InVivoMAb anti-mouse PD-1 (CD279)
Product Details
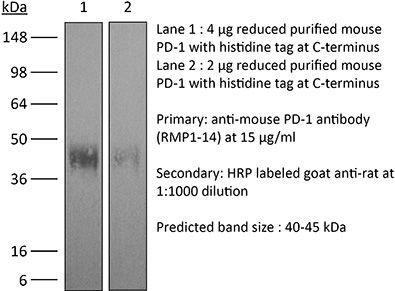
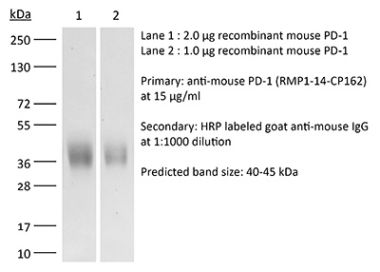
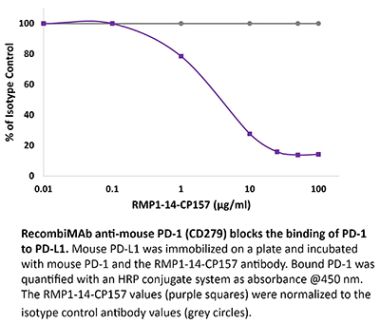
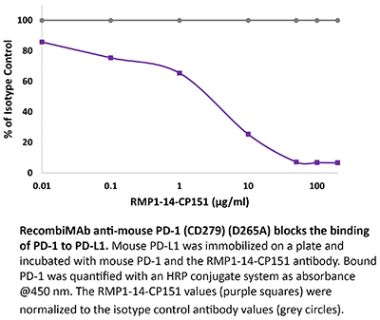
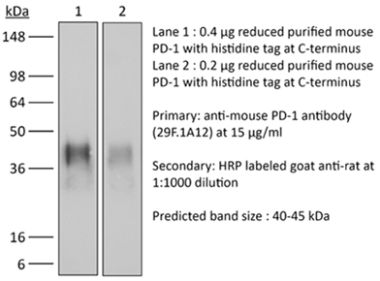
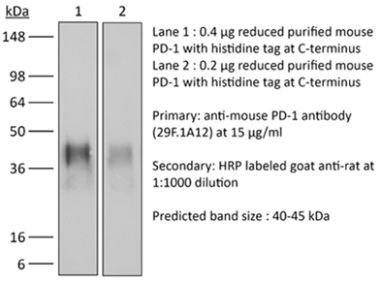
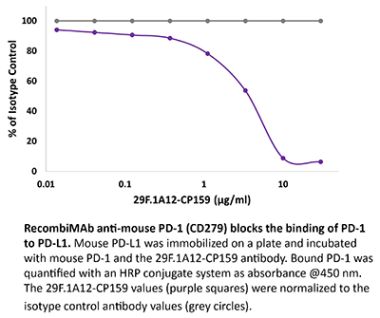
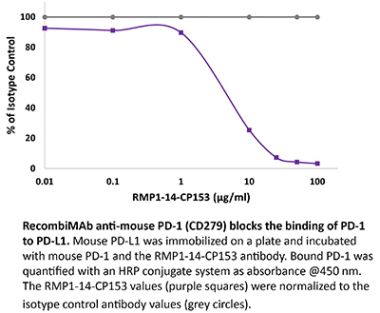
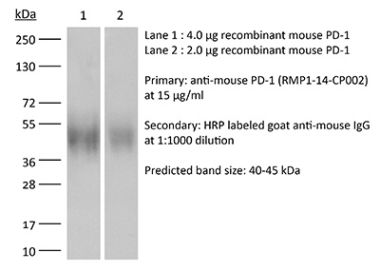
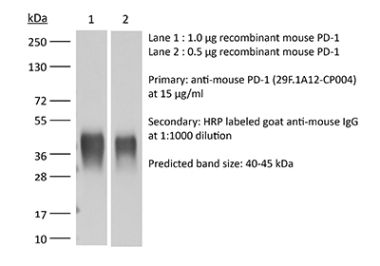
The RMP1-14 monoclonal antibody reacts with mouse PD-1 (programmed death-1) also known as CD279. PD-1 is a 50-55 kDa cell surface receptor encoded by the Pdcd1 gene that belongs to the CD28 family of the Ig superfamily. PD-1 is transiently expressed on CD4 and CD8 thymocytes as well as activated T and B lymphocytes and myeloid cells. PD-1 expression declines after successful elimination of antigen. Additionally, Pdcd1 mRNA is expressed in developing B lymphocytes during the pro-B-cell stage. PD-1’s structure includes a ITIM (immunoreceptor tyrosine-based inhibitory motif) suggesting that PD-1 negatively regulates TCR signals. PD-1 signals via binding its two ligands, PD-L1 and PD-L2 both members of the B7 family. Upon ligand binding, PD-1 signaling inhibits T-cell activation, leading to reduced proliferation, cytokine production, and T-cell death. Additionally, PD-1 is known to play key roles in peripheral tolerance and prevention of autoimmune disease in mice as PD-1 knockout animals show dilated cardiomyopathy, splenomegaly, and loss of peripheral tolerance. Induced PD-L1 expression is common in many tumors including squamous cell carcinoma, colon adenocarcinoma, and breast adenocarcinoma. PD-L1 overexpression results in increased resistance of tumor cells to CD8 T cell mediated lysis. In mouse models of melanoma, tumor growth can be transiently arrested via treatment with antibodies which block the interaction between PD-L1 and its receptor PD-1. For these reasons anti-PD-1 mediated immunotherapies are currently being explored as cancer treatments. Like the J43 antibody the RMP1-14 antibody has been shown to block the binding of both mouse PD-L1-Ig and mouse PD-L2-Ig to PD-1.Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Syrian Hamster BKH cells transfected with mouse PD-1 cDNA |
| Reported Applications | in vivo blocking of PD-1/PD-L signaling |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
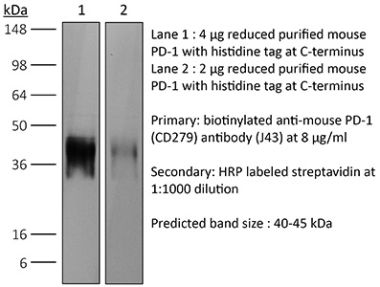
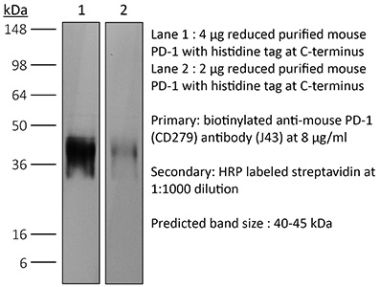
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10949053 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
in vivo blocking of PD-1/PD-L signaling
Triplett, T. A., et al. (2018). "Reversal of indoleamine 2,3-dioxygenase-mediated cancer immune suppression by systemic kynurenine depletion with a therapeutic enzyme" Nat Biotechnol 36(8): 758-764. PubMed
Increased tryptophan (Trp) catabolism in the tumor microenvironment (TME) can mediate immune suppression by upregulation of interferon (IFN)-gamma-inducible indoleamine 2,3-dioxygenase (IDO1) and/or ectopic expression of the predominantly liver-restricted enzyme tryptophan 2,3-dioxygenase (TDO). Whether these effects are due to Trp depletion in the TME or mediated by the accumulation of the IDO1 and/or TDO (hereafter referred to as IDO1/TDO) product kynurenine (Kyn) remains controversial. Here we show that administration of a pharmacologically optimized enzyme (PEGylated kynureninase; hereafter referred to as PEG-KYNase) that degrades Kyn into immunologically inert, nontoxic and readily cleared metabolites inhibits tumor growth. Enzyme treatment was associated with a marked increase in the tumor infiltration and proliferation of polyfunctional CD8(+) lymphocytes. We show that PEG-KYNase administration had substantial therapeutic effects when combined with approved checkpoint inhibitors or with a cancer vaccine for the treatment of large B16-F10 melanoma, 4T1 breast carcinoma or CT26 colon carcinoma tumors. PEG-KYNase mediated prolonged depletion of Kyn in the TME and reversed the modulatory effects of IDO1/TDO upregulation in the TME.
in vivo blocking of PD-1/PD-L signaling
Grasselly, C., et al. (2018). "The Antitumor Activity of Combinations of Cytotoxic Chemotherapy and Immune Checkpoint Inhibitors Is Model-Dependent" Front Immunol 9: 2100. PubMed
In spite of impressive response rates in multiple cancer types, immune checkpoint inhibitors (ICIs) are active in only a minority of patients. Alternative strategies currently aim to combine immunotherapies with conventional agents such as cytotoxic chemotherapies. Here, we performed a study of PD-1 or PDL-1 blockade in combination with reference chemotherapies in four fully immunocompetent mouse models of cancer. We analyzed both the in vivo antitumor response, and the tumor immune infiltrate 4 days after the first treatment. in vivo tumor growth experiments revealed variable responsiveness to ICIs between models. We observed enhanced antitumor effects of the combination of immunotherapy with chemotherapy in the MC38 colon and MB49 bladder models, a lack of response in the 4T1 breast model, and an inhibition of ICIs activity in the MBT-2 bladder model. Flow cytometry analysis of tumor samples showed significant differences in all models between untreated and treated mice. At baseline, all the tumor models studied were predominantly infiltrated with cells harboring an immunosuppressive phenotype. Early alterations of the tumor immune infiltrate after treatment were found to be highly variable. We found that the balance between effector cells and immunosuppressive cells in the tumor microenvironment could be altered with some treatment combinations, but this effect was not always correlated with an impact on in vivo tumor growth. These results show that the combination of cytotoxic chemotherapy with ICIs may result in enhanced, similar or reduced antitumor activity, in a model- and regimen-dependent fashion. The present investigations should help to select appropriate combination regimens for ICIs.
in vivo blocking of PD-1/PD-L signaling
Moynihan, K. D., et al. (2016). "Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses" Nat Med. doi : 10.1038/nm.4200. PubMed
Checkpoint blockade with antibodies specific for cytotoxic T lymphocyte-associated protein (CTLA)-4 or programmed cell death 1 (PDCD1; also known as PD-1) elicits durable tumor regression in metastatic cancer, but these dramatic responses are confined to a minority of patients. This suboptimal outcome is probably due in part to the complex network of immunosuppressive pathways present in advanced tumors, which are unlikely to be overcome by intervention at a single signaling checkpoint. Here we describe a combination immunotherapy that recruits a variety of innate and adaptive immune cells to eliminate large tumor burdens in syngeneic tumor models and a genetically engineered mouse model of melanoma; to our knowledge tumors of this size have not previously been curable by treatments relying on endogenous immunity. Maximal antitumor efficacy required four components: a tumor-antigen-targeting antibody, a recombinant interleukin-2 with an extended half-life, anti-PD-1 and a powerful T cell vaccine. Depletion experiments revealed that CD8+ T cells, cross-presenting dendritic cells and several other innate immune cell subsets were required for tumor regression. Effective treatment induced infiltration of immune cells and production of inflammatory cytokines in the tumor, enhanced antibody-mediated tumor antigen uptake and promoted antigen spreading. These results demonstrate the capacity of an elicited endogenous immune response to destroy large, established tumors and elucidate essential characteristics of combination immunotherapies that are capable of curing a majority of tumors in experimental settings typically viewed as intractable.
in vivo blocking of PD-1/PD-L signaling
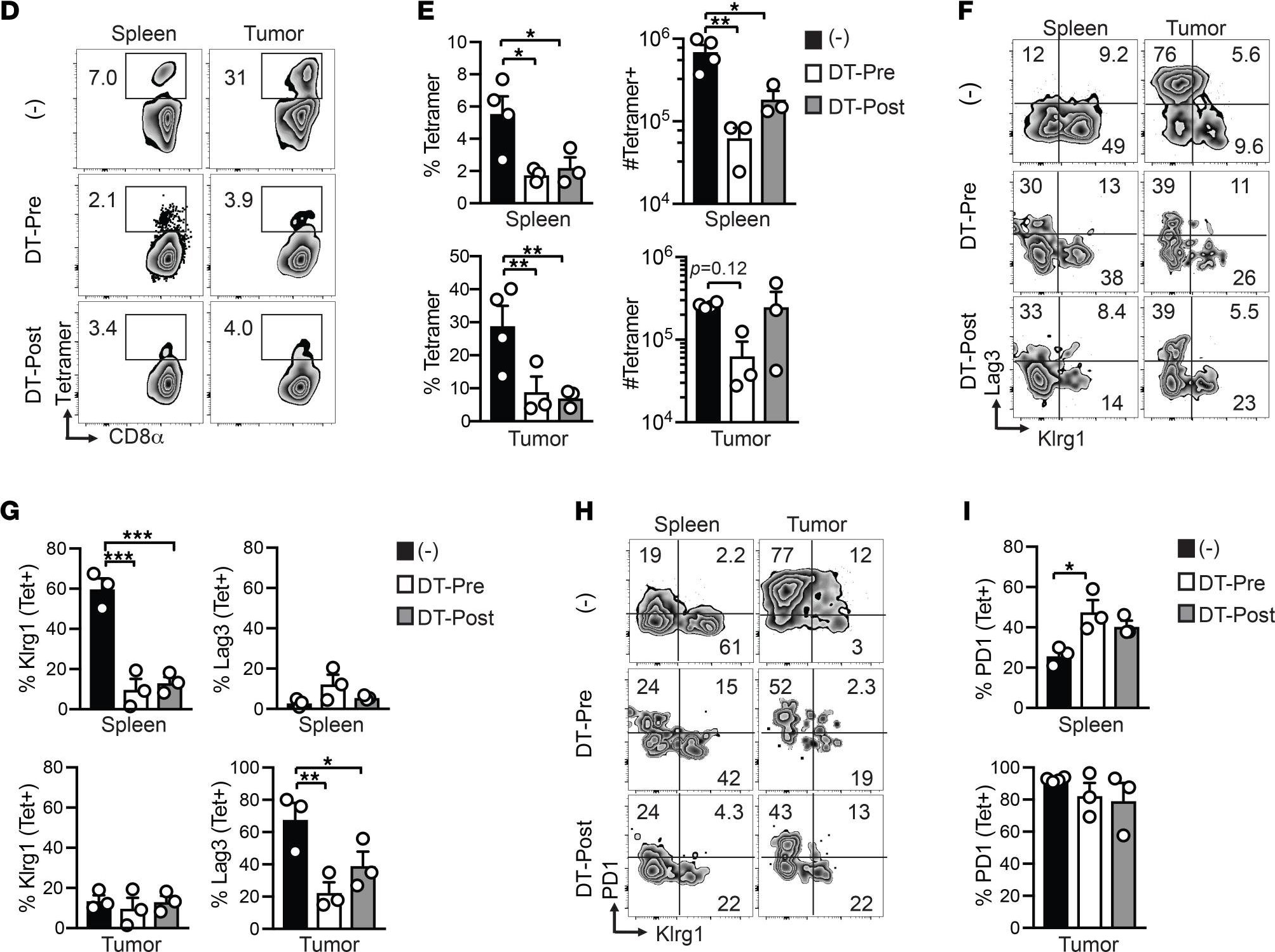
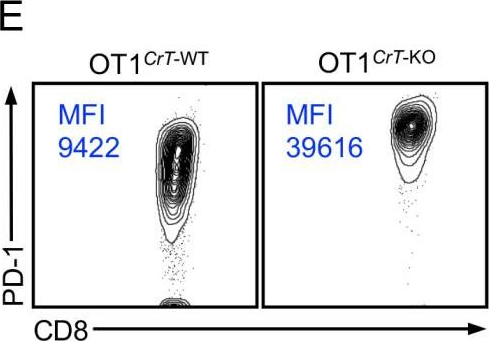
Ngiow, S. F., et al. (2015). "A Threshold Level of Intratumor CD8+ T-cell PD1 Expression Dictates Therapeutic Response to Anti-PD1" Cancer Res 75(18): 3800-3811. PubMed
Despite successes, thus far, a significant proportion of the patients treated with anti-PD1 antibodies have failed to respond. We use mouse tumor models of anti-PD1 sensitivity and resistance and flow cytometry to assess tumor-infiltrating immune cells immediately after therapy. We demonstrate that the expression levels of T-cell PD1 (PD1(lo)), myeloid, and T-cell PDL1 (PDL1(hi)) in the tumor microenvironment inversely correlate and dictate the efficacy of anti-PD1 mAb and function of intratumor CD8(+) T cells. In sensitive tumors, we reveal a threshold for PD1 downregulation on tumor-infiltrating CD8(+) T cells below which the release of adaptive immune resistance is achieved. In contrast, PD1(hi) T cells in resistant tumors fail to be rescued by anti-PD1 therapy and remain dysfunctional unless intratumor PDL1(lo) immune cells are targeted. Intratumor Tregs are partly responsible for the development of anti-PD1-resistant tumors and PD1(hi) CD8(+) T cells. Our analyses provide a framework to interrogate intratumor CD8(+) T-cell PD1 and immune PDL1 levels and response in human cancer. Cancer Res; 75(18); 3800-11. (c)2015 AACR.
in vivo blocking of PD-1/PD-L signaling
Evans, E. E., et al. (2015). "Antibody Blockade of Semaphorin 4D Promotes Immune Infiltration into Tumor and Enhances Response to Other Immunomodulatory Therapies" Cancer Immunol Res 3(6): 689-701. PubMed
Semaphorin 4D (SEMA4D, CD100) and its receptor plexin-B1 (PLXNB1) are broadly expressed in murine and human tumors, and their expression has been shown to correlate with invasive disease in several human tumors. SEMA4D normally functions to regulate the motility and differentiation of multiple cell types, including those of the immune, vascular, and nervous systems. In the setting of cancer, SEMA4D-PLXNB1 interactions have been reported to affect vascular stabilization and transactivation of ERBB2, but effects on immune-cell trafficking in the tumor microenvironment (TME) have not been investigated. We describe a novel immunomodulatory function of SEMA4D, whereby strong expression of SEMA4D at the invasive margins of actively growing tumors influences the infiltration and distribution of leukocytes in the TME. Antibody neutralization of SEMA4D disrupts this gradient of expression, enhances recruitment of activated monocytes and lymphocytes into the tumor, and shifts the balance of cells and cytokines toward a proinflammatory and antitumor milieu within the TME. This orchestrated change in the tumor architecture was associated with durable tumor rejection in murine Colon26 and ERBB2(+) mammary carcinoma models. The immunomodulatory activity of anti-SEMA4D antibody can be enhanced by combination with other immunotherapies, including immune checkpoint inhibition and chemotherapy. Strikingly, the combination of anti-SEMA4D antibody with antibody to CTLA-4 acts synergistically to promote complete tumor rejection and survival. Inhibition of SEMA4D represents a novel mechanism and therapeutic strategy to promote functional immune infiltration into the TME and inhibit tumor progression.
in vivo blocking of PD-1/PD-L signaling
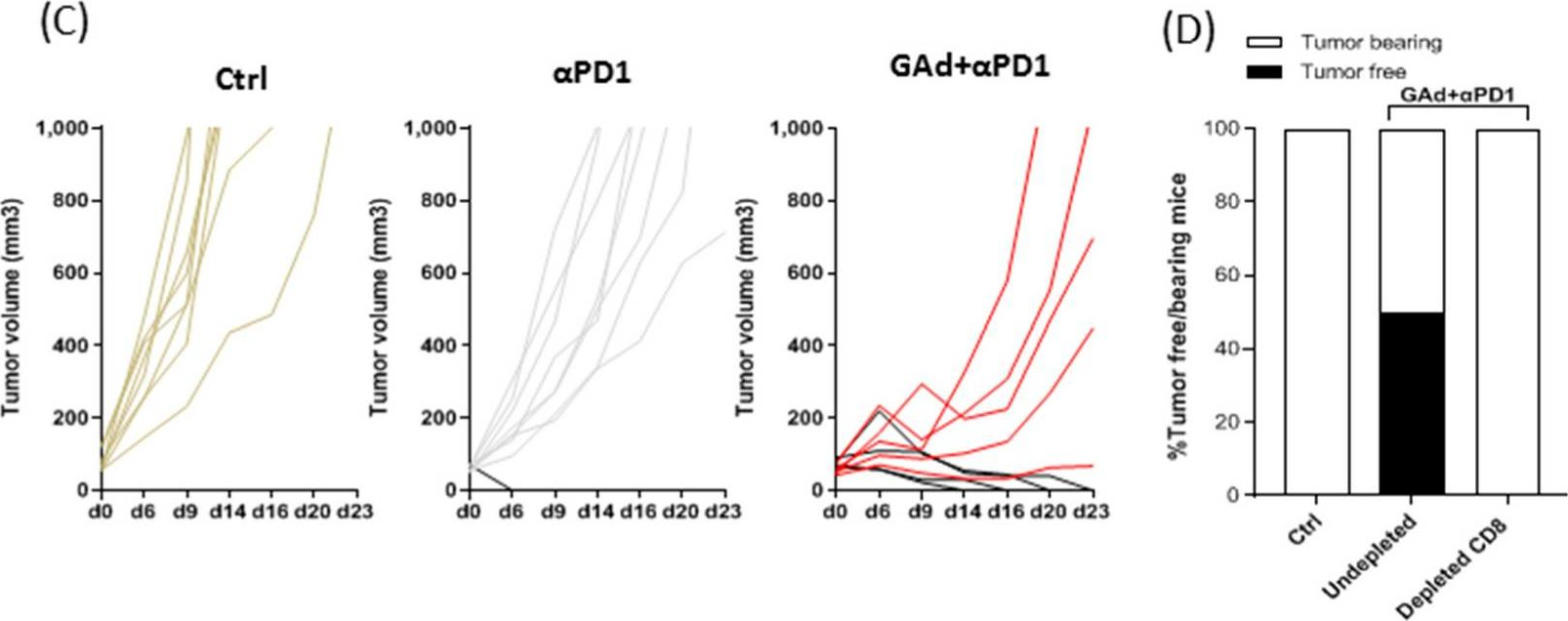
Zelenay, S., et al. (2015). "Cyclooxygenase-Dependent Tumor Growth through Evasion of Immunity" Cell 162(6): 1257-1270. PubMed
The mechanisms by which melanoma and other cancer cells evade anti-tumor immunity remain incompletely understood. Here, we show that the growth of tumors formed by mutant Braf(V600E) mouse melanoma cells in an immunocompetent host requires their production of prostaglandin E2, which suppresses immunity and fuels tumor-promoting inflammation. Genetic ablation of cyclooxygenases (COX) or prostaglandin E synthases in Braf(V600E) mouse melanoma cells, as well as in Nras(G12D) melanoma or in breast or colorectal cancer cells, renders them susceptible to immune control and provokes a shift in the tumor inflammatory profile toward classic anti-cancer immune pathways. This mouse COX-dependent inflammatory signature is remarkably conserved in human cutaneous melanoma biopsies, arguing for COX activity as a driver of immune suppression across species. Pre-clinical data demonstrate that inhibition of COX synergizes with anti-PD-1 blockade in inducing eradication of tumors, implying that COX inhibitors could be useful adjuvants for immune-based therapies in cancer patients.
in vivo blocking of PD-1/PD-L signaling
Zander, R. A., et al. (2015). "PD-1 Co-inhibitory and OX40 Co-stimulatory Crosstalk Regulates Helper T Cell Differentiation and Anti-Plasmodium Humoral Immunity" Cell Host Microbe 17(5): 628-641. PubMed
The differentiation and protective capacity of Plasmodium-specific T cells are regulated by both positive and negative signals during malaria, but the molecular and cellular details remain poorly defined. Here we show that malaria patients and Plasmodium-infected rodents exhibit atypical expression of the co-stimulatory receptor OX40 on CD4 T cells and that therapeutic enhancement of OX40 signaling enhances helper CD4 T cell activity, humoral immunity, and parasite clearance in rodents. However, these beneficial effects of OX40 signaling are abrogated following coordinate blockade of PD-1 co-inhibitory pathways, which are also upregulated during malaria and associated with elevated parasitemia. Co-administration of biologics blocking PD-1 and promoting OX40 signaling induces excessive interferon-gamma that directly limits helper T cell-mediated support of humoral immunity and decreases parasite control. Our results show that targeting OX40 can enhance Plasmodium control and that crosstalk between co-inhibitory and co-stimulatory pathways in pathogen-specific CD4 T cells can impact pathogen clearance.
in vivo blocking of PD-1/PD-L signaling
Twyman-Saint Victor, C., et al. (2015). "Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer" Nature 520(7547): 373-377. PubMed
Immune checkpoint inhibitors result in impressive clinical responses, but optimal results will require combination with each other and other therapies. This raises fundamental questions about mechanisms of non-redundancy and resistance. Here we report major tumour regressions in a subset of patients with metastatic melanoma treated with an anti-CTLA4 antibody (anti-CTLA4) and radiation, and reproduced this effect in mouse models. Although combined treatment improved responses in irradiated and unirradiated tumours, resistance was common. Unbiased analyses of mice revealed that resistance was due to upregulation of PD-L1 on melanoma cells and associated with T-cell exhaustion. Accordingly, optimal response in melanoma and other cancer types requires radiation, anti-CTLA4 and anti-PD-L1/PD-1. Anti-CTLA4 predominantly inhibits T-regulatory cells (Treg cells), thereby increasing the CD8 T-cell to Treg (CD8/Treg) ratio. Radiation enhances the diversity of the T-cell receptor (TCR) repertoire of intratumoral T cells. Together, anti-CTLA4 promotes expansion of T cells, while radiation shapes the TCR repertoire of the expanded peripheral clones. Addition of PD-L1 blockade reverses T-cell exhaustion to mitigate depression in the CD8/Treg ratio and further encourages oligoclonal T-cell expansion. Similarly to results from mice, patients on our clinical trial with melanoma showing high PD-L1 did not respond to radiation plus anti-CTLA4, demonstrated persistent T-cell exhaustion, and rapidly progressed. Thus, PD-L1 on melanoma cells allows tumours to escape anti-CTLA4-based therapy, and the combination of radiation, anti-CTLA4 and anti-PD-L1 promotes response and immunity through distinct mechanisms.
in vivo blocking of PD-1/PD-L signaling
Vanpouille-Box, C., et al. (2015). "TGFbeta Is a Master Regulator of Radiation Therapy-Induced Antitumor Immunity" Cancer Res 75(11): 2232-2242. PubMed
T cells directed to endogenous tumor antigens are powerful mediators of tumor regression. Recent immunotherapy advances have identified effective interventions to unleash tumor-specific T-cell activity in patients who naturally develop them. Eliciting T-cell responses to a patient’s individual tumor remains a major challenge. Radiation therapy can induce immune responses to model antigens expressed by tumors, but it remains unclear whether it can effectively prime T cells specific for endogenous antigens expressed by poorly immunogenic tumors. We hypothesized that TGFbeta activity is a major obstacle hindering the ability of radiation to generate an in situ tumor vaccine. Here, we show that antibody-mediated TGFbeta neutralization during radiation therapy effectively generates CD8(+) T-cell responses to multiple endogenous tumor antigens in poorly immunogenic mouse carcinomas. Generated T cells were effective at causing regression of irradiated tumors and nonirradiated lung metastases or synchronous tumors (abscopal effect). Gene signatures associated with IFNgamma and immune-mediated rejection were detected in tumors treated with radiation therapy and TGFbeta blockade in combination but not as single agents. Upregulation of programmed death (PD) ligand-1 and -2 in neoplastic and myeloid cells and PD-1 on intratumoral T cells limited tumor rejection, resulting in rapid recurrence. Addition of anti-PD-1 antibodies extended survival achieved with radiation and TGFbeta blockade. Thus, TGFbeta is a fundamental regulator of radiation therapy’s ability to generate an in situ tumor vaccine. The combination of local radiation therapy with TGFbeta neutralization offers a novel individualized strategy for vaccinating patients against their tumors.
in vivo blocking of PD-1/PD-L signaling
Mittal, D., et al. (2014). "Antimetastatic effects of blocking PD-1 and the adenosine A2A receptor" Cancer Res 74(14): 3652-3658. PubMed
Adenosine targeting is an attractive new approach to cancer treatment, but no clinical study has yet examined adenosine inhibition in oncology despite the safe clinical profile of adenosine A2A receptor inhibitors (A2ARi) in Parkinson disease. Metastasis is the main cause of cancer-related deaths worldwide, and therefore we have studied experimental and spontaneous mouse models of melanoma and breast cancer metastasis to demonstrate the efficacy and mechanism of a combination of A2ARi in combination with anti-PD-1 monoclonal antibody (mAb). This combination significantly reduces metastatic burden and prolongs the life of mice compared with either monotherapy alone. Importantly, the combination was only effective when the tumor expressed high levels of CD73, suggesting a tumor biomarker that at a minimum could be used to stratify patients that might receive this combination. The mechanism of the combination therapy was critically dependent on NK cells and IFNgamma, and to a lesser extent, CD8(+) T cells and the effector molecule, perforin. Overall, these results provide a strong rationale to use A2ARi with anti-PD-1 mAb for the treatment of minimal residual and metastatic disease.
in vivo blocking of PD-1/PD-L signaling
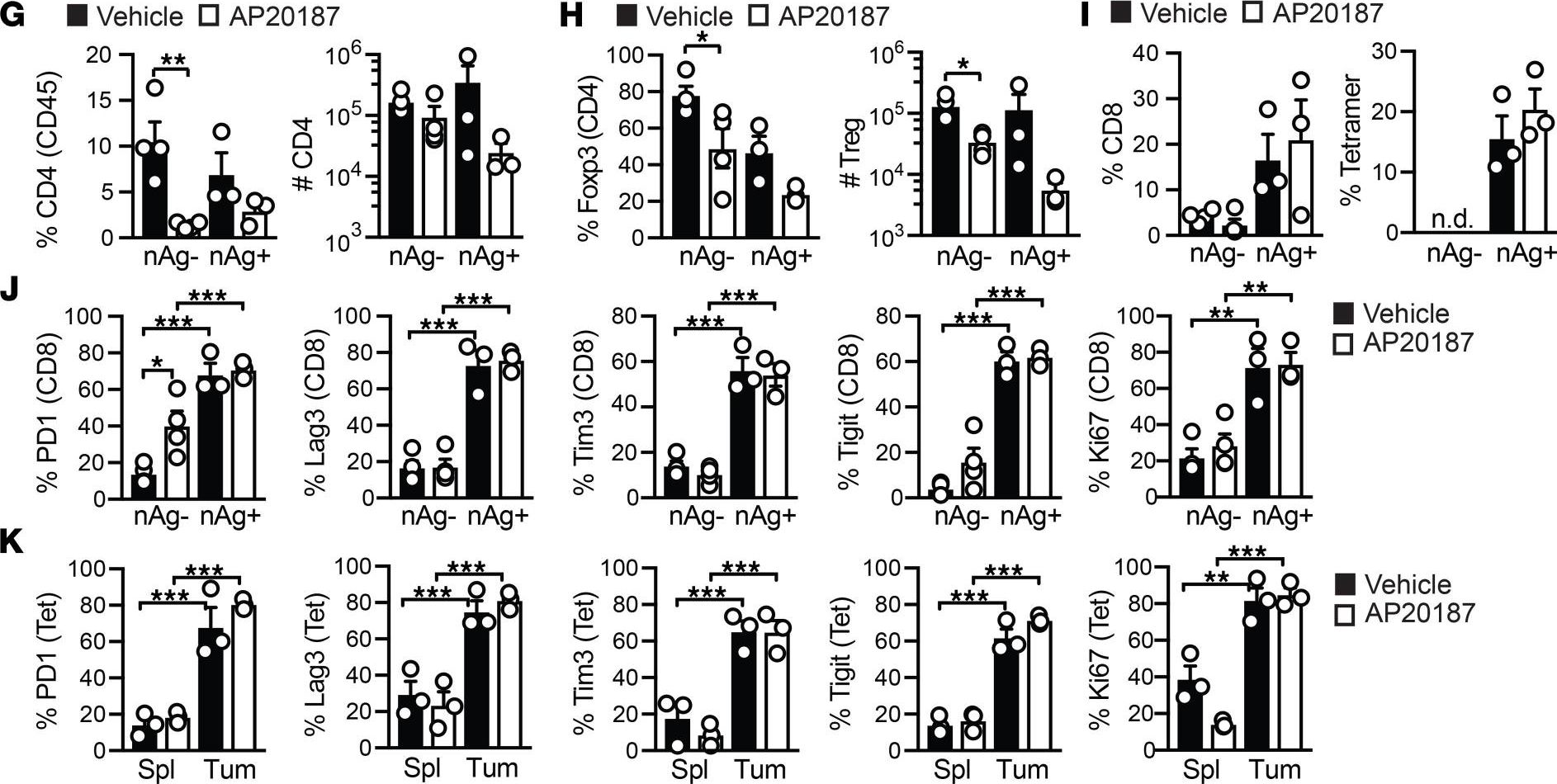
McGray, A. J., et al. (2014). "Immunotherapy-induced CD8+ T cells instigate immune suppression in the tumor" Mol Ther 22(1): 206-218. PubMed
Despite clear evidence of immunogenicity, cancer vaccines only provide a modest clinical benefit. To evaluate the mechanisms that limit tumor regression following vaccination, we have investigated the weak efficacy of a highly immunogenic experimental vaccine using a murine melanoma model. We discovered that the tumor adapts rapidly to the immune attack instigated by tumor-specific CD8+ T cells in the first few days following vaccination, resulting in the upregulation of a complex set of biological networks, including multiple immunosuppressive processes. This rapid adaptation acts to prevent sustained local immune attack, despite continued infiltration by increasing numbers of tumor-specific T cells. Combining vaccination with adoptive transfer of tumor-specific T cells produced complete regression of the treated tumors but did not prevent the adaptive immunosuppression. In fact, the adaptive immunosuppressive pathways were more highly induced in regressing tumors, commensurate with the enhanced level of immune attack. Examination of tumor infiltrating T-cell functionality revealed that the adaptive immunosuppression leads to a progressive loss in T-cell function, even in tumors that are regressing. These novel observations that T cells produced by therapeutic intervention can instigate a rapid adaptive immunosuppressive response within the tumor have important implications for clinical implementation of immunotherapies.
in vivo blocking of PD-1/PD-L signaling
John, L. B., et al. (2013). "Anti-PD-1 antibody therapy potently enhances the eradication of established tumors by gene-modified T cells" Clin Cancer Res 19(20): 5636-5646. PubMed
PURPOSE: To determine the antitumor efficacy and toxicity of a novel combination approach involving adoptive T-cell immunotherapy using chimeric antigen receptor (CAR) T cells with an immunomodulatory reagent for blocking immunosuppression. EXPERIMENTAL DESIGN: We examined whether administration of a PD-1 blocking antibody could increase the therapeutic activity of CAR T cells against two different Her-2(+) tumors. The use of a self-antigen mouse model enabled investigation into the efficacy, mechanism, and toxicity of this combination approach. RESULTS: In this study, we first showed a significant increase in the level of PD-1 expressed on transduced anti-Her-2 CD8(+) T cells following antigen-specific stimulation with PD-L1(+) tumor cells and that markers of activation and proliferation were increased in anti-Her-2 T cells in the presence of anti-PD-1 antibody. In adoptive transfer studies in Her-2 transgenic recipient mice, we showed a significant improvement in growth inhibition of two different Her-2(+) tumors treated with anti-Her-2 T cells in combination with anti-PD-1 antibody. The therapeutic effects observed correlated with increased function of anti-Her-2 T cells following PD-1 blockade. Strikingly, a significant decrease in the percentage of Gr1(+) CD11b(+) myeloid-derived suppressor cells (MDSC) was observed in the tumor microenvironment of mice treated with the combination therapy. Importantly, increased antitumor effects were not associated with any autoimmune pathology in normal tissue expressing Her-2 antigen. CONCLUSION: This study shows that specifically blocking PD-1 immunosuppression can potently enhance CAR T-cell therapy that has significant implications for potentially improving therapeutic outcomes of this approach in patients with cancer.
in vivo blocking of PD-1/PD-L signaling
Holmgaard, R. B., et al. (2013). "Indoleamine 2,3-dioxygenase is a critical resistance mechanism in antitumor T cell immunotherapy targeting CTLA-4" J Exp Med 210(7): 1389-1402. PubMed
The cytotoxic T lymphocyte antigen-4 (CTLA-4)-blocking antibody ipilimumab results in durable responses in metastatic melanoma, though therapeutic benefit has been limited to a fraction of patients. This calls for identification of resistance mechanisms and development of combinatorial strategies. Here, we examine the inhibitory role of indoleamine 2,3-dioxygenase (IDO) on the antitumor efficacy of CTLA-4 blockade. In IDO knockout mice treated with anti-CTLA-4 antibody, we demonstrate a striking delay in B16 melanoma tumor growth and increased overall survival when compared with wild-type mice. This was also observed with antibodies targeting PD-1-PD-L1 and GITR. To highlight the therapeutic relevance of these findings, we show that CTLA-4 blockade strongly synergizes with IDO inhibitors to mediate rejection of both IDO-expressing and nonexpressing poorly immunogenic tumors, emphasizing the importance of the inhibitory role of both tumor- and host-derived IDO. This effect was T cell dependent, leading to enhanced infiltration of tumor-specific effector T cells and a marked increase in the effector-to-regulatory T cell ratios in the tumors. Overall, these data demonstrate the immunosuppressive role of IDO in the context of immunotherapies targeting immune checkpoints and provide a strong incentive to clinically explore combination therapies using IDO inhibitors irrespective of IDO expression by the tumor cells.
in vivo blocking of PD-1/PD-L signaling
van der Werf, N., et al. (2013). "Th2 cell-intrinsic hypo-responsiveness determines susceptibility to helminth infection" PLoS Pathog 9(3): e1003215. PubMed
The suppression of protective Type 2 immunity is a principal factor driving the chronicity of helminth infections, and has been attributed to a range of Th2 cell-extrinsic immune-regulators. However, the intrinsic fate of parasite-specific Th2 cells within a chronic immune down-regulatory environment, and the resultant impact such fate changes may have on host resistance is unknown. We used IL-4gfp reporter mice to demonstrate that during chronic helminth infection with the filarial nematode Litomosoides sigmodontis, CD4(+) Th2 cells are conditioned towards an intrinsically hypo-responsive phenotype, characterised by a loss of functional ability to proliferate and produce the cytokines IL-4, IL-5 and IL-2. Th2 cell hypo-responsiveness was a key element determining susceptibility to L. sigmodontis infection, and could be reversed in vivo by blockade of PD-1 resulting in long-term recovery of Th2 cell functional quality and enhanced resistance. Contrasting with T cell dysfunction in Type 1 settings, the control of Th2 cell hypo-responsiveness by PD-1 was mediated through PD-L2, and not PD-L1. Thus, intrinsic changes in Th2 cell quality leading to a functionally hypo-responsive phenotype play a key role in determining susceptibility to filarial infection, and the therapeutic manipulation of Th2 cell-intrinsic quality provides a potential avenue for promoting resistance to helminths.
in vivo blocking of PD-1/PD-L signaling
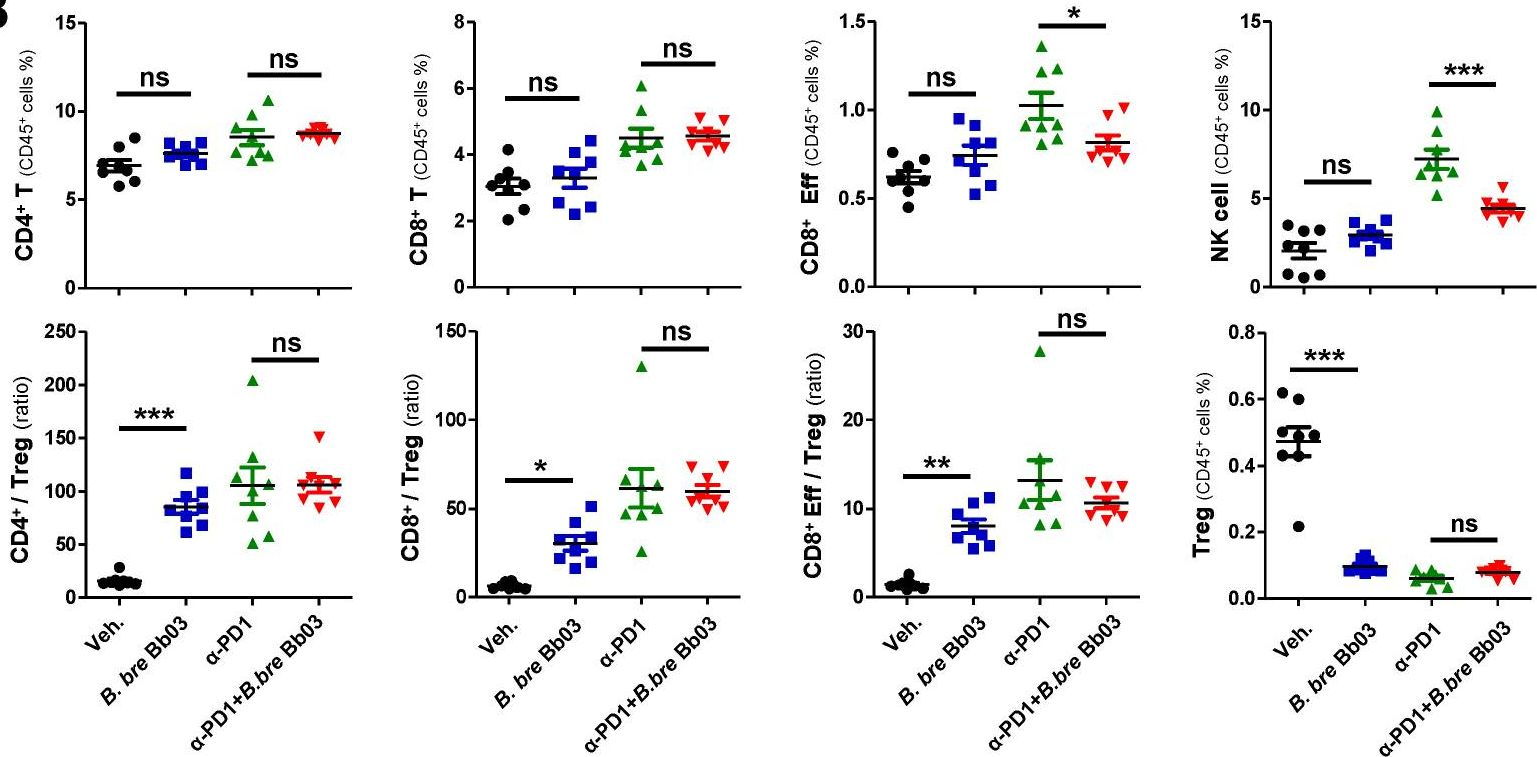
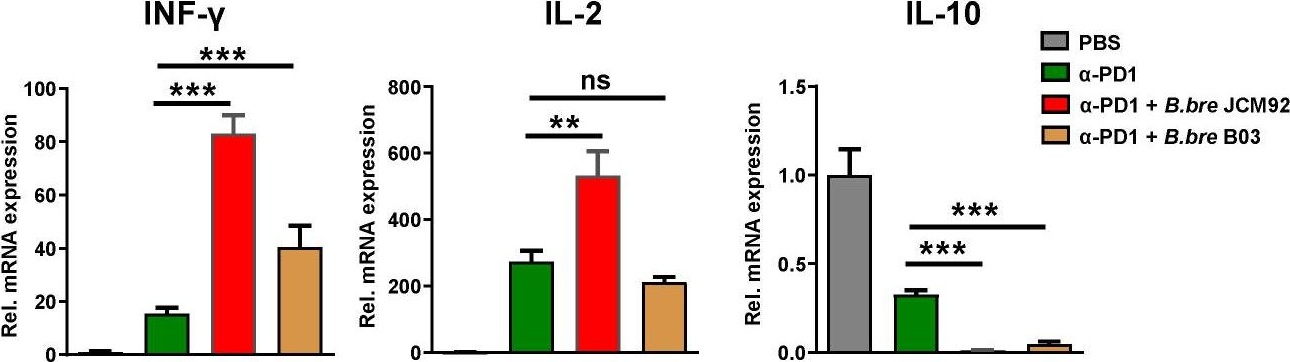
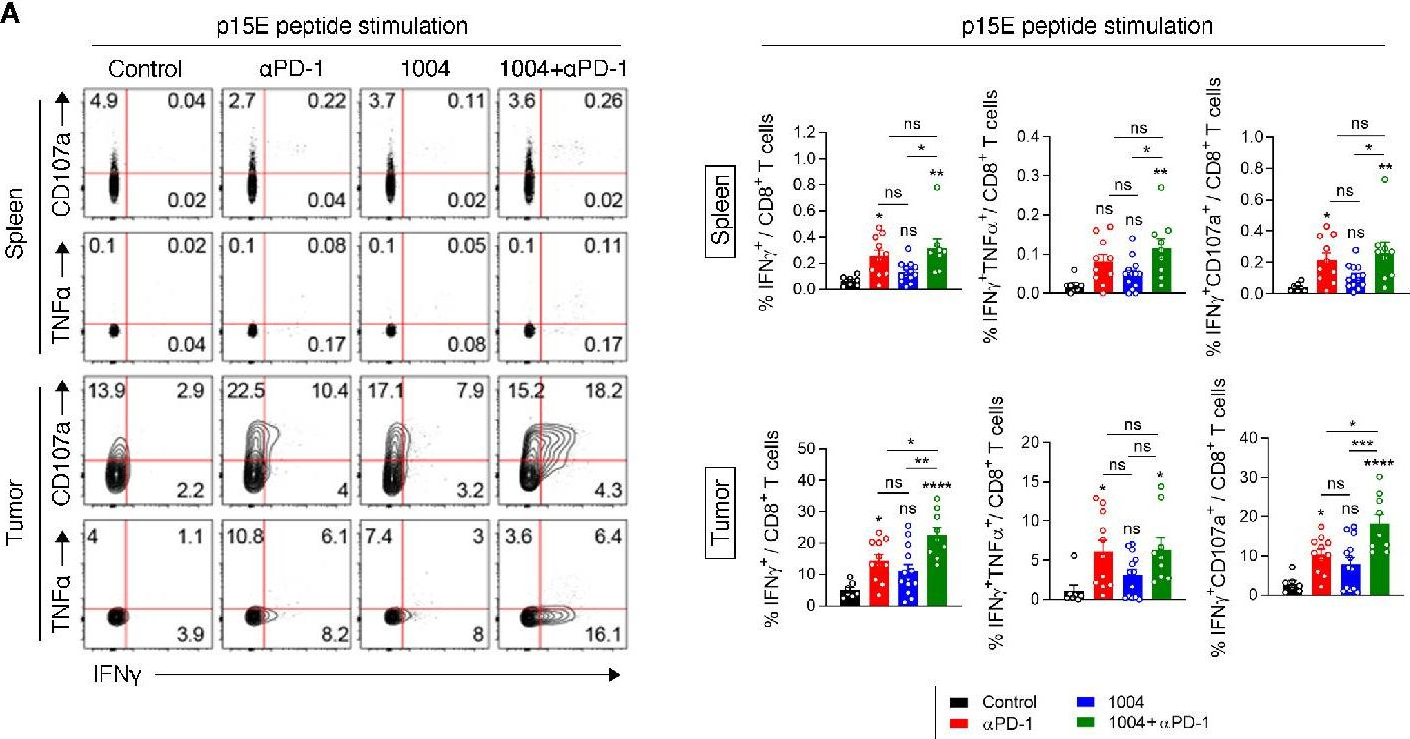
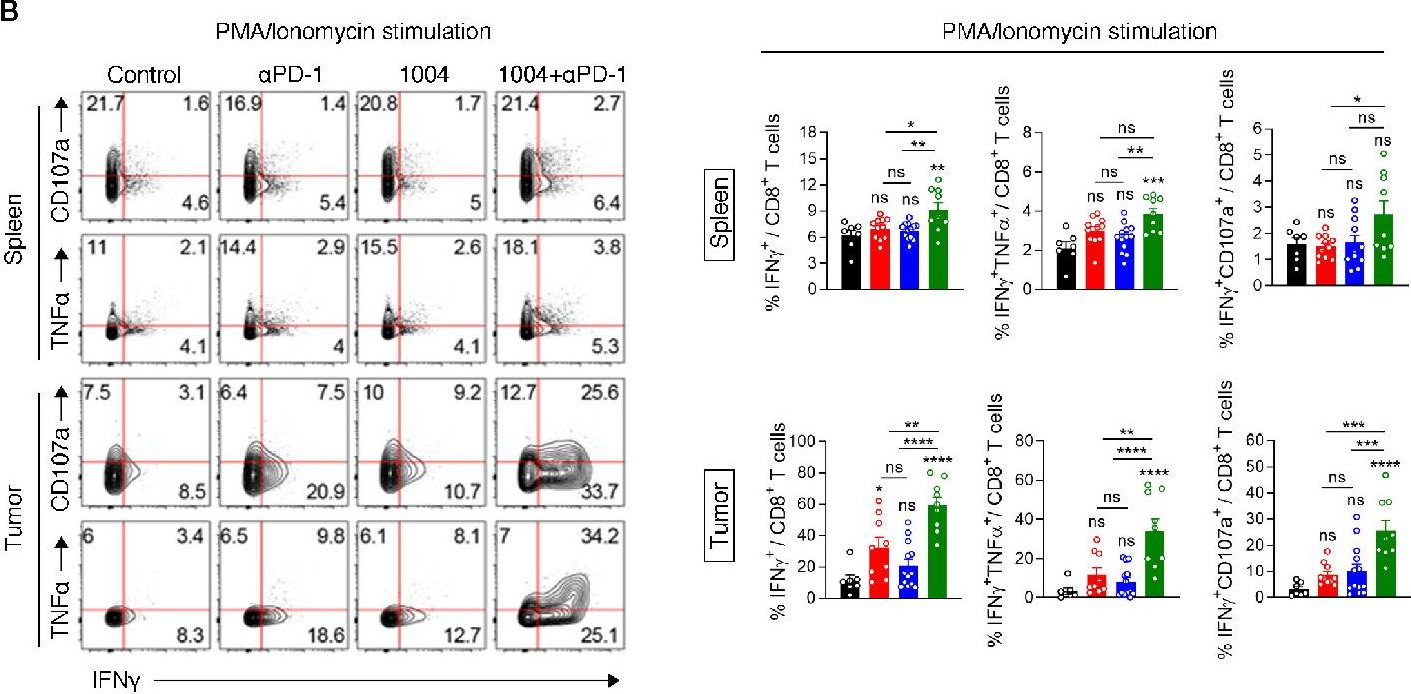
Curran, M. A., et al. (2010). "PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors" Proc Natl Acad Sci U S A 107(9): 4275-4280. PubMed
Vaccination with irradiated B16 melanoma cells expressing either GM-CSF (Gvax) or Flt3-ligand (Fvax) combined with antibody blockade of the negative T-cell costimulatory receptor cytotoxic T-lymphocyte antigen-4 (CTLA-4) promotes rejection of preimplanted tumors. Despite CTLA-4 blockade, T-cell proliferation and cytokine production can be inhibited by the interaction of programmed death-1 (PD-1) with its ligands PD-L1 and PD-L2 or by the interaction of PD-L1 with B7-1. Here, we show that the combination of CTLA-4 and PD-1 blockade is more than twice as effective as either alone in promoting the rejection of B16 melanomas in conjunction with Fvax. Adding alphaPD-L1 to this regimen results in rejection of 65% of preimplanted tumors vs. 10% with CTLA-4 blockade alone. Combination PD-1 and CTLA-4 blockade increases effector T-cell (Teff) infiltration, resulting in highly advantageous Teff-to-regulatory T-cell ratios with the tumor. The fraction of tumor-infiltrating Teffs expressing CTLA-4 and PD-1 increases, reflecting the proliferation and accumulation of cells that would otherwise be anergized. Combination blockade also synergistically increases Teff-to-myeloid-derived suppressor cell ratios within B16 melanomas. IFN-gamma production increases in both the tumor and vaccine draining lymph nodes, as does the frequency of IFN-gamma/TNF-alpha double-producing CD8(+) T cells within the tumor. These results suggest that combination blockade of the PD-1/PD-L1- and CTLA-4-negative costimulatory pathways allows tumor-specific T cells that would otherwise be inactivated to continue to expand and carry out effector functions, thereby shifting the tumor microenvironment from suppressive to inflammatory.

- Cancer Research,
- Immunology and Microbiology
Generation of Orthotopic Patient-Derived Xenograft in Humanized Mice for Evaluation of Emerging Targeted Therapies and Immunotherapy Combinations for Melanoma
Preprint on Preprints.org on 10 July 2023 by Yan, C., Nebhan, C. A., et al.
PubMed
Current methodologies for developing patient-derived xenografts (PDX) in humanized mice in preclinical trials to test response to immune-based therapies are limited by graft versus host disease. Here we compared two approaches for establishing PDX tumors in humanized mice: 1) PDX are first established in immune-deficient mice; 2) PDX are initially established in humanized mice, before transplanting established PDX’s to a larger cohort of humanized mice for preclinical trials. With the first approach, there was rapid wasting of PDX-bearing humanized mice with high levels of activated T cells in the circulation and organs, indicating immune-mediated toxicity. In contrast, with the second approach, toxicity was less of an issue and long-term human melanoma tumor growth and maintenance of human chimerism was achieved. Pre-clinical trials from the second approach revealed that rigosertib, but not anti-PD-1, increased CD8/CD4 T cell ratios in spleen and blood and inhibited PDX tumor growth. Resistance to anti-PD-1 was associated with limited infiltration of CD8+ T cell into the tumor. Our findings suggest that it is essential to carefully manage immune editing by first establishing PDX tumors in the presence of human immune cells before expanding PDX tumors into a larger cohort of humanized mice to evaluate therapy response.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Single-cell analyses reveal cannabidiol rewires tumor microenvironment via inhibiting alternative activation of macrophage and synergizes with anti-PD-1 in colon cancer.
In Journal of Pharmaceutical Analysis on 1 July 2023 by Sun, X., Zhou, L., et al.
PubMed
Colorectal tumors often create an immunosuppressive microenvironment that prevents them from responding to immunotherapy. Cannabidiol (CBD) is a non-psychoactive natural active ingredient from the cannabis plant that has various pharmacological effects, including neuroprotective, antiemetic, anti-inflammatory, and antineoplastic activities. This study aimed to elucidate the specific anticancer mechanism of CBD by single-cell RNA sequencing (scRNA-seq) and single-cell ATAC sequencing (scATAC-seq) technologies. Here, we report that CBD inhibits colorectal cancer progression by modulating the suppressive tumor microenvironment (TME). Our single-cell transcriptome and ATAC sequencing results showed that CBD suppressed M2-like macrophages and promoted M1-like macrophages in tumors both in strength and quantity. Furthermore, CBD significantly enhanced the interaction between M1-like macrophages and tumor cells and restored the intrinsic anti-tumor properties of macrophages, thereby preventing tumor progression. Mechanistically, CBD altered the metabolic pattern of macrophages and related anti-tumor signaling pathways. We found that CBD inhibited the alternative activation of macrophages and shifted the metabolic process from oxidative phosphorylation and fatty acid oxidation to glycolysis by inhibiting the phosphatidylinositol 3-kinase-protein kinase B signaling pathway and related downstream target genes. Furthermore, CBD-mediated macrophage plasticity enhanced the response to anti-programmed cell death protein-1 (PD-1) immunotherapy in xenografted mice. Taken together, we provide new insights into the anti-tumor effects of CBD. © 2023 The Author(s).
- Mus musculus (House mouse),
- Cancer Research
SIRPG expression positively associates with an inflamed tumor microenvironment and response to PD-1 blockade.
In Cancer Immunology, Immunotherapy : CII on 4 June 2024 by Luo, L., Jiang, M., et al.
PubMed
This study aimed to investigate the relationship between signal regulatory protein gamma (SIRPG) and tumor immune microenvironment phenotypes or T cell mediated-adaptive antitumor immunity, and its predictive value for response to PD-1 blockade in cancers. Pan-cancer analysis of SIRPG expression and immune deconvolution was performed using transcriptomic data across 33 tumor types. Transcriptomic and clinical data from 157 patients with non-small-cell lung cancer (NSCLC) and melanoma received PD-1 blockade were analyzed. Expression characteristics of SIRPG were investigated using single-cell RNA sequencing (scRNA-seq) data of 103,599 cells. The effect of SIRPG expression was evaluated via SIRPG knockdown or overexpression in Jurkat T cells. The results showed that most cancers with high SIRPG expression had significantly higher abundance of T cells, B cells, NK cells, M1 macrophages and cytotoxic lymphocytes and increased expression level of immunomodulatory factors regulating immune cell recruitment, antigen presentation, T cell activation and cytotoxicity, but markedly lower abundance of neutrophils, M2 macrophages, and myeloid-derived suppressor cells. High SIRPG expression was associated with favorable response to PD-1 blockade in both NSCLC and melanoma. scRNA-seq data suggested SIRPG was mainly expressed in CD8+ exhausted T and CD4+ regulatory T cells, and positively associated with immune checkpoint expression including PDCD1 and CTLA4. In vitro test showed SIRPG expression in T cells could facilitate expression of PDCD1 and CTLA4. High SIRPG expression is associated with an inflamed immune phenotype in cancers and favorable response to PD-1 blockade, suggesting it would be a promising predictive biomarker for PD-1 blockade and novel immunotherapeutic target. © 2024. The Author(s).
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
CD276-dependent efferocytosis by tumor-associated macrophages promotes immune evasion in bladder cancer.
In Nature Communications on 1 April 2024 by Cheng, M., Chen, S., et al.
PubMed
Interplay between innate and adaptive immune cells is important for the antitumor immune response. However, the tumor microenvironment may turn immune suppressive, and tumor associated macrophages are playing a role in this transition. Here, we show that CD276, expressed on tumor-associated macrophages (TAM), play a role in diminishing the immune response against tumors. Using a model of tumors induced by N-butyl-N-(4-hydroxybutyl) nitrosamine in BLCA male mice we show that genetic ablation of CD276 in TAMs blocks efferocytosis and enhances the expression of the major histocompatibility complex class II (MHCII) of TAMs. This in turn increases CD4 + and cytotoxic CD8 + T cell infiltration of the tumor. Combined single cell RNA sequencing and functional experiments reveal that CD276 activates the lysosomal signaling pathway and the transcription factor JUN to regulate the expression of AXL and MerTK, resulting in enhanced efferocytosis in TAMs. Proving the principle, we show that simultaneous blockade of CD276 and PD-1 restrain tumor growth better than any of the components as a single intervention. Taken together, our study supports a role for CD276 in efferocytosis by TAMs, which is potentially targetable for combination immune therapy. © 2024. The Author(s).
- Cancer Research
DPP Inhibition Enhances the Efficacy of PD-1 Blockade by Remodeling the Tumor Microenvironment in Lewis Lung Carcinoma Model.
In Biomolecules on 25 March 2024 by Lei, M., Liu, J., et al.
PubMed
The remarkable efficacy of cancer immunotherapy has been established in several tumor types. Of the various immunotherapies, PD-1/PD-L1 inhibitors are most extensively used in the treatment of many cancers in clinics. These inhibitors restore the suppressed antitumor immune response and inhibit tumor progression by blocking the PD-1/PD-L1 signaling. However, the low response rate is a major limitation in the clinical application of PD-1/PD-L1 inhibitors. Therefore, combination strategies that enhance the response rate are the need of the hour. In this investigation, PT-100 (also referred to as Talabostat, Val-boroPro, and BXCL701), an orally administered and nonselective dipeptidyl peptidase inhibitor, not only augmented the effectiveness of anti-PD-1 therapy but also significantly improved T immune cell infiltration and reversed the immunosuppressive tumor microenvironment. The combination of PT-100 and anti-PD-1 antibody increased the number of CD4+ and CD8+ T cells. Moreover, the mRNA expression of T cell-associated molecules was elevated in the tumor microenvironment. The results further suggested that PT-100 dramatically reduced the ratio of tumor-associated macrophages. These findings provide a promising combination strategy for immunotherapy in lung cancer.
- Mus musculus (House mouse),
- Immunology and Microbiology
Inhibition of IL-25/IL-17RA improves immune-related adverse events of checkpoint inhibitors and reveals antitumor activity.
In Journal for Immunotherapy of Cancer on 21 March 2024 by Hu, X., Bukhari, S. M., et al.
PubMed
Immune checkpoint inhibitors (ICIs) have improved outcomes and extended patient survival in several tumor types. However, ICIs often induce immune-related adverse events (irAEs) that warrant therapy cessation, thereby limiting the overall effectiveness of this class of therapeutic agents. Currently, available therapies used to treat irAEs might also blunt the antitumor activity of the ICI themselves. Therefore, there is an urgent need to identify treatments that have the potential to be administered alongside ICI to optimize their use. Using a translationally relevant murine model of anti-PD-1 and anti-CTLA-4 antibodies-induced irAEs, we compared the safety and efficacy of prednisolone, anti-IL-6, anti-TNFɑ, anti-IL-25 (IL-17E), and anti-IL-17RA (the receptor for IL-25) administration to prevent irAEs and to reduce tumor size. While all interventions were adequate to inhibit the onset of irAEs pneumonitis and hepatitis, treatment with anti-IL-25 or anti-IL-17RA antibodies also exerted additional antitumor activity. Mechanistically, IL-25/IL-17RA blockade reduced the number of organ-infiltrating lymphocytes. These findings suggest that IL-25/IL-17RA may serve as an additional target when treating ICI-responsive tumors, allowing for better tumor control while suppressing immune-related toxicities. © Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Cancer Research,
- Immunology and Microbiology
Spermine Synthase Engages in Macrophages M2 polarization to Sabotage Antitumor Immunity in Hepatocellular Carcinoma
Preprint on Research Square on 19 March 2024 by Fang, Y., Sun, Y., et al.
PubMed
Disturbances in tumor cell metabolism reshape the tumor microenvironment (TME) and impair antitumor immunity, but the implicit mechanisms remain elusive. Here, we found that spermine synthase (SMS) was significantly upregulated in tumor cells, which correlated positively with immunosuppressive microenvironments and predicted poor survival in hepatocellular carcinoma (HCC) patients. Via “subcutaneous” and “orthotopic” HCC syngeneic mouse models and a series of in vitro coculture experiments, we identified elevated SMS level in HCC cells played a role in immune escape mainly through its metabolic product spermine, which induced tumor-associated macrophage (TAM) reprogramming and subsequently corresponded with a decreased antitumor functionality of CD8 + T cells. Mechanistically, we discovered that spermine reprogrammed TAM mainly by activating the PI3K-Akt-mTOR-S6K signaling pathway. Spermine inhibition in combination with immune checkpoint blockade effectively diminishes tumor burden in vivo . Our results expand the understanding of the critical role of metabolites in regulating cancer progression and anti-tumor immunity, and open new avenues for developing novel therapeutic strategies against HCC.
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Cancer Research
Assessing Longitudinal Treatment Efficacies and Alterations in Molecular Markers Associated with Glutamatergic Signaling and Immune Checkpoint Inhibitors in a Spontaneous Melanoma Mouse Model.
In JID Innovations on 1 March 2024 by Eddy, K., Gupta, K., et al.
PubMed
Previous work done by our laboratory described the use of an immunocompetent spontaneous melanoma-prone mouse model, TGS (TG-3/SKH-1), to evaluate treatment outcomes using inhibitors of glutamatergic signaling and immune checkpoint for 18 weeks. We showed a significant therapeutic efficacy with a notable sex-biased response in male mice. In this follow-up 18-week study, the dose of the glutamatergic signaling inhibitor was increased (from 1.7 mg/kg to 25 mg/kg), which resulted in improved responses in female mice but not male mice. The greatest reduction in tumor progression was observed in male mice treated with single-agent troriluzole and anti-PD-1. Furthermore, a randomly selected group of mice was removed from treatment after 18 weeks and maintained for up to an additional 48 weeks demonstrating the utility of the TGS mouse model to perform a ≥1-year preclinical therapeutic study in a physiologically relevant tumor-host environment. Digital spatial imaging analyses were performed in tumors and tumor microenvironments across treatment modalities using antibody panels for immune cell types and immune cell activation. The results suggest that immune cell populations and cytotoxic activities of T cells play critical roles in treatment responses in these mice. Examination of a group of molecular protein markers based on the proposed mechanisms of action of inhibitors of glutamatergic signaling and immune checkpoint showed that alterations in expression levels of xCT, γ-H2AX, EAAT2, PD-L1, and PD-1 are likely associated with the loss of treatment responses. These results suggest the importance of tracking changes in molecular markers associated with the mechanism of action of therapeutics over the course of a longitudinal preclinical therapeutic study in spatial and temporal manners. © 2024 The Authors.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
IFI35 limits antitumor immunity in triple-negative breast cancer via CCL2 secretion.
In Oncogene on 1 March 2024 by Xu, B., Sun, H., et al.
PubMed
Triple-negative breast cancer (TNBC) is the most aggressive subtype of breast cancer with poor prognosis due to the lack of therapeutic targets. Although immunotherapy brings survival benefits to patients diagnosed with TNBC, it remains limited and treatment resistance is widespread. Here we demonstrate that IFI35 is highly expressed in tumor tissues and can be induced by Interferon-γ in a time-dependent and concentration-dependent manner in breast cancer cells. In xenograft models, we reveal that IFI35 dramatically increases myeloid-derived suppressor cells infiltration in tumors, along with depletion and anergy of CD8+T cells. IFI35 ablation leads to prolonged survival of the mice. Mechanistically, RNA-sequencing reveals that IFI35 promotes CCL2 secretion, resulting in the remodeling of TNBC immune microenvironment. Ablation of IFI35 promotes the infiltration of effector CD8+T cells, and thereby sensitizes TNBC to anti-PD-1 immunotherapy. Our data suggest that IFI35 limits antitumor immunity and may be expected to become a new immunotherapy target in TNBC. © 2024. The Author(s).
- Mus musculus (House mouse),
- Cancer Research
S100A8/A9 predicts response to PIM kinase and PD-1/PD-L1 inhibition in triple-negative breast cancer mouse models.
In Commun Med (Lond) on 20 February 2024 by Begg, L. R., Orriols, A., et al.
PubMed
Understanding why some triple-negative breast cancer (TNBC) patients respond poorly to existing therapies while others respond well remains a challenge. This study aims to understand the potential underlying mechanisms distinguishing early-stage TNBC tumors that respond to clinical intervention from non-responders, as well as to identify clinically viable therapeutic strategies, specifically for TNBC patients who may not benefit from existing therapies. We conducted retrospective bioinformatics analysis of historical gene expression datasets to identify a group of genes whose expression levels in early-stage tumors predict poor clinical outcomes in TNBC. In vitro small-molecule screening, genetic manipulation, and drug treatment in syngeneic mouse models of TNBC were utilized to investigate potential therapeutic strategies and elucidate mechanisms of drug action. Our bioinformatics analysis reveals a robust association between increased expression of immunosuppressive cytokine S100A8/A9 in early-stage tumors and subsequent disease progression in TNBC. A targeted small-molecule screen identifies PIM kinase inhibitors as capable of decreasing S100A8/A9 expression in multiple cell types, including TNBC and immunosuppressive myeloid cells. Combining PIM inhibition and immune checkpoint blockade induces significant antitumor responses, especially in otherwise resistant S100A8/A9-high PD-1/PD-L1-positive tumors. Notably, serum S100A8/A9 levels mirror those of tumor S100A8/A9 in a syngeneic mouse model of TNBC. Our data propose S100A8/A9 as a potential predictive and pharmacodynamic biomarker in clinical trials evaluating combination therapy targeting PIM and immune checkpoints in TNBC. This work encourages the development of S100A8/A9-based liquid biopsy tests for treatment guidance. © 2024. The Author(s).
- Mus musculus (House mouse)
Several first-line anti-hypertensives act on fibrosarcoma progression and PD1ab blockade therapy.
In Journal of Orthopaedic Surgery and Research on 19 February 2024 by Sun, J., Zhang, C., et al.
PubMed
Patients are typically diagnosed with both hypertension and fibrosarcoma. Medical oncologists must prescribe suitable anti-hypertensive medications while considering anti-tumor drugs. Recently, immunotherapy has become prominent in cancer treatment. Nonetheless, it is unknown what role anti-hypertensive medications will play in immunotherapy. We examined the effects of six first-line anti-hypertensive medications on programmed cell death protein 1 antibody (PD1ab) in tumor treatment using a mouse model of subcutaneous fibrosarcoma. The drugs examined were verapamil, losartan, furosemide, spironolactone, captopril, and hydrochlorothiazide (HCTZ). The infiltration of CD8+ T cells was examined by immunohistochemistry. Additionally, several in vitro and in vivo assays were used to study the effects of HCTZ on human fibrosarcoma cancer cells to explore its mechanism. Verapamil suppressed tumor growth and showed an improved effect on the tumor inhibition of PD1ab. Captopril did not affect tumor growth but brought an unexpected benefit to PD1ab treatment. In contrast, spironolactone and furosemide showed no effect on tumor growth but had an offset effect on the PD1ab therapy. Consequently, the survival time of mice was also significantly reduced. Notably, losartan and HCTZ, especially HCTZ, promoted tumor growth and weakened the effect of PD1ab treatment. Consistent results were observed in vivo and in vitro using the human fibrosarcoma cell line HT1080. We determined that the Solute Carrier Family 12 Member 3 (SLC12A3), a known target of HCTZ, may be the principal factor underlying its effect-enhancing properties through mechanism studies employing The Cancer Genome Atlas (TCGA) data and in vivo and in vitro assays. Verapamil and captopril potentiated the anti-tumor effect of PD1ab, whereas spironolactone and furosemide weakened the effect of PD1ab on tumor inhibition. Alarmingly, losartan and HCTZ promoted tumor growth and impaired the effect of PD1ab. Furthermore, we preliminarily found that HCTZ may promote tumor progression through SLC12A3. Based on this study, futher mechanism researches and clinical trials should be conducted in the future. © 2024. The Author(s).
- Mus musculus (House mouse),
- Cancer Research
Homologous-Magnetic Dual-Targeted Metal-Organic Framework to Improve the Anti-Hepatocellular Carcinoma Efficacy of PD-1 Inhibitor
Preprint on Research Square on 8 February 2024 by Guo, H., Li, X., et al.
PubMed
The insufficient abundance and weak activity of tumour-infiltrating lymphocytes (TILs) are two important reasons for the poor efficacy of PD-1 inhibitors in hepatocellular carcinoma (HCC) treatment. The combined administration of tanshinone Ⅱ A (TSA) and astragaloside IV (As) can up-regulate the abundance and activity of TILs by normalising tumour blood vessels and reducing the levels of immunosuppressive factors respectively. For enhancing the efficacy of PD-1 antibody, a magnetic metal–organic framework (MOF) with a homologous tumour cell membrane (Hm) coating (Hm@TSA/As-MOF) is established to co-deliver TSA&As into the HCC microenvironment. Hm@TSA/As-MOF is a spherical nanoparticle and has a high total drug-loading capacity of 16.13 wt%. The Hm coating and magnetic responsiveness of Hm@TSA/As-MOF provide a homologous-magnetic dual-targeting, which enable Hm@TSA/As-MOF to counteract the interference posed by ascites tumour cells and enhance the precision of targeting solid tumours. Hm coating also enable Hm@TSA/As-MOF to evade immune clearance by macrophages. The release of TSA&As from Hm@TSA/As-MOF can be accelerated by HCC microenvironment, thereby up-regulating the abundance and activity of TILs to synergistic PD-1 antibody against HCC. This study presents a nanoplatform to improve the efficacy of PD-1 inhibitors in HCC, providing a novel approach for anti-tumour immunotherapy in clinical practice.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
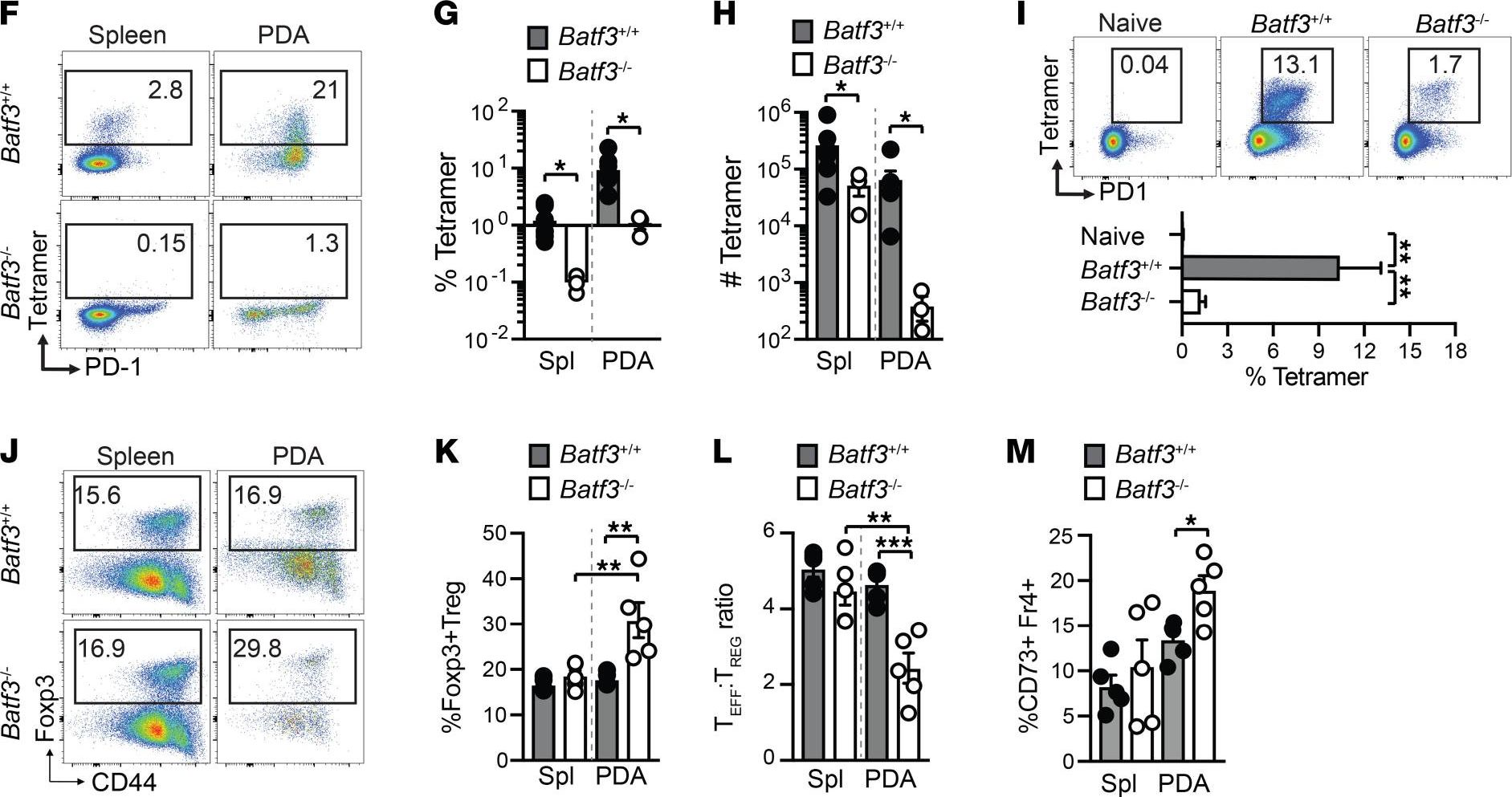
Cytokine-armed dendritic cell progenitors for antigen-agnostic cancer immunotherapy.
In Nature Cancer on 1 February 2024 by Ghasemi, A., Martinez-Usatorre, A., et al.
PubMed
Dendritic cells (DCs) are antigen-presenting myeloid cells that regulate T cell activation, trafficking and function. Monocyte-derived DCs pulsed with tumor antigens have been tested extensively for therapeutic vaccination in cancer, with mixed clinical results. Here, we present a cell-therapy platform based on mouse or human DC progenitors (DCPs) engineered to produce two immunostimulatory cytokines, IL-12 and FLT3L. Cytokine-armed DCPs differentiated into conventional type-I DCs (cDC1) and suppressed tumor growth, including melanoma and autochthonous liver models, without the need for antigen loading or myeloablative host conditioning. Tumor response involved synergy between IL-12 and FLT3L and was associated with natural killer and T cell infiltration and activation, M1-like macrophage programming and ischemic tumor necrosis. Antitumor immunity was dependent on endogenous cDC1 expansion and interferon-γ signaling but did not require CD8+ T cell cytotoxicity. Cytokine-armed DCPs synergized effectively with anti-GD2 chimeric-antigen receptor (CAR) T cells in eradicating intracranial gliomas in mice, illustrating their potential in combination therapies. © 2023. The Author(s).
- Mus musculus (House mouse),
- Immunology and Microbiology
An oncogene regulating chromatin favors response to immunotherapy: Oncogene CHAF1A and immunotherapy outcomes.
In Oncoimmunology on 18 January 2024 by Ying, L., Hu, Z., et al.
PubMed
Many biological processes related to cell function and fate begin with chromatin alterations, and many factors associated with the efficacy of immune checkpoint inhibitors (ICIs) are actually downstream events of chromatin alterations, such as genome changes, neoantigen production, and immune checkpoint expression. However, the influence of genes as chromatin regulators on the efficacy of ICIs remains elusive, especially in gastric cancer (GC). In this study, thirty out of 1593 genes regulating chromatin associated with a favorable prognosis were selected for GC. CHAF1A, a well-defined oncogene, was identified as the highest linkage hub gene. High CHAF1A expression were associated with microsatellite instability (MSI), high tumor mutation burden (TMB), high tumor neoantigen burden (TNB), high expressions of PD-L1 and immune effector genes, and live infiltration of immune cells. High CHAF1A expression indicated a favorable response and prognosis in immunotherapy of several cohorts, which was independent of MSI, TMB, TNB, PD-L1 expression, immune phenotype and transcriptome scoring, and improved patient selection based on these classic biomarkers. In vivo, CHAF1A knockdown alone inhibited tumor growth but it impaired the effect of an anti-PD-1 antibody by increasing the relative tumor proliferation rate and decreasing the survival benefit, potentially through the activation of TGF-β signaling. In conclusion, CHAF1A may be a novel biomarker for improving patient selection in immunotherapy. © 2024 The Author(s). Published with license by Taylor & Francis Group, LLC.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Shikonin improves the effectiveness of PD-1 blockade in colorectal cancer by enhancing immunogenicity via Hsp70 upregulation.
In Molecular Biology Reports on 6 January 2024 by Chen, J., Liu, J., et al.
PubMed
PD-1 blockade has shown impressive clinical outcomes in colorectal cancers patients with high microsatellite instability (MSI-H). However, the majority of patients with colorectal cancer who present low microsatellite instability (MSI-L) or stable microsatellites (MSS) show little response to PD-1 blockade therapy. Here, we have demonstrated that Shikonin (SK) could induce cell death of CT26 cells via classically programmed and immunogenic pathways. SK promoted the membrane exposure of calreticulin and upregulated the expression of heat shock protein 70 (Hsp70). The upregulation of Hsp70 was dependent on ROS induced by SK and silencing of PKM2 in CT26 cells reverts ROS upregulation. Besides, SK synergizes with PD-1 blockade in CT26 tumor mice model, with the increase of intramural DC cells and CD8+ T cells. The expression of Hsp70 in tumor tissue was also increased in combinational SK plus αPD-1 therapy group. Our study elucidated the potential role of 'Shikonin-PKM2-ROS-Hsp70' axis in the promotion of efficacy of PD-1 blockade in CRC treatments, providing a potential strategy and targets for improving the efficacy of PD-1 blockade in colorectal cancer. © 2024. The Author(s).
- Mus musculus (House mouse),
- Cancer Research
Gasdermin C sensitizes tumor cells to PARP inhibitor therapy in cancer models.
In The Journal of Clinical Investigation on 2 January 2024 by Wang, S., Chang, C. W., et al.
PubMed
Several poly (ADP-ribose) polymerase (PARP) inhibitors (PARPi) are approved by FDA to treat cancer with BRCA mutations. BRCA mutations are considered to fuel a PARPi killing effect by inducing apoptosis. However, resistance to PARPi is frequently observed in the clinic due to an incomplete understanding on the molecular basis of PARPi function and a lack of good markers, beyond BRCA mutations, to predict response. Here, we show that gasdermin C (GSDMC) sensitized tumor cells to PARPi in vitro and in immunocompetent mice and caused durable tumor regression in an immune-dependent manner. A high expression level of GSDMC predicted better response to PARPi treatment in patients with triple-negative breast cancer (TNBC). PARPi treatment triggered GSDMC/caspase-8-mediated cancer cell pyroptosis (CCP) that enhanced PARPi killing of tumor cells. GSDMC-mediated CCP increased memory CD8+ T cell population in lymph node (LN), spleen, and tumor and, thus, promoted cytotoxic CD8+ T cell infiltration in the tumor microenvironment. T cell-derived granzyme B (GZMB) activated caspase-6, which subsequently cleaved GSDMC to induce pyroptosis. Interestingly, IFN-γ induced GSDMC expression, which, in turn, enhanced the cytotoxicity of PARPi and T cells. Importantly, GSDMC promoted tumor clearance independent of BRCA deficiency in multiple cancer types with PARPi treatment. This study identifies a general marker and target for PARPi therapy and offers insights into the mechanism of PARPi function.
- Mus musculus (House mouse),
- Cancer Research
A multidimensional platform of patient-derived tumors identifies drug susceptibilities for clinical lenvatinib resistance.
In Acta Pharmaceutica Sinica. B on 1 January 2024 by Sun, L., Wan, A. H., et al.
PubMed
Lenvatinib, a second-generation multi-receptor tyrosine kinase inhibitor approved by the FDA for first-line treatment of advanced liver cancer, facing limitations due to drug resistance. Here, we applied a multidimensional, high-throughput screening platform comprising patient-derived resistant liver tumor cells (PDCs), organoids (PDOs), and xenografts (PDXs) to identify drug susceptibilities for conquering lenvatinib resistance in clinically relevant settings. Expansion and passaging of PDCs and PDOs from resistant patient liver tumors retained functional fidelity to lenvatinib treatment, expediting drug repurposing screens. Pharmacological screening identified romidepsin, YM155, apitolisib, NVP-TAE684 and dasatinib as potential antitumor agents in lenvatinib-resistant PDC and PDO models. Notably, romidepsin treatment enhanced antitumor response in syngeneic mouse models by triggering immunogenic tumor cell death and blocking the EGFR signaling pathway. A combination of romidepsin and immunotherapy achieved robust and synergistic antitumor effects against lenvatinib resistance in humanized immunocompetent PDX models. Collectively, our findings suggest that patient-derived liver cancer models effectively recapitulate lenvatinib resistance observed in clinical settings and expedite drug discovery for advanced liver cancer, providing a feasible multidimensional platform for personalized medicine. © 2024 The Authors.
- Immunology and Microbiology,
- Cancer Research
Ex Vivo Evaluation of Combination Immunotherapy Using Tumor-Microenvironment-on-Chip.
In Advanced Healthcare Materials on 1 January 2024 by Mu, H. Y., Lin, C. M., et al.
PubMed
Combination immunotherapy has emerged as a promising strategy to address the challenges associated with immune checkpoint inhibitor (ICI) therapy in breast cancer. The efficacy of combination immunotherapy hinges upon the intricate and dynamic nature of the tumor microenvironment (TME), characterized by cellular heterogeneity and molecular gradients. However, current methodologies for drug screening often fail to accurately replicate these complex conditions, resulting in limited predictive capacity for treatment outcomes. Here, a tumor-microenvironment-on-chip (TMoC), integrating a circulation system and ex vivo tissue culture with physiological oxygen and nutrient gradients, is described. This platform enables spatial infiltration of cytotoxic CD8+ T cells and their targeted attack on the tumor, while preserving the high complexity and heterogeneity of the TME. The TMoC is employed to assess the synergistic effect of five targeted therapy drugs and five chemotherapy drugs in combination with immunotherapy, demonstrating strong concordance between chip and animal model responses. The TMoC holds significant potential for advancing drug development and guiding clinical decision-making, as it offers valuable insights into the complex dynamics of the TME. © 2023 Wiley-VCH GmbH.
- Mus musculus (House mouse),
- Cancer Research
Single-cell deconvolution reveals high lineage- and location-dependent heterogeneity in mesenchymal multivisceral stage 4 colorectal cancer.
In The Journal of Clinical Investigation on 28 December 2023 by Berlin, C., Mauerer, B., et al.
PubMed
Metastasized colorectal cancer (CRC) is associated with a poor prognosis and rapid disease progression. Besides hepatic metastasis, peritoneal carcinomatosis is the major cause of death in Union for International Cancer Control (UICC) stage IV CRC patients. Insights into differential site-specific reconstitution of tumor cells and the corresponding tumor microenvironment are still missing. Here, we analyzed the transcriptome of single cells derived from murine multivisceral CRC and delineated the intermetastatic cellular heterogeneity regarding tumor epithelium, stroma, and immune cells. Interestingly, we found an intercellular site-specific network of cancer-associated fibroblasts and tumor epithelium during peritoneal metastasis as well as an autologous feed-forward loop in cancer stem cells. We furthermore deciphered a metastatic dysfunctional adaptive immunity by a loss of B cell-dependent antigen presentation and consecutive effector T cell exhaustion. Furthermore, we demonstrated major similarities of this murine metastatic CRC model with human disease and - based on the results of our analysis - provided an auspicious site-specific immunomodulatory treatment approach for stage IV CRC by intraperitoneal checkpoint inhibition.
- Immunology and Microbiology,
- Cancer Research
Lactose blocks intercellular spreading of Galectin-1 from cancer cells to T-cells and activates tumor immunological control
Preprint on BioRxiv : the Preprint Server for Biology on 20 December 2023 by Hong, Y., Si, X., et al.
PubMed
Understanding the mechanisms by which the immune system surveils cancer is the key to developing better tumor immunotherapy strategies. By CRISPR/Cas9 screenings, we identified that inactivation of beta-1,4-galactosyltransferase-1 (B4GALT1), a key enzyme in glycoconjugate biosynthesis, leads to enhanced T-cell receptor (TCR) activation and functions of CD8 + T-cells. Via proximity-dependent-intercellular-protein-spreading (PDICPS), cancer cells transfer surface-bound galectin-1 (Gal-1) proteins, which recognize and bind galactosylated membrane proteins, to CD8 + T-cells, thereby suppressing T-cell-mediated cytolysis. B4GALT1-deficiency leads to reduced cell-surface galactosylation and Gal-1 binding of CD8 + T-cells. Proteomic analysis revealed reduced binding of Gal-1 with TCR and its coreceptor CD8 on B4GALT1-deficient CD8 + T-cells, leading to enhanced TCR-CD8 colocalization and T-cell activation. Lactose, a structure-mimicking competitive inhibitor of N-glycan galactosylation, enhances the functions of CD8 + T-cells and tumor immunosurveillance. Results from various preclinical tumor models demonstrate that lactose and its derivatives are a new class of immune checkpoint inhibitors for tumor immunotherapy.