3 ablation rescues both phenotypes. However, acute loss of cFLIP in the skin produces a similar phenotype that is not rescued by RIPK3 ablation. TNF neutralization protects from either acute loss of caspase-8 or cFLIP. These results demonstrate that caspase-8-mediated suppression of RIPK3-induced death is required not only during development but also for adult homeostasis. Furthermore, RIPK3-dependent inflammation is dispensable for the skin phenotype.
Mohr, E., et al (2010). "IFN-{gamma} produced by CD8 T cells induces T-bet-dependent and -independent class switching in B cells in responses to alum-precipitated protein vaccine" Proc Natl Acad Sci U S A 107(40): 17292-17297.
PubMed
Alum-precipitated protein (alum protein) vaccines elicit long-lasting neutralizing antibody responses that prevent bacterial exotoxins and viruses from entering cells. Typically, these vaccines induce CD4 T cells to become T helper 2 (Th2) cells that induce Ig class switching to IgG1. We now report that CD8 T cells also respond to alum proteins, proliferating extensively and producing IFN-gamma, a key Th1 cytokine. These findings led us to question whether adoptive transfer of antigen-specific CD8 T cells alters the characteristic CD4 Th2 response to alum proteins and the switching pattern in responding B cells. To this end, WT mice given transgenic ovalbumin (OVA)-specific CD4 (OTII) or CD8 (OTI) T cells, or both, were immunized with alum-precipitated OVA. Cotransfer of antigen-specific CD8 T cells skewed switching patterns in responding B cells from IgG1 to IgG2a and IgG2b. Blocking with anti-IFN-gamma antibody largely inhibited this altered B-cell switching pattern. The transcription factor T-bet is required in B cells for IFN-gamma-dependent switching to IgG2a. By contrast, we show that this transcription factor is dispensable in B cells both for IFN-gamma-induced switching to IgG2b and for inhibition of switching to IgG1. Thus, T-bet dependence identifies distinct transcriptional pathways in B cells that regulate IFN-gamma-induced switching to different IgG isotypes.
Product Citations
-
-
Neuroscience
TNF-mediated hilar interneuron loss and aberrant granule cell migration are associated with chronic cognitive deficits following TBI.
In Brain Behav Immun on 1 March 2026 by Harris, E. A., Budianto, S., et al.
PubMed
Chronic morbidities, including cognitive impairment, are a common consequence of traumatic brain injury (TBI), with millions currently living with permanent TBI-related disabilities. Recent work has indicated that altered cellular architecture in the dentate gyrus (DG) may play a significant role in the development of chronic cognitive impairment and excitotoxicity. However, current understanding of the temporal progression of these pathological changes in the context of neuroinflammation and chronic cognitive outcomes is limited. This study characterized temporospatial changes in the hilar region of the DG, showing that the population of reelin- and somatostatin-expressing inhibitory interneurons was significantly reduced as early as 7 days post-injury (dpi), and that aberrant migration of excitatory granule cells occurs gradually in the weeks to months following injury. These findings coincided with upregulation of monocyte/macrophage-associated inflammatory mediators, including MIP-1β, MIG, MCP-1, and TNF-α at 7 days dpi, with differential cytokine regulation persisting 120 dpi. Injury was associated with the development of chronic spatial memory impairment and reduced risk-assessment behavior, with a transient reduction in spontaneous anxiety. TNFR1 and TNFR2 were differentially expressed in inhibitory neurons, further implicating TNF-signaling as a driver of hilar neuron loss. Furthermore, systemic administration of anti-TNF-α monoclonal antibody induced significant neuroprotection, attenuated pro-inflammatory mediators, and hilar interneuron loss. These findings suggest that TNF-TNFR signaling plays a crucial role in driving hilar interneuron loss and aberrant granule cell migration, which, in turn, may contribute to the development of excitotoxicity and chronic cognitive deficits.
-
-
Colonic Engyodontium fungus triggers neutrophil antimicrobial activity to suppress Lactobacillus johnsonii-derived glutamic acid-maintained Tregs.
In J Clin Invest on 17 February 2026 by Wang, X., Sun, H., et al.
PubMed
Isolating commensal fungi from mouse intestines has been challenging, limiting our understanding of their role in intestinal immune homeostasis and diseases. Using an Fc fusion protein of the C-type lectin Dectin-2, we successfully purified the commensal Ascomycota fungus Engyodontium sp. from mouse feces. Engyodontium enhances the antimicrobial activity of colonic neutrophils via CARD9 pathway, and exacerbates colitis by impairing the colonization of intestinal Lactobacillus johnsonii (L. johnsonii) WXY strain. L. johnsonii produces high levels of L-glutamic acid by expressing the glutaminase-encoding gene glsA to facilitate Treg expansion via enhancing IL-2 receptor signaling. Patients with Crohn's disease (CD) and ulcerative colitis harbored increased Engyodontium and decreased L. johnsonii abundance. Engyodontium directly induced calprotectin in human colonic neutrophils, and CD patients exhibited lower levels of L-glutamic acid which also promoted human Treg expansion. These findings highlight the Engyodontium-calprotectin axis against the Lactobacillus-glutamate-Treg cascade to aggravate colitis, suggesting commensal Engyodontium-triggered signaling as a therapeutic target for mucosal inflammatory diseases.
-
-
Immunology and Microbiology
Acute peritonitis-induced adipose CD127+ ILC1s express PD-L1 and ameliorate inflammation in mice.
In Nat Commun on 5 February 2026 by Nagata, R., Akama, Y., et al.
PubMed
Peritonitis is an inflammation of the peritoneum primarily caused by gut perforation and consequent bacterial leakage, a known cause of sepsis. Although adipose tissue is recognized as an immunologically active organ, the involvement of adipose tissue innate lymphoid cells (ILC) in regulating peritonitis remains poorly understood. Here, we employ a cecal ligation and puncture mouse model and demonstrate that circulating CD127- group 1 ILC (ILC1) migrate into the mesenteric adipose tissue (MAT) during the inflammatory period of peritonitis. CD127- ILC1s undergo phenotypic changes to become CD127+ ILC1s, resulting in an increased number of CD127+ ILC1s in the MAT. We also show that this population of CD127+ ILC1s expresses PD-L1, exhibits low IFN-γ production, and potentially acts as a negative regulator of TNF production by γδ T cells, thereby controlling acute peritonitis. Our findings suggest that MAT-CD127+ ILC1s play an important regulatory role in acute peritonitis and may represent a potential therapeutic target for sepsis.
-
-
-
Immunology and Microbiology
Immobilized IgG-containing immune complexes require platelets to recruit neutrophils during inflammation.
In J Clin Invest on 2 February 2026 by Bellio, M., Allaeys, I., et al.
PubMed
During vascular injury, platelets are essential for halting bleeding and recruiting neutrophils to prevent microbial invasion. However, in antibody-mediated autoimmune diseases occurring without vascular damage, neutrophils infiltrate tissues and contribute to pathology. Here, we investigated whether the dependence of neutrophils on platelets is conserved in the context of antibody-driven inflammation. Using human cells from individuals with rheumatoid arthritis and a microfluidic system mimicking physiological shear over IgG-containing immune complexes, we demonstrate that despite expressing Fc receptors, neutrophils required platelets to stably adhere to immune complexes under flow. Platelet Fcγ receptor 2a (FcγRIIA) binding was critical for resisting shear stress, while neutrophils used FcγRIIA and FcγRIIIB for immune complex recognition. Platelet P-selectin binding to neutrophil P-selectin glycoprotein ligand 1 (PSGL-1) was essential for recruitment, whereas macrophage-1 antigen (Mac-1) was dispensable. In a mouse model of autoantibody-mediated arthritis, intravital imaging confirmed that neutrophil recruitment relied on PSGL-1. Importantly, expression of FcγRIIA aggravated arthritis, and blockade of PSGL-1, but not Mac-1, in these mice abrogated both the platelet and neutrophil interactions and disease. These findings identify key molecular interactions in platelet-neutrophil cooperation and reveal that platelets are essential enablers of FcR-mediated neutrophil adhesion in antibody-driven inflammation.
-
-
-
Cell Biology
Telomere Shortening Drives Atrial Fibrillation Through VCAM-1 Mediated Atrial Electrical and Structural Remodeling.
In Aging Cell on 1 February 2026 by Wang, Z., Zhao, R., et al.
PubMed
Telomere shortening is a hallmark of aging and has been implicated in cardiovascular disease, but its mechanistic link to atrial fibrillation (AF) remains elusive. Using a high-throughput, single-gene-calibrated dot blot assay, we developed to quantify leukocyte telomere length (LTL). In age-stratified analyses, shorter LTL was associated with AF predominantly in individuals younger than 70 years. In telomerase-deficient (TERT-/-) mice with telomere dysfunction, higher AF inducibility, atrial electrical conduction slowing, and atrial fibrosis were observed. Transcriptomic profiling revealed significant alterations in extracellular matrix and cell adhesion pathways in response to telomere dysfunction. Subsequent validation identified vascular cell adhesion molecule-1 (VCAM-1) as a potential mediator linking telomere shortening to AF-related atrial remodeling. Functional inhibition of VCAM-1 reversed electrophysiological abnormalities, attenuated atrial fibrosis, normalized ECM gene expression-including Col1α1, α-SMA, and CD168-and reduced AF susceptibility by 30%. These findings establish a telomere-VCAM-1 axis that drives atrial remodeling and arrhythmogenesis in aging, and position VCAM-1 as a candidate therapeutic target for age-related AF.
-
-
-
Immunology and Microbiology
-
Cardiovascular biology
CXCR6+ T Cells Drive Immune Checkpoint Inhibitor Myocarditis.
In Circulation on 7 January 2026 by Munir, A. Z., Gutierrez, A., et al.
PubMed
Myocarditis is a severe complication of immune checkpoint inhibitors (ICIs). The major risk factor for ICI myocarditis is the use of combination ICI treatment, especially when relatlimab, a novel anti-LAG-3 (lymphocyte-activation gene 3) antibody, is combined with anti-PD-1 (programmed cell death protein 1) therapy. Although pathogenic T cells are necessary for ICI myocarditis, the specific signaling and T-cell populations that drive cardiac infiltration have not been fully elucidated, especially in setting of anti-LAG-3/PD-1 treatment.
-
-
-
Cancer Research
Fibroblast STAT3 Activation Drives Organ-Specific Premetastatic Niche Formation.
In Cancer Res on 2 January 2026 by Lasse Opsahl, E. L., Espinoza, C. E., et al.
PubMed
Pancreatic cancer is associated with a high rate of metastasis and poor prognosis. The formation of a premetastatic niche (PMN) facilitates cancer cell spread and contributes to cancer mortality. Using murine pancreatic cancer models based on expression of oncogenic KRAS in the pancreas epithelium, we discovered that remodeling of the lung microenvironment occurred in mice bearing pancreatic precursor lesions prior to cancer formation. This early-lesion PMN resembled the PMN in cancer-bearing mice, and both feature characteristics of overt metastasis, such as transcriptional reprogramming, activation of fibroblast STAT3 signaling, and infiltration of immunosuppressive arginase 1-positive macrophages. Both patients with pancreatic cancer and mouse models demonstrated elevated serum IL6. Inactivating oncogenic KRAS reduced serum IL6 and reverted fibroblast STAT3 phosphorylation in mouse lungs; loss of lung fibroblast STAT3 phosphorylation was similarly observed when mice were treated with the pan-RAS inhibitor RMC-7977. Whereas arginase 1-positive macrophage infiltration was dispensable for fibroblast STAT3 activation, IL6 blockade inhibited lung fibroblast STAT3 activation. Functionally, fibroblast STAT3 activation was necessary for lung metastasis establishment and growth. Interestingly, activation of STAT3 in the PMN was present in the lungs but not in the liver, in which fibroblast reprogramming occurred only in overt metastasis, pointing to organ-specific PMN formation. In human metastasis samples, phosphorylated STAT3 in fibroblasts was similarly more abundant in the lungs than liver. Together, these data point to organ-specific mechanisms driving formation of the PMN and indicate that reprogramming of the microenvironment prior to metastasis might support early dissemination of pancreatic cancer.
-
-
-
Cancer Research
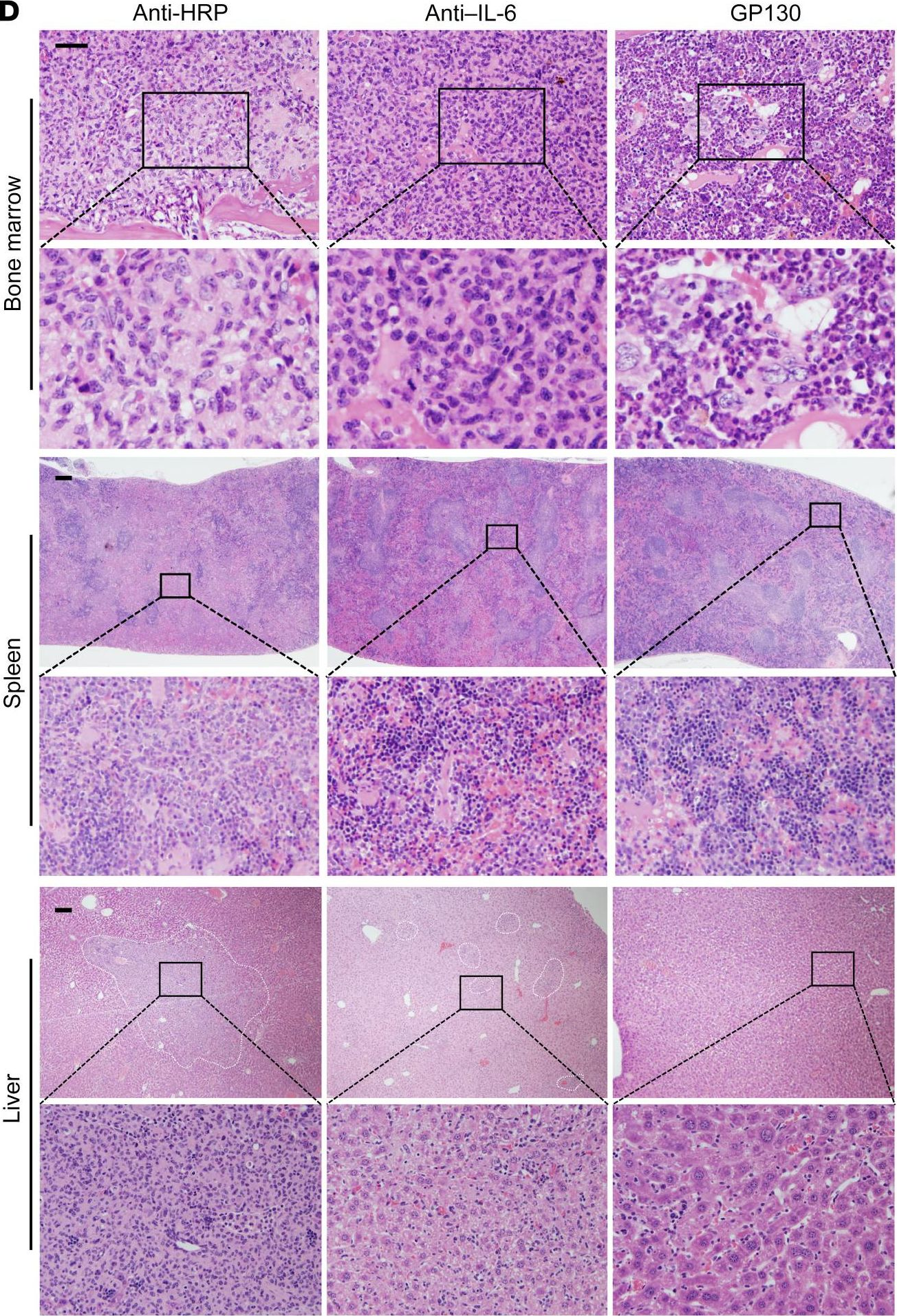
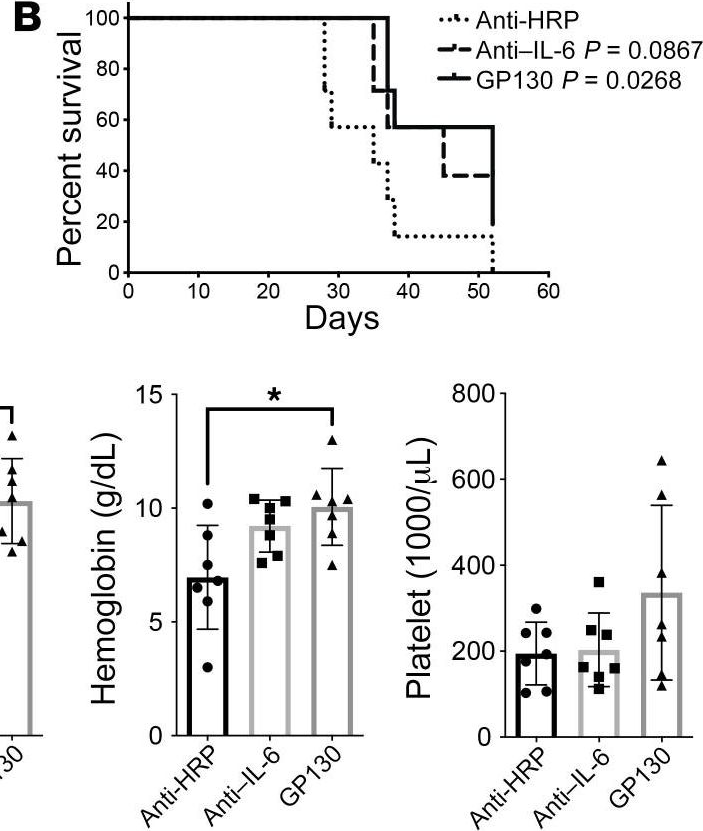
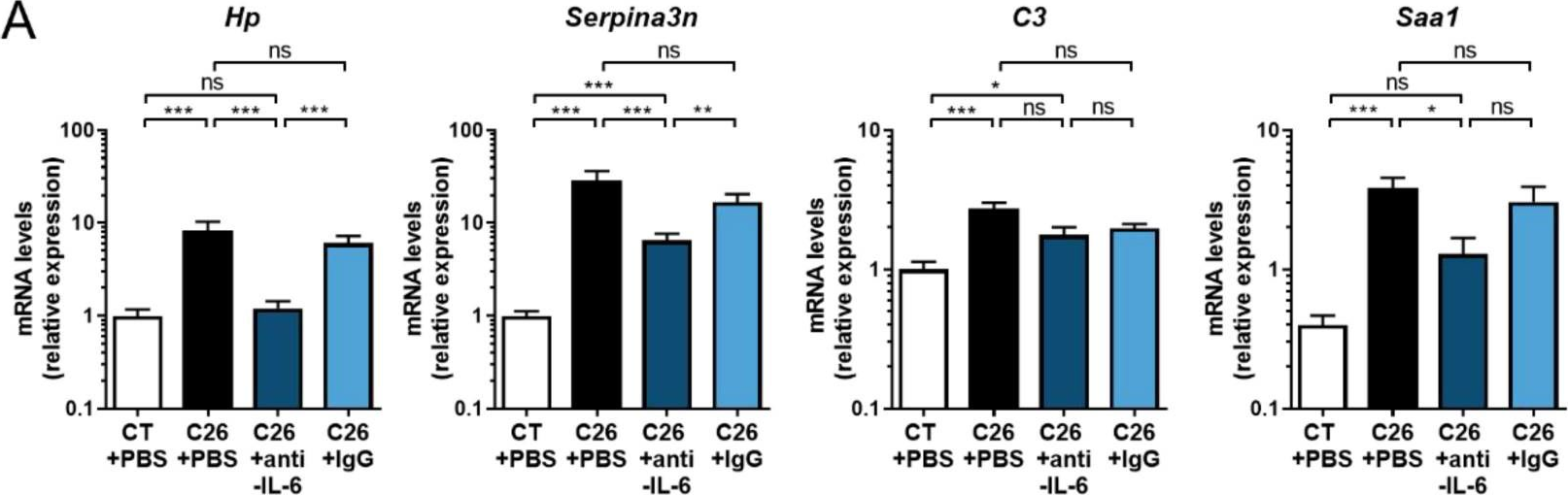
Multi-omics profiling of cachexia-targeted tissues reveals a spatio-temporally coordinated response to cancer.
In Nat Metab on 1 January 2026 by Morigny, P., Vondráčková, M., et al.
PubMed
Cachexia is a wasting disorder associated with high morbidity and mortality in patients with cancer. Tumour-host interaction and maladaptive metabolic reprogramming are substantial, yet poorly understood, contributors to cachexia. Here we present a comprehensive overview of the spatio-temporal metabolic reprogramming during cachexia, using integrated metabolomics, RNA sequencing and 13C-glucose tracing data from multiple tissues and tumours of C26 tumour-bearing male mice at different disease stages. We identified one-carbon metabolism as a tissue-overarching pathway characteristic for metabolic wasting in mice and patients and linked to inflammation, glucose hypermetabolism and atrophy in muscle. The same metabolic rewiring also occurred in five additional mouse models, namely Panc02, 8025, ApcMin, LLC and KPP, and a humanised cachexia mouse model. Together, our study provides a molecular framework for understanding metabolic reprogramming and the multi-tissue metabolite-coordinated response during cancer cachexia progression, with one-carbon metabolism as a tissue-overarching mechanism linked to wasting.
-
-
-
Immunology and Microbiology
-
Genetics
mRNA vaccine expressing enterovirus D68 virus-like particles induces potent neutralizing antibodies and protects against infection.
In Mol Ther Nucleic Acids on 9 December 2025 by Kunishima, Y., Senpuku, K., et al.
PubMed
Enterovirus D68 (EV-D68) causes respiratory illness in children. It also causes severe paralysis called acute flaccid myelitis (AFM), which has become a global health threat. Here, we generated an mRNA vaccine expressing virus-like particles (VLPs) of EV-D68. We found that the mRNA vaccine elicited potent neutralizing antibodies against EV-D68 in the blood, and the neutralizing titer was superior to that of the inactivated whole virion (IWV) vaccine. The mRNA vaccine showed protective effects against intranasal challenge with EV-D68, and antisera from the vaccinated mice prevented the paralysis caused by EV-D68 infection in neonatal mice. Moreover, the mRNA vaccine induced neutralizing antibodies in the respiratory tract, which is the entry site for EV-D68. Additionally, it attenuated infection with coxsackievirus B3 (CVB3), which belongs to another enterovirus group, via CD8+ T cell responses. In conclusion, our results suggest that this mRNA vaccine is a promising candidate for EV-D68 prevention.
-
-
-
Biochemistry and Molecular biology
-
Immunology and Microbiology
Bone marrow-derived CD169+ macrophages promote autoimmune hepatitis by recruiting CCR2+ monocytes via secreting CCL12.
In Exp Mol Med on 1 December 2025 by Lin, B., Zhang, H., et al.
PubMed
CD169+ macrophages, a unique subset of macrophages that cannot be simply defined as M1 or M2 macrophages, have been reported to be associated with various autoimmune diseases. However, the role of CD169+ macrophages in autoimmune hepatitis (AIH) is largely unknown. Here we found that the infiltration of CD169+ macrophages increased in the liver of patients with AIH and strongly positively correlated with inflammation degree. In a mouse model, depletion of CD169+ macrophages ameliorated ConA-induced acute liver injury. Immune homeostasis was also improved when CD169+ macrophages were depleted, as the infiltration of monocytes, macrophages and T cells decreased. Bone marrow-derived Ly6ChiCD169+ macrophages were further identified as the crucial subset in AIH. Next, we found that CD169+ macrophages were IFNγ-responsive and IFNγ could induce the expression of CD169. In response to the IFNγ signal, CD169+ macrophages actively secrete chemokine (C-C motif) ligand (CCL12), thus recruiting CCR2+ monocytes and macrophages to exacerbate AIH. Finally, neutralizing CCL12 improved AIH. Our results suggest that bone marrow-derived CD169+ macrophages, the key subset of macrophages in AIH, actively secrete CCL12 in response to IFNγ to recruit CCR2+ monocytes and macrophages, thus exacerbating AIH. The CD169+ macrophages are a potential therapeutic target in AIH.
-
-
-
Biochemistry and Molecular biology
-
Immunology and Microbiology
-
Cell Biology
Skeletal muscle-derived IL-33 mediates muscle-to-bone crosstalk and regulates bone metabolism via CD8+ T cell-secreted CCL5.
In EBioMedicine on 1 December 2025 by Liu, M., Han, Y., et al.
PubMed
Skeletal muscle-to-bone crosstalk may play critical roles in the association between muscle atrophy and bone loss. Here, we report a myokine, IL-33, which may mediate muscle-to-bone crosstalk.
-
-
-
Cancer Research
-
Immunology and Microbiology
Aging alters tumor cell - T cell crosstalk to promote breast cancer progression
In bioRxiv on 17 November 2025 by Yin, S., Yeung, K. T., et al.
-
-
-
Immunology and Microbiology
-
Cancer Research
CBX6 induces CD8+ T cell exhaustion and tumor development in esophageal squamous cell carcinoma through SMARCD1-mediated CCL8 secretion and lactate efflux.
In Cell Biol Toxicol on 12 November 2025 by Wang, L., Liu, G., et al.
PubMed
This study investigates the functions of chromobox 6 (CBX6) in esophageal squamous cell carcinoma (ESCC) and delves into its functional mechanisms. The bioinformatics insights suggested that CBX6 was overexpressed in ESCC and linked to dismal prognosis. Cbx6 knockdown was induced in mouse mEC25 cells. This procedure curbed the proliferation and migration of mEC25 cells and reduced exhaustion of the co-cultured CD8+ T cells. In vivo, Cbx6 knockdown in mEC25 cells reduced tumorigenesis while enhancing immune activity in mice. Further experiments showed that CBX6 reduced CD8+ T cell cytotoxicity by secreting C-C motif chemokine ligand 8 (CCL8) and promoting monocarboxylate transporter 4 (MCT4)-mediated lactate transport. Regarding the mechanism, CBX6 regulated the expression of SWI/SNF related BAF chromatin remodeling complex subunit D1 (Smarcd1) to modulate chromatin remodeling, thus promoting transcription of Ccl8 and Slc16a3 (encoding MCT4). Smarcd1 overexpression restored metabolic activity in mEC25 cells, reduced activity of co-cultured CD8+ T cells, and promoted tumorigenesis in vivo. Tissue microarrays analysis suggested that CBX6 and SMARCD1 were linked to immunosuppression and poor prognosis in clinical samples. In conclusion, this study suggests that CBX6 induces CD8+ T cell exhaustion and tumor development in ESCC through SMARCD1-mediated CCL8 secretion and lactate efflux.
-
-
-
Immunology and Microbiology
S. aureus exposure during cutaneous antigen sensitization causes basophil- and interleukin-4-dependent exaggerated food anaphylaxis.
In Immunity on 11 November 2025 by Das, M., Alasharee, M., et al.
PubMed
The mechanism of the association of S. aureus skin colonization with food allergy in atopic dermatitis (AD) is unknown. Interleukin-4 (IL-4) plays an important role in food allergy. We found elevated serum IL-4 concentrations in AD patients with S. aureus skin colonization and food allergy. Using an AD mouse model, we demonstrated that epicutaneous application of antigen together with superantigen-producing S. aureus, or staphylococcal enterotoxin B (SEB), caused a heightened systemic antigen-specific T helper-2 (Th2) response and elevated serum IL-4 concentrations. T cell-derived IL-4 acted on intestinal epithelial cells to enhance intestinal permeability and anaphylaxis to enteral antigen challenge. CD40-dependent SEB binding to keratinocytes triggered IL-33 release, which caused T cells to produce IL-3 that elicited a basophil influx in skin-draining lymph nodes (dLNs). Basophil-derived IL-4 augmented Th2 cell polarization by antigen-bearing dendritic cells from skin dLNs. These results suggest therapeutic interventions that might attenuate food allergy in AD patients.
-
-
-
Immunology and Microbiology
Identification of distinct cDC2 subpopulations that direct microbiota-specific T cell differentiation
In bioRxiv on 5 November 2025 by Carroll, S. L., Ly, A., et al.
-
-
-
Immunology and Microbiology
Salmonella-superspreader hosts require gut regulatory T cells to maintain a disease-tolerant state.
In J Exp Med on 3 November 2025 by Di Luccia, B., Massis, L. M., et al.
PubMed
Host-pathogen interactions involve two critical strategies: resistance, whereby hosts clear invading microbes, and tolerance, whereby hosts carry high pathogen burden asymptomatically. Here, we investigate mechanisms by which Salmonella-superspreader (SSP) hosts maintain an asymptomatic state during chronic infection. We found that regulatory T cells (Tregs) are essential for this disease-tolerant state, limiting intestinal immunopathology and enabling SSP hosts to thrive, while facilitating Salmonella transmission. Treg depletion in SSP mice resulted in decreased survival, heightened gut inflammation, and impairment of the intestinal barrier, without affecting Salmonella persistence. Colonic Tregs from SSP mice exhibited a unique transcriptomic profile characterized by the upregulation of type 1 inflammatory genes, including the transcription factor T-bet. In the absence of Tregs, we observed robust expansion of cytotoxic CD4+ T cells, with CD4+ T cell depletion restoring homeostasis. These results uncover a critical host strategy to establish disease tolerance during chronic enteric infection, providing novel insights into mucosal responses to persistent pathogens and chronic intestinal inflammation.
-
-
-
Cancer Research
-
Immunology and Microbiology
Therapy-Induced ECM Remodeling Creates a Transient Immune Barrier in Residual Melanoma.
In Adv Sci (Weinh) on 1 November 2025 by Hsu, C. H., Chen, J., et al.
PubMed
Targeted therapies reshape the tumor not only by eliminating malignant cells but also by altering the stromal and immunologic adaptations that emerge during treatment, which remain incompletely defined. Here, extracellular matrix (ECM) remodeling is identified as a key driver of immune exclusion during the residual disease phase-a transient, therapy-tolerant state that precedes overt resistance. Using an immune-competent melanoma model and temporal transcriptomic profiling of tumor cells and fibroblasts, a coordinated induction of ECM-related genes, particularly collagen, is uncovered during the development of residual disease. This remodeling creates a physical barrier that spatially excludes CD8⁺ T cells from residual tumor niches, compromising immune surveillance. Human melanoma datasets validate increased ECM gene expression and show an inverse correlation between collagen and cytotoxic T lymphocyte infiltration, as well as patient survival. Strikingly, pharmacologic inhibition of collagen deposition, administered at the point of maximal tumor regression, restores CD8⁺ T cell infiltration and delays resistance in a CD8⁺ T cell-dependent manner. These findings define residual disease as a therapeutically actionable stromal state and demonstrate that ECM modulation can overcome immune exclusion, thereby improving the durability of targeted therapy responses.
-
-
-
Cancer Research
-
Immunology and Microbiology
VEGFR2 blockade converts thermally ablative focused ultrasound into a potent driver of T cell-dependent anti-tumor immunity
In bioRxiv on 24 October 2025 by Schwartz, M. R., Anwar, N. Z., et al.
-
-
-
Immunology and Microbiology
-
Neuroscience
IL-6 Inhibition Partially Ameliorates Maternal Immune Activation-Induced Autism-Like Behavioral Abnormalities in Mice.
In Curr Issues Mol Biol on 16 October 2025 by Zhang, X., Luo, W., et al.
PubMed
Prenatal maternal immune activation (MIA) has been implicated in autism spectrum disorder (ASD) pathogenesis, with interleukin-6 (IL-6) identified as a key inflammatory mediator. We investigated the therapeutic potential of IL-6 inhibition in an MIA mouse model induced by Toxoplasma gondii soluble tachyzoite antigen (STAg). Adult MIA offspring received systemic administration of the IL-6-neutralizing antibody (MP5-20F3) or isotype control, followed by behavioral assessments one week later. Open field and elevated plus maze tests revealed heightened anxiety-like behaviors in the STAg offspring, which were largely reversed by IL-6 inhibition. Reciprocal social interaction tests showed diminished sociability in the STAg offspring, which was partially restored by IL-6 inhibition. However, core ASD-like features, including impaired social preference and recognition in the three-chamber test, as well as increased repetitive behaviors, remained resistant to IL-6 inhibition. These findings demonstrate that STAg-induced MIA elicits anxiety-like and ASD-like phenotypes in adult offspring, with IL-6 playing an important role in anxiety-like behaviors and social interaction deficits. Systemic IL-6 inhibition partially ameliorates behavioral abnormalities. This study suggests that IL-6-targeted therapies may address a subset of ASD-related symptoms, and comprehensive strategies are needed for broader efficacy.
-
-
-
Cancer Research
-
Flow cytometry/Cell sorting
Single-cell profiling of ERBB family receptors identifies ERBB3 as a key regulator in head and neck squamous cell carcinoma progression.
In Discov Oncol on 9 October 2025 by Luo, Y., Li, Y., et al.
PubMed
The ERBB receptor family is widely implicated in epithelial malignancies, yet the functional and immunological significance of ERBB3 in head and neck squamous cell carcinoma (HNSCC) remains insufficiently characterized. In this study, we employed single-cell and bulk transcriptomic analyses to comprehensively map the expression patterns and prognostic value of ERBB family members in HNSCC, identifying ERBB3 as a tumor-specific marker predominantly enriched in malignant epithelial clusters. Notably, high ERBB3 expression was paradoxically associated with favorable overall survival, prompting further mechanistic investigation. Functional assays in SCC9 cells demonstrated that ERBB3 promotes proliferation, colony formation, and invasion. Immune profiling revealed that ERBB3-high tumors displayed enhanced communication with B cell subsets, particularly involving immunosuppressive signals such as TNFRSF13B and IL4R. Flow cytometry analysis in a 4NQO-induced mouse model showed that ERBB3 inhibition reduced CCDC50⁺ B cells while restoring MHC-II expression, indicating a shift toward immune activation. These findings highlight a dual role of ERBB3 in HNSCC, acting both as an oncogenic contributor and an immune-modulatory regulator, and position ERBB3 as a promising context-dependent therapeutic target.
-