InVivoPlus anti-mouse CSF1R (CD115)
Product Description
Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoPlus rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Not available or unknown |
| Reported Applications |
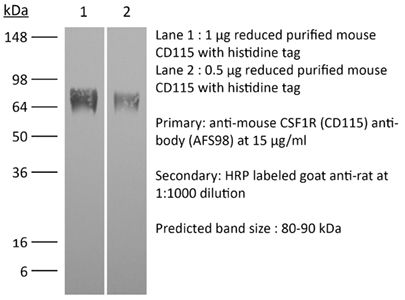
in vivo macrophage depletion in vitro CSF1R neutralization in vivo monocyte depletion Flow cytometry Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin* |
≤0.5EU/mg (≤0.0005EU/μg) Determined by LAL assay |
| Aggregation* |
<5% Determined by SEC |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2687699 |
| Molecular Weight | 150 kDa |
| Murine Pathogen Tests* |
Ectromelia/Mousepox Virus: Negative Hantavirus: Negative K Virus: Negative Lactate Dehydrogenase-Elevating Virus: Negative Lymphocytic Choriomeningitis virus: Negative Mouse Adenovirus: Negative Mouse Cytomegalovirus: Negative Mouse Hepatitis Virus: Negative Mouse Minute Virus: Negative Mouse Norovirus: Negative Mouse Parvovirus: Negative Mouse Rotavirus: Negative Mycoplasma Pulmonis: Negative Pneumonia Virus of Mice: Negative Polyoma Virus: Negative Reovirus Screen: Negative Sendai Virus: Negative Theiler’s Murine Encephalomyelitis: Negative |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo macrophage depletion
Bauche, D., et al (2018). "LAG3(+) Regulatory T Cells Restrain Interleukin-23-Producing CX3CR1(+) Gut-Resident Macrophages during Group 3 Innate Lymphoid Cell-Driven Colitis" Immunity 49(2): 342-352 e345.
PubMed
Interleukin-22 (IL-22)-producing group 3 innate lymphoid cells (ILC3) maintains gut homeostasis but can also promote inflammatory bowel disease (IBD). The regulation of ILC3-dependent colitis remains to be elucidated. Here we show that Foxp3(+) regulatory T cells (Treg cells) prevented ILC3-mediated colitis in an IL-10-independent manner. Treg cells inhibited IL-23 and IL-1beta production from intestinal-resident CX3CR1(+) macrophages but not CD103(+) dendritic cells. Moreover, Treg cells restrained ILC3 production of IL-22 through suppression of CX3CR1(+) macrophage production of IL-23 and IL-1beta. This suppression was contact dependent and was mediated by latent activation gene-3 (LAG-3)-an immune checkpoint receptor-expressed on Treg cells. Engagement of LAG-3 on MHC class II drove profound immunosuppression of CX3CR1(+) tissue-resident macrophages. Our study reveals that the health of the intestinal mucosa is maintained by an axis driven by Treg cells communication with resident macrophages that withhold inflammatory stimuli required for ILC3 function.
in vivo macrophage depletion
Gordon, S. R., et al (2017). "PD-1 expression by tumour-associated macrophages inhibits phagocytosis and tumour immunity" Nature 545(7655): 495-499.
PubMed
Programmed cell death protein 1 (PD-1) is an immune checkpoint receptor that is upregulated on activated T cells for the induction of immune tolerance. Tumour cells frequently overexpress the ligand for PD-1, programmed cell death ligand 1 (PD-L1), facilitating their escape from the immune system. Monoclonal antibodies that block the interaction between PD-1 and PD-L1, by binding to either the ligand or receptor, have shown notable clinical efficacy in patients with a variety of cancers, including melanoma, colorectal cancer, non-small-cell lung cancer and Hodgkin’s lymphoma. Although it is well established that PD-1-PD-L1 blockade activates T cells, little is known about the role that this pathway may have in tumour-associated macrophages (TAMs). Here we show that both mouse and human TAMs express PD-1. TAM PD-1 expression increases over time in mouse models of cancer and with increasing disease stage in primary human cancers. TAM PD-1 expression correlates negatively with phagocytic potency against tumour cells, and blockade of PD-1-PD-L1 in vivo increases macrophage phagocytosis, reduces tumour growth and lengthens the survival of mice in mouse models of cancer in a macrophage-dependent fashion. This suggests that PD-1-PD-L1 therapies may also function through a direct effect on macrophages, with substantial implications for the treatment of cancer with these agents.
in vivo macrophage depletion
Moynihan, K. D., et al (2016). "Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses" Nat Med. doi : 10.1038/nm.4200.
PubMed
Checkpoint blockade with antibodies specific for cytotoxic T lymphocyte-associated protein (CTLA)-4 or programmed cell death 1 (PDCD1; also known as PD-1) elicits durable tumor regression in metastatic cancer, but these dramatic responses are confined to a minority of patients. This suboptimal outcome is probably due in part to the complex network of immunosuppressive pathways present in advanced tumors, which are unlikely to be overcome by intervention at a single signaling checkpoint. Here we describe a combination immunotherapy that recruits a variety of innate and adaptive immune cells to eliminate large tumor burdens in syngeneic tumor models and a genetically engineered mouse model of melanoma; to our knowledge tumors of this size have not previously been curable by treatments relying on endogenous immunity. Maximal antitumor efficacy required four components: a tumor-antigen-targeting antibody, a recombinant interleukin-2 with an extended half-life, anti-PD-1 and a powerful T cell vaccine. Depletion experiments revealed that CD8+ T cells, cross-presenting dendritic cells and several other innate immune cell subsets were required for tumor regression. Effective treatment induced infiltration of immune cells and production of inflammatory cytokines in the tumor, enhanced antibody-mediated tumor antigen uptake and promoted antigen spreading. These results demonstrate the capacity of an elicited endogenous immune response to destroy large, established tumors and elucidate essential characteristics of combination immunotherapies that are capable of curing a majority of tumors in experimental settings typically viewed as intractable.
in vivo macrophage depletion
Arnold, I. C., et al (2015). "CD11c monocyte/macrophages promote chronic Helicobacter hepaticus-induced intestinal inflammation through the production of IL-23" Mucosal Immunol. doi : 10.1038/mi.2015.65.
PubMed
In inflammatory bowel diseases, a breakdown in host microbial interactions accompanies sustained activation of immune cells in the gut. Functional studies suggest a key role for interleukin-23 (IL-23) in orchestrating intestinal inflammation. IL-23 can be produced by various mononuclear phagocytes (MNPs) following acute microbial stimulation, but little is known about the key cellular sources of IL-23 that drive chronic intestinal inflammation. Here we have addressed this question using a physiological model of bacteria-driven colitis. By combining conditional gene ablation and gene expression profiling, we found that IL-23 production by CD11c+ MNPs was essential to trigger intestinal immunopathology and identified MHCII+ monocytes and macrophages as the major source of IL-23. Expression of IL-23 by monocytes was acquired during their differentiation in the intestine and correlated with the expression of major histocompatibility complex class II (MHCII) and CD64. In contrast, Batf3-dependent CD103+ CD11b- dendritic cells were dispensable for bacteria-induced colitis in this model. These studies reinforce the pathogenic role of monocytes in dysregulated responses to intestinal bacteria and identify production of IL-23 as a key component of this response. Further understanding of the functional sources of IL-23 in diverse forms of intestinal inflammation may lead to novel therapeutic strategies aimed at interrupting IL-23-driven immune pathology.Mucosal Immunology advance online publication 5 August 2015. doi:10.1038/mi.2015.65.
in vivo macrophage depletion
Kaminsky, L. W., et al (2015). "Redundant Function of Plasmacytoid and Conventional Dendritic Cells Is Required To Survive a Natural Virus Infection" J Virol 89(19): 9974-9985.
PubMed
Viruses that spread systemically from a peripheral site of infection cause morbidity and mortality in the human population. Innate myeloid cells, including monocytes, macrophages, monocyte-derived dendritic cells (mo-DC), and dendritic cells (DC), respond early during viral infection to control viral replication, reducing virus spread from the peripheral site. Ectromelia virus (ECTV), an orthopoxvirus that naturally infects the mouse, spreads systemically from the peripheral site of infection and results in death of susceptible mice. While phagocytic cells have a requisite role in the response to ECTV, the requirement for individual myeloid cell populations during acute immune responses to peripheral viral infection is unclear. In this study, a variety of myeloid-specific depletion methods were used to dissect the roles of individual myeloid cell subsets in the survival of ECTV infection. We showed that DC are the primary producers of type I interferons (T1-IFN), requisite cytokines for survival, following ECTV infection. DC, but not macrophages, monocytes, or granulocytes, were required for control of the virus and survival of mice following ECTV infection. Depletion of either plasmacytoid DC (pDC) alone or the lymphoid-resident DC subset (CD8alpha(+) DC) alone did not confer lethal susceptibility to ECTV. However, the function of at least one of the pDC or CD8alpha(+) DC subsets is required for survival of ECTV infection, as mice depleted of both populations were susceptible to ECTV challenge. The presence of at least one of these DC subsets is sufficient for cytokine production that reduces ECTV replication and virus spread, facilitating survival following infection. IMPORTANCE: Prior to the eradication of variola virus, the orthopoxvirus that causes smallpox, one-third of infected people succumbed to the disease. Following successful eradication of smallpox, vaccination rates with the smallpox vaccine have significantly dropped. There is now an increasing incidence of zoonotic orthopoxvirus infections for which there are no effective treatments. Moreover, the safety of the smallpox vaccine is of great concern, as complications may arise, resulting in morbidity. Like many viruses that cause significant human diseases, orthopoxviruses spread from a peripheral site of infection to become systemic. This study elucidates the early requirement for innate immune cells in controlling a peripheral infection with ECTV, the causative agent of mousepox. We report that there is redundancy in the function of two innate immune cell subsets in controlling virus spread early during infection. The viral control mediated by these cell subsets presents a potential target for therapies and rational vaccine design.
in vivo monocyte depletion
Naik, S., et al (2015). "Commensal-dendritic-cell interaction specifies a unique protective skin immune signature" Nature 520(7545): 104-108.
PubMed
The skin represents the primary interface between the host and the environment. This organ is also home to trillions of microorganisms that play an important role in tissue homeostasis and local immunity. Skin microbial communities are highly diverse and can be remodelled over time or in response to environmental challenges. How, in the context of this complexity, individual commensal microorganisms may differentially modulate skin immunity and the consequences of these responses for tissue physiology remains unclear. Here we show that defined commensals dominantly affect skin immunity and identify the cellular mediators involved in this specification. In particular, colonization with Staphylococcus epidermidis induces IL-17A(+) CD8(+) T cells that home to the epidermis, enhance innate barrier immunity and limit pathogen invasion. Commensal-specific T-cell responses result from the coordinated action of skin-resident dendritic cell subsets and are not associated with inflammation, revealing that tissue-resident cells are poised to sense and respond to alterations in microbial communities. This interaction may represent an evolutionary means by which the skin immune system uses fluctuating commensal signals to calibrate barrier immunity and provide heterologous protection against invasive pathogens. These findings reveal that the skin immune landscape is a highly dynamic environment that can be rapidly and specifically remodelled by encounters with defined commensals, findings that have profound implications for our understanding of tissue-specific immunity and pathologies.
in vitro CSF-R1 neutralization
Sheng, K. C., et al (2014). "IL-3 and CSF-1 interact to promote generation of CD11c+ IL-10-producing macrophages" PLoS One 9(4): e95208.
PubMed
Unraveling the mechanisms of hematopoiesis regulated by multiple cytokines remains a challenge in hematology. IL-3 is an allergic cytokine with the multilineage potential, while CSF-1 is produced in the steady state with restricted lineage coverage. Here, we uncovered an instructive role of CSF-1 in IL-3-mediated hematopoiesis. CSF-1 significantly promoted IL-3-driven CD11c+ cell expansion and dampened basophil and mast cell generation from C57BL/6 bone marrow. Further studies indicated that the CSF-1/CSF-1R axis contributed significantly to IL-3-induced CD11c+ cell generation through enhancing c-Fos-associated monopoiesis. CD11c+ cells induced by IL-3 or IL-3/CSF-1 were competent in cellular maturation and endocytosis. Both IL-3 and IL-3/CSF-1 cells lacked classical dendritic cell appearance and resembled macrophages in morphology. Both populations produced a high level of IL-10, in addition to IL-1, IL-6 and TNFalpha, in response to LPS, and were relatively poor T cell stimulators. Collectively, these findings reveal a role for CSF-1 in mediating the IL-3 hematopoietic pathway through monopoiesis, which regulates expansion of CD11c+ macrophages.
in vivo monocyte depletion
Greter, M., et al (2012). "GM-CSF controls nonlymphoid tissue dendritic cell homeostasis but is dispensable for the differentiation of inflammatory dendritic cells" Immunity 36(6): 1031-1046.
PubMed
GM-CSF (Csf-2) is a critical cytokine for the in vitro generation of dendritic cells (DCs) and is thought to control the development of inflammatory DCs and resident CD103(+) DCs in some tissues. Here we showed that in contrast to the current understanding, Csf-2 receptor acts in the steady state to promote the survival and homeostasis of nonlymphoid tissue-resident CD103(+) and CD11b(+) DCs. Absence of Csf-2 receptor on lung DCs abrogated the induction of CD8(+) T cell immunity after immunization with particulate antigens. In contrast, Csf-2 receptor was dispensable for the differentiation and innate function of inflammatory DCs during acute injuries. Instead, inflammatory DCs required Csf-1 receptor for their development. Thus, Csf-2 is important in vaccine-induced CD8(+) T cell immunity through the regulation of nonlymphoid tissue DC homeostasis rather than control of inflammatory DCs in vivo.
Flow Cytometry
Li, W., et al (2012). "Intravital 2-photon imaging of leukocyte trafficking in beating heart" J Clin Invest 122(7): 2499-2508.
PubMed
Two-photon intravital microscopy has substantially broadened our understanding of tissue- and organ-specific differences in the regulation of inflammatory responses. However, little is known about the dynamic regulation of leukocyte recruitment into inflamed heart tissue, largely due to technical difficulties inherent in imaging moving tissue. Here, we report a method for imaging beating murine hearts using intravital 2-photon microscopy. Using this method, we visualized neutrophil trafficking at baseline and during inflammation. Ischemia reperfusion injury induced by transplantation or transient coronary artery ligation led to recruitment of neutrophils to the heart, their extravasation from coronary veins, and infiltration of the myocardium where they formed large clusters. Grafting hearts containing mutant ICAM-1, a ligand important for neutrophil recruitment, reduced the crawling velocities of neutrophils within vessels, and markedly inhibited their extravasation. Similar impairment was seen with the inhibition of Mac-1, a receptor for ICAM-1. Blockade of LFA-1, another ICAM-1 receptor, prevented neutrophil adherence to endothelium and extravasation in heart grafts. As inflammatory responses in the heart are of great relevance to public health, this imaging approach holds promise for studying cardiac-specific mechanisms of leukocyte recruitment and identifying novel therapeutic targets for treating heart disease.
Flow Cytometry
Tagliani, E., et al (2011). "Coordinate regulation of tissue macrophage and dendritic cell population dynamics by CSF-1" J Exp Med 208(9): 1901-1916.
PubMed
Tissue macrophages (Mphis) and dendritic cells (DCs) play essential roles in tissue homeostasis and immunity. How these cells are maintained at their characteristic densities in different tissues has remained unclear. Aided by a novel flow cytometric technique for assessing relative rates of blood-borne precursor recruitment, we examined Mphi and DC population dynamics in the pregnant mouse uterus, where rapid tissue growth facilitated a dissection of underlying regulatory mechanisms. We demonstrate how Mphi dynamics, and thus Mphi tissue densities, are locally controlled by CSF-1, a pleiotropic growth factor whose in situ level of activity varied widely between uterine tissue layers. CSF-1 acted in part by inducing Mphi proliferation and in part by stimulating the extravasation of Ly6C(hi) monocytes (Mos) that served as Mphi precursors. Mo recruitment was dependent on the production of CCR2 chemokine receptor ligands by uterine Mphis in response to CSF-1. Unexpectedly, a parallel CSF-1-regulated, but CCR2-independent pathway influenced uterine DC tissue densities by controlling local pre-DC extravasation rates. Together, these data provide cellular and molecular insight into the regulation of Mphi tissue densities under noninflammatory conditions and reveal a central role for CSF-1 in the coordination of Mphi and DC homeostasis.
Lim, A. K., et al (2009). "Antibody blockade of c-fms suppresses the progression of inflammation and injury in early diabetic nephropathy in obese db/db mice" Diabetologia 52(8): 1669-1679.
PubMed
AIMS/HYPOTHESIS: Macrophage-mediated renal injury plays an important role in the development of diabetic nephropathy. Colony-stimulating factor (CSF)-1 is a cytokine that is produced in diabetic kidneys and promotes macrophage accumulation, activation and survival. CSF-1 acts exclusively through the c-fms receptor, which is only expressed on cells of the monocyte-macrophage lineage. Therefore, we used c-fms blockade as a strategy to selectively target macrophage-mediated injury during the progression of diabetic nephropathy. METHODS: Obese, type 2 diabetic db/db BL/KS mice with established albuminuria were treated with a neutralising anti-c-fms monoclonal antibody (AFS98) or isotype matched control IgG from 12 to 18 weeks of age and examined for renal injury. RESULTS: Treatment with AFS98 did not affect obesity, hyperglycaemia, circulating monocyte levels or established albuminuria in db/db mice. However, AFS98 did prevent glomerular hyperfiltration and suppressed variables of inflammation in the diabetic kidney, including kidney macrophages (accumulation, activation and proliferation), chemokine CC motif ligand 2 levels (mRNA and urine protein), kidney activation of proinflammatory pathways (c-Jun amino-terminal kinase and activating transcription factor 2) and Tnf-alpha (also known as Tnf) mRNA levels. In addition, AFS98 decreased the tissue damage caused by macrophages including tubular injury (apoptosis and hypertrophy), interstitial damage (cell proliferation and myofibroblast accrual) and renal fibrosis (Tgf-beta1 [also known as Tgfb1] and Col4a1 mRNA). CONCLUSIONS/INTERPRETATION: Blockade of c-fms can suppress the progression of established diabetic nephropathy in db/db mice by targeting macrophage-mediated injury.
Product Citations
-
-
In vivo experiments
-
Rattus norvegicus (Rat)
Differential regulation of fetal bone marrow and liver hematopoiesis by yolk-sac-derived myeloid cells.
In Nat Commun on 14 May 2025 by Weinhaus, B., Homan, S., et al.
PubMed
Fetal hematopoiesis takes place in the liver before colonizing the bone marrow where it will persist for life. This colonization is thought to be mediated by specification of a microenvironment that selectively recruits hematopoietic cells to the nascent bone marrow. The identity and mechanisms regulating the specification of this colonization niche are unclear. Here we identify a VCAM1+ sinusoidal colonization niche in the diaphysis that regulates neutrophil and hematopoietic stem cell colonization of the bone marrow. Using confocal microscopy, we find that colonizing hematopoietic stem and progenitor cells (HSPC) and myeloid cells selectively localize to a subset of VCAM1+ sinusoids in the center of the diaphysis. Vcam1 deletion in endothelial cells impairs hematopoietic colonization while depletion of yolk-sac-derived osteoclasts disrupts VCAM1+ expression, and impairs neutrophil and HSPC colonization to the bone marrow. Depletion of yolk-sac-derived myeloid cells increases fetal liver hematopoietic stem cell numbers, function and erythropoiesis independent of osteoclast activity. Thus, the yolk sac produces myeloid cells that have opposite roles in fetal hematopoiesis: while yolk-sac derived myeloid cells in the bone marrow promote hematopoietic colonization by specifying a VCAM1+ colonization niche, a different subset of yolk-sac-derived myeloid cells inhibits HSC in the fetal liver.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Immune landscape of oncohistone-mutant gliomas reveals diverse myeloid populations and tumor-promoting function.
In Nat Commun on 5 September 2024 by Andrade, A. F., Annett, A., et al.
PubMed
Histone H3-mutant gliomas are deadly brain tumors characterized by a dysregulated epigenome and stalled differentiation. In contrast to the extensive datasets available on tumor cells, limited information exists on their tumor microenvironment (TME), particularly the immune infiltrate. Here, we characterize the immune TME of H3.3K27M and G34R/V-mutant gliomas, and multiple H3.3K27M mouse models, using transcriptomic, proteomic and spatial single-cell approaches. Resolution of immune lineages indicates high infiltration of H3-mutant gliomas with diverse myeloid populations, high-level expression of immune checkpoint markers, and scarce lymphoid cells, findings uniformly reproduced in all H3.3K27M mouse models tested. We show these myeloid populations communicate with H3-mutant cells, mediating immunosuppression and sustaining tumor formation and maintenance. Dual inhibition of myeloid cells and immune checkpoint pathways show significant therapeutic benefits in pre-clinical syngeneic mouse models. Our findings provide a valuable characterization of the TME of oncohistone-mutant gliomas, and insight into the means for modulating the myeloid infiltrate for the benefit of patients.
-
-
-
Mus musculus (House mouse)
-
Cancer Research
-
Immunology and Microbiology
Immune landscape of oncohistone-mutant gliomas reveals diverse myeloid populations and tumor-promoting function.
In Nature Communications on 5 September 2024 by Andrade, A. F., Annett, A., et al.
Histone H3-mutant gliomas are deadly brain tumors characterized by a dysregulated epigenome and stalled differentiation. In contrast to the extensive datasets available on tumor cells, limited information exists on their tumor microenvironment (TME), particularly the immune infiltrate. Here, we characterize the immune TME of H3.3K27M and G34R/V-mutant gliomas, and multiple H3.3K27M mouse models, using transcriptomic, proteomic and spatial single-cell approaches. Resolution of immune lineages indicates high infiltration of H3-mutant gliomas with diverse myeloid populations, high-level expression of immune checkpoint markers, and scarce lymphoid cells, findings uniformly reproduced in all H3.3K27M mouse models tested. We show these myeloid populations communicate with H3-mutant cells, mediating immunosuppression and sustaining tumor formation and maintenance. Dual inhibition of myeloid cells and immune checkpoint pathways show significant therapeutic benefits in pre-clinical syngeneic mouse models. Our findings provide a valuable characterization of the TME of oncohistone-mutant gliomas, and insight into the means for modulating the myeloid infiltrate for the benefit of patients. © 2024. The Author(s).
-
-
-
Cancer Research
-
Immunology and Microbiology
Lymph node and tumor-associated PD-L1+ macrophages antagonize dendritic cell vaccines by suppressing CD8+ T cells.
In Cell Rep Med on 16 January 2024 by Sprooten, J., Vanmeerbeek, I., et al.
PubMed
Current immunotherapies provide limited benefits against T cell-depleted tumors, calling for therapeutic innovation. Using multi-omics integration of cancer patient data, we predict a type I interferon (IFN) responseHIGH state of dendritic cell (DC) vaccines, with efficacious clinical impact. However, preclinical DC vaccines recapitulating this state by combining immunogenic cancer cell death with induction of type I IFN responses fail to regress mouse tumors lacking T cell infiltrates. Here, in lymph nodes (LNs), instead of activating CD4+/CD8+ T cells, DCs stimulate immunosuppressive programmed death-ligand 1-positive (PD-L1+) LN-associated macrophages (LAMs). Moreover, DC vaccines also stimulate PD-L1+ tumor-associated macrophages (TAMs). This creates two anatomically distinct niches of PD-L1+ macrophages that suppress CD8+ T cells. Accordingly, a combination of PD-L1 blockade with DC vaccines achieves significant tumor regression by depleting PD-L1+ macrophages, suppressing myeloid inflammation, and de-inhibiting effector/stem-like memory T cells. Importantly, clinical DC vaccines also potentiate T cell-suppressive PD-L1+ TAMs in glioblastoma patients. We propose that a multimodal immunotherapy and vaccination regimen is mandatory to overcome T cell-depleted tumors.
-
-
-
Cancer Research
-
Immunology and Microbiology
STING Protein-Based In Situ Vaccine Synergizes CD4+ T, CD8+ T, and NK Cells for Tumor Eradication.
In Adv Healthc Mater on 1 September 2023 by He, Y., Hong, C., et al.
PubMed
Stimulator of interferon genes (STING) signaling is a promising target in cancer immunotherapy, with many ongoing clinical studies in combination with immune checkpoint blockade (ICB). Existing STING-based therapies largely focus on activating CD8+ T cell or NK cell-mediated cytotoxicity, while the role of CD4+ T cells in STING signaling has yet to be extensively studied in vivo. Here, a distinct CD4-mediated, protein-based combination therapy of STING and ICB as an in situ vaccine, is reported. The treatment eliminates subcutaneous MC38 and YUMM1.7 tumors in 70-100% of mice and protected all cured mice against rechallenge. Mechanistic studies reveal a robust TH 1 polarization and suppression of Treg of CD4+ T cells, followed by an effective collaboration of CD4+ T, CD8+ T, and NK cells to eliminate tumors. Finally, the potential to overcome host STING deficiency by significantly decreasing MC38 tumor burden in STING KO mice is demonstrated, addressing the translational challenge for the 19% of human population with loss-of-function STING variants.
-
-
-
Cancer Research
-
Immunology and Microbiology
-
Pharmacology
Pexidartinib synergize PD-1 antibody through inhibiting treg infiltration by reducing TAM-derived CCL22 in lung adenocarcinoma.
In Front Pharmacol on 28 March 2023 by Zhang, W., Jiang, X., et al.
PubMed
There is a crosstalk between Tumor-associated macrophages (TAM) and tumor-infiltrating T cells in tumor environment. TAM could inhibit the activity of cytotoxic T cells; TAM could also regulate the composition of T cells in tumor immune environment. The combination therapy for TAM and tumor infiltrated T cells has been widely noticed, but the crosstalk between TAM and tumor infiltrated T cells remains unclear in the process of combination therapy. We treated lung adenocarcinoma tumor models with pexidartinib, which targets macrophage colony stimulating factor receptor (M-CSFR) and c-kit tyrosine kinase, to inhibited TAM. Pexidartinib inhibited the ratio of macrophages in the tumor and also altered macrophage polarization. In addition to reprogram TAM, pexidartinib also changed the composition of tumor-invasive T cells. After pexidartinib treatment, the total number of T cells, CD8+ T cells and Treg cells were all decreased, the ratio of CD8+T/Treg increased significantly. According to the analysis of cytokines and chemokines during the treatment of pexidartinib, CCL22, as a chemokine for Treg recruitment, significantly decreased after the treatment of pexidartinib. Base on the above observation, the combination of pexidartinib and PD-1 antibody were used in the treatment of lung adenocarcinoma subcutaneous tumor model, the combination therapy has significantly improved the efficacy of tumor treatment compared with the monotherapy. Meanwhile, compared with pexidartinib monotherapy, the combination treatment further switches the polarization status of tumor-associated macrophages. In summary, our results showed that the combination of pexidartinib and PD-1 antibody showed a synergy and significantly improved the anti-tumor efficacy, through pexidartinib increasing CD8T/Treg ratio by reducing TAM-derived CCL22.
-
-
-
Mus musculus (Mouse)
-
Stem Cells and Developmental Biology
Testicular macrophages are recruited during a narrow fetal time window and promote organ-specific developmental functions.
In Nat Commun on 15 March 2023 by Gu, X. W., Heinrich, A., et al.
PubMed
A growing body of evidence demonstrates that fetal-derived tissue-resident macrophages have developmental functions. It has been proposed that macrophages promote testicular functions, but which macrophage populations are involved is unclear. Previous studies showed that macrophages play critical roles in fetal testis morphogenesis and described two adult testicular macrophage populations, interstitial and peritubular. There has been debate regarding the hematopoietic origins of testicular macrophages and whether distinct macrophage populations promote specific testicular functions. Here our hematopoietic lineage-tracing studies in mice show that yolk-sac-derived macrophages comprise the earliest testicular macrophages, while fetal hematopoietic stem cells (HSCs) generate monocytes that colonize the gonad during a narrow time window in a Sertoli-cell-dependent manner and differentiate into adult testicular macrophages. Finally, we show that yolk-sac-derived versus HSC-derived macrophages have distinct functions during testis morphogenesis, while interstitial macrophages specifically promote adult Leydig cell steroidogenesis. Our findings provide insight into testicular macrophage origins and their tissue-specific roles.
-
-
-
Cancer Research
Inhibition of HCK in myeloid cells restricts pancreatic tumor growth and metastasis.
In Cell Rep on 11 October 2022 by Poh, A. R., O'Brien, M., et al.
PubMed
Pancreatic ductal adenocarcinoma (PDAC) is an aggressive disease with a low 5-year survival rate and is associated with poor response to therapy. Elevated expression of the myeloid-specific hematopoietic cell kinase (HCK) is observed in PDAC and correlates with reduced patient survival. To determine whether aberrant HCK signaling in myeloid cells is involved in PDAC growth and metastasis, we established orthotopic and intrasplenic PDAC tumors in wild-type and HCK knockout mice. Genetic ablation of HCK impaired PDAC growth and metastasis by inducing an immune-stimulatory endotype in myeloid cells, which in turn reduced the desmoplastic microenvironment and enhanced cytotoxic effector cell infiltration. Consequently, genetic ablation or therapeutic inhibition of HCK minimized metastatic spread, enhanced the efficacy of chemotherapy, and overcame resistance to anti-PD1, anti-CTLA4, or stimulatory anti-CD40 immunotherapy. Our results provide strong rationale for HCK to be developed as a therapeutic target to improve the response of PDAC to chemo- and immunotherapy.
-
-
-
Cancer Research
-
Immunology and Microbiology
Lactate increases stemness of CD8 + T cells to augment anti-tumor immunity.
In Nat Commun on 6 September 2022 by Feng, Q., Liu, Z., et al.
PubMed
Lactate is a key metabolite produced from glycolytic metabolism of glucose molecules, yet it also serves as a primary carbon fuel source for many cell types. In the tumor-immune microenvironment, effect of lactate on cancer and immune cells can be highly complex and hard to decipher, which is further confounded by acidic protons, a co-product of glycolysis. Here we show that lactate is able to increase stemness of CD8+ T cells and augments anti-tumor immunity. Subcutaneous administration of sodium lactate but not glucose to mice bearing transplanted MC38 tumors results in CD8+ T cell-dependent tumor growth inhibition. Single cell transcriptomics analysis reveals increased proportion of stem-like TCF-1-expressing CD8+ T cells among intra-tumoral CD3+ cells, a phenotype validated by in vitro lactate treatment of T cells. Mechanistically, lactate inhibits histone deacetylase activity, which results in increased acetylation at H3K27 of the Tcf7 super enhancer locus, leading to increased Tcf7 gene expression. CD8+ T cells in vitro pre-treated with lactate efficiently inhibit tumor growth upon adoptive transfer to tumor-bearing mice. Our results provide evidence for an intrinsic role of lactate in anti-tumor immunity independent of the pH-dependent effect of lactic acid, and might advance cancer immune therapy.
-
-
-
Cancer Research
-
Immunology and Microbiology
Therapeutic inhibition of the SRC-kinase HCK facilitates T cell tumor infiltration and improves response to immunotherapy.
In Sci Adv on 24 June 2022 by Poh, A. R., Love, C. G., et al.
PubMed
Although immunotherapy has revolutionized cancer treatment, many immunogenic tumors remain refractory to treatment. This can be largely attributed to an immunologically "cold" tumor microenvironment characterized by an accumulation of immunosuppressive myeloid cells and exclusion of activated T cells. Here, we demonstrate that genetic ablation or therapeutic inhibition of the myeloid-specific hematopoietic cell kinase (HCK) enables activity of antagonistic anti-programmed cell death protein 1 (anti-PD1), anti-CTLA4, or agonistic anti-CD40 immunotherapies in otherwise refractory tumors and augments response in treatment-susceptible tumors. Mechanistically, HCK ablation reprograms tumor-associated macrophages and dendritic cells toward an inflammatory endotype and enhances CD8+ T cell recruitment and activation when combined with immunotherapy in mice. Meanwhile, therapeutic inhibition of HCK in humanized mice engrafted with patient-derived xenografts counteracts tumor immunosuppression, improves T cell recruitment, and impairs tumor growth. Collectively, our results suggest that therapeutic targeting of HCK activity enhances response to immunotherapy by simultaneously stimulating immune cell activation and inhibiting the immunosuppressive tumor microenvironment.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
CD95/Fas protects triple negative breast cancer from anti-tumor activity of NK cells.
In iScience on 19 November 2021 by Qadir, A. S., Guégan, J. P., et al.
PubMed
The apoptosis inducing receptor CD95/Fas has multiple tumorigenic activities. In different genetically engineered mouse models tumor-expressed CD95 was shown to be critical for cell growth. Using a combination of immune-deficient and immune-competent mouse models, we now establish that loss of CD95 in metastatic triple negative breast cancer (TNBC) cells prevents tumor growth by modulating the immune landscape. CD95-deficient, but not wild-type, tumors barely grow in an immune-competent environment and show an increase in immune infiltrates into the tumor. This growth reduction is caused by infiltrating NK cells and does not involve T cells or macrophages. In contrast, in immune compromised mice CD95 k.o. cells are not growth inhibited, but they fail to form metastases. In summary, we demonstrate that in addition to its tumor and metastasis promoting activities, CD95 expression by tumor cells can exert immune suppressive activities on NK cells, providing a new target for immune therapy.
-
-
Targeting the CSF1/CSF1R axis is a potential treatment strategy for malignant meningiomas.
In Neuro Oncol on 2 November 2021 by Yeung, J., Yaghoobi, V., et al.
PubMed
Malignant meningiomas are fatal and lack effective therapy. As M2 macrophages are the most prevalent immune cell type in human meningiomas, we hypothesized that normalizing this immunosuppressive population would be an effective treatment strategy.
-
-
Cardiovascular biology
-
Immunology and Microbiology
-
Mus musculus (Mouse)
PDGF-D activation by macrophage-derived uPA promotes AngII-induced cardiac remodeling in obese mice.
In J Exp Med on 6 September 2021 by Cheng, Y. W., Zhang, Z. B., et al.
PubMed
Obesity-induced secretory disorder of adipose tissue-derived factors is important for cardiac damage. However, whether platelet-derived growth factor-D (PDGF-D), a newly identified adipokine, regulates cardiac remodeling in angiotensin II (AngII)-infused obese mice is unclear. Here, we found obesity induced PDGF-D expression in adipose tissue as well as more severe cardiac remodeling compared with control lean mice after AngII infusion. Adipocyte-specific PDGF-D knockout attenuated hypertensive cardiac remodeling in obese mice. Consistently, adipocyte-specific PDGF-D overexpression transgenic mice (PA-Tg) showed exacerbated cardiac remodeling after AngII infusion without high-fat diet treatment. Mechanistic studies indicated that AngII-stimulated macrophages produce urokinase plasminogen activator (uPA) that activates PDGF-D by splicing full-length PDGF-D into the active PDGF-DD. Moreover, bone marrow-specific uPA knockdown decreased active PDGF-DD levels in the heart and improved cardiac remodeling in HFD hypertensive mice. Together, our data provide for the first time a new interaction pattern between macrophage and adipocyte: that macrophage-derived uPA activates adipocyte-secreted PDGF-D, which finally accelerates AngII-induced cardiac remodeling in obese mice.
-
-
-
Mus musculus (Mouse)
p38 MAPK signaling in M1 macrophages results in selective elimination of M2 macrophages by MEK inhibition.
In J Immunother Cancer on 1 July 2021 by Baumann, D., Drebant, J., et al.
PubMed
M2 macrophages promote tumor progression and therapy resistance, whereas proimmunogenic M1 macrophages can contribute to the efficacy of cytostatic and immunotherapeutic strategies. The abundance of M2 macrophages in the immune infiltrate of many cancer types has prompted the search for strategies to target and eliminate this subset. From our prior experiments in syngeneic mouse tumor models, we learned that pharmacological inhibition of mitogen-activated protein kinase kinase (MEK) did not merely result in tumor cell death, but also in the modulation of the tumor immune infiltrate. This included a prominent decrease in the numbers of macrophages as well as an increase in the M1/M2 macrophage ratio. Investigation of the mechanism underlying this finding in primary murine macrophage cultures revealed that M2 macrophages are significantly more sensitive to MEK inhibition-induced cell death than their M1 counterparts. Further analyses showed that the p38 MAPK pathway, which is activated in M1 macrophages only, renders these cells resistant to death by MEK inhibition. In conclusion, the dependency of M2 macrophages on the MEK/extracellular-signal regulated kinase (ERK) pathway empowers MEK inhibitors to selectively eliminate this subset from the tumor microenvironment.
-
-
-
Mus musculus (Mouse)
-
Biochemistry and Molecular biology
-
Genetics
-
Immunology and Microbiology
Glioblastomas acquire myeloid-affiliated transcriptional programs via epigenetic immunoediting to elicit immune evasion.
In Cell on 29 April 2021 by Gangoso, E., Southgate, B., et al.
PubMed
Glioblastoma multiforme (GBM) is an aggressive brain tumor for which current immunotherapy approaches have been unsuccessful. Here, we explore the mechanisms underlying immune evasion in GBM. By serially transplanting GBM stem cells (GSCs) into immunocompetent hosts, we uncover an acquired capability of GSCs to escape immune clearance by establishing an enhanced immunosuppressive tumor microenvironment. Mechanistically, this is not elicited via genetic selection of tumor subclones, but through an epigenetic immunoediting process wherein stable transcriptional and epigenetic changes in GSCs are enforced following immune attack. These changes launch a myeloid-affiliated transcriptional program, which leads to increased recruitment of tumor-associated macrophages. Furthermore, we identify similar epigenetic and transcriptional signatures in human mesenchymal subtype GSCs. We conclude that epigenetic immunoediting may drive an acquired immune evasion program in the most aggressive mesenchymal GBM subtype by reshaping the tumor immune microenvironment.
-
-
-
Endocrinology and Physiology
-
Immunology and Microbiology
-
Mus musculus (Mouse)
Neutrophil-Macrophage Imbalance Drives the Development of Renal Scarring during Experimental Pyelonephritis.
In J Am Soc Nephrol on 1 January 2021 by Ruíz-Rosado, J. D., Robledo-Avila, F., et al.
PubMed
In children, the acute pyelonephritis that can result from urinary tract infections (UTIs), which commonly ascend from the bladder to the kidney, is a growing concern because it poses a risk of renal scarring and irreversible loss of kidney function. To date, the cellular mechanisms underlying acute pyelonephritis-driven renal scarring remain unknown.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
Tissue-Resident Macrophages in Pancreatic Ductal Adenocarcinoma Originate from Embryonic Hematopoiesis and Promote Tumor Progression.
In Immunity on 15 August 2017 by Zhu, Y., Herndon, J. M., et al.
PubMed
Tumor-associated macrophages (TAMs) are essential components of the cancer microenvironment and play critical roles in the regulation of tumor progression. Optimal therapeutic intervention requires in-depth understanding of the sources that sustain macrophages in malignant tissues. In this study, we investigated the ontogeny of TAMs in murine pancreatic ductal adenocarcinoma (PDAC) models. We identified both inflammatory monocytes and tissue-resident macrophages as sources of TAMs. Unexpectedly, significant portions of pancreas-resident macrophages originated from embryonic development and expanded through in situ proliferation during tumor progression. Whereas monocyte-derived TAMs played more potent roles in antigen presentation, embryonically derived TAMs exhibited a pro-fibrotic transcriptional profile, indicative of their role in producing and remodeling molecules in the extracellular matrix. Collectively, these findings uncover the heterogeneity of TAM origin and functions and could provide therapeutic insight for PDAC treatment.
-