InVivoMAb anti-mouse PD-L1 (B7-H1)
Product Description
Specifications
| Isotype | Rat IgG2b, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2b isotype control, anti-keyhole limpet hemocyanin |
| Recommended Dilution Buffer | InVivoPure pH 6.5 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse CD274 |
| Reported Applications |
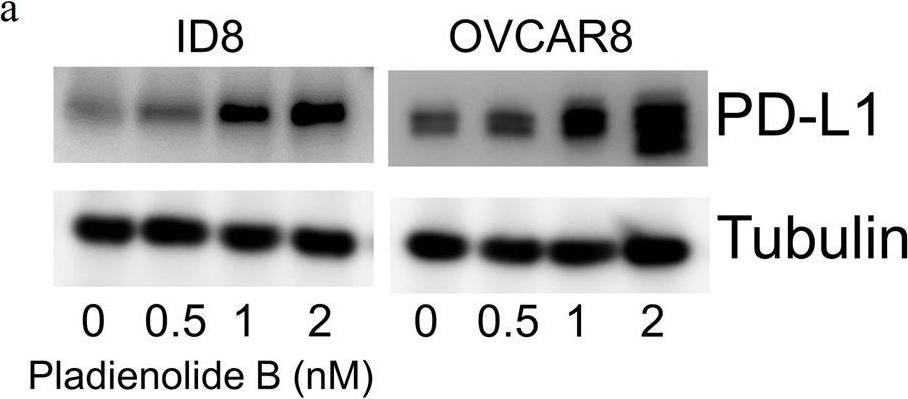
in vivo PD-L1 blockade in vitro PD-L1 blockade Immunofluorescence Immunohistochemistry (frozen) Flow cytometry Western blot |
| Formulation |
PBS, pH 6.5 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL gel clotting assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10949073 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo PD-L1 blockade
Grasselly, C., et al. (2018). "The Antitumor Activity of Combinations of Cytotoxic Chemotherapy and Immune Checkpoint Inhibitors Is Model-Dependent" Front Immunol 9: 2100.
PubMed
In spite of impressive response rates in multiple cancer types, immune checkpoint inhibitors (ICIs) are active in only a minority of patients. Alternative strategies currently aim to combine immunotherapies with conventional agents such as cytotoxic chemotherapies. Here, we performed a study of PD-1 or PDL-1 blockade in combination with reference chemotherapies in four fully immunocompetent mouse models of cancer. We analyzed both the in vivo antitumor response, and the tumor immune infiltrate 4 days after the first treatment. in vivo tumor growth experiments revealed variable responsiveness to ICIs between models. We observed enhanced antitumor effects of the combination of immunotherapy with chemotherapy in the MC38 colon and MB49 bladder models, a lack of response in the 4T1 breast model, and an inhibition of ICIs activity in the MBT-2 bladder model. Flow cytometry analysis of tumor samples showed significant differences in all models between untreated and treated mice. At baseline, all the tumor models studied were predominantly infiltrated with cells harboring an immunosuppressive phenotype. Early alterations of the tumor immune infiltrate after treatment were found to be highly variable. We found that the balance between effector cells and immunosuppressive cells in the tumor microenvironment could be altered with some treatment combinations, but this effect was not always correlated with an impact on in vivo tumor growth. These results show that the combination of cytotoxic chemotherapy with ICIs may result in enhanced, similar or reduced antitumor activity, in a model- and regimen-dependent fashion. The present investigations should help to select appropriate combination regimens for ICIs.
in vivo PD-L1 blockade
Stathopoulou, C., et al. (2018). "PD-1 Inhibitory Receptor Downregulates Asparaginyl Endopeptidase and Maintains Foxp3 Transcription Factor Stability in Induced Regulatory T Cells" Immunity 49(2): 247-263 e247.
PubMed
CD4(+) T cell differentiation into multiple T helper (Th) cell lineages is critical for optimal adaptive immune responses. This report identifies an intrinsic mechanism by which programmed death-1 receptor (PD-1) signaling imparted regulatory phenotype to Foxp3(+) Th1 cells (denoted as Tbet(+)iTregPDL1 cells) and inducible regulatory T (iTreg) cells. Tbet(+)iTregPDL1 cells prevented inflammation in murine models of experimental colitis and experimental graft versus host disease (GvHD). Programmed death ligand-1 (PDL-1) binding to PD-1 imparted regulatory function to Tbet(+)iTregPDL1 cells and iTreg cells by specifically downregulating endo-lysosomal protease asparaginyl endopeptidase (AEP). AEP regulated Foxp3 stability and blocking AEP imparted regulatory function in Tbet(+)iTreg cells. Also, Aep(-/-) iTreg cells significantly inhibited GvHD and maintained Foxp3 expression. PD-1-mediated Foxp3 maintenance in Tbet(+) Th1 cells occurred both in tumor infiltrating lymphocytes (TILs) and during chronic viral infection. Collectively, this report has identified an intrinsic function for PD-1 in maintaining Foxp3 through proteolytic pathway.
in vivo PD-L1 blockade
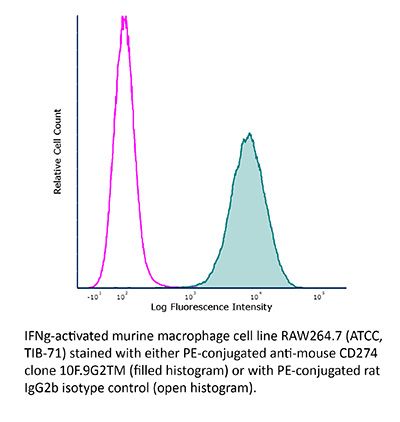
Flow Cytometry
Aloulou, M., et al. (2016). "Follicular regulatory T cells can be specific for the immunizing antigen and derive from naive T cells" Nat Commun 7: 10579.
PubMed
T follicular regulatory (Tfr) cells are a subset of Foxp3(+) regulatory T (Treg) cells that form in response to immunization or infection, which localize to the germinal centre where they control the magnitude of the response. Despite an increased interest in the role of Tfr cells in humoral immunity, many fundamental aspects of their biology remain unknown, including whether they recognize self- or foreign antigen. Here we show that Tfr cells can be specific for the immunizing antigen, irrespective of whether it is a self- or foreign antigen. We show that, in addition to developing from thymic derived Treg cells, Tfr cells can also arise from Foxp3(-) precursors in a PD-L1-dependent manner, if the adjuvant used is one that supports T-cell plasticity. These findings have important implications for Tfr cell biology and for improving vaccine efficacy by formulating vaccines that modify the Tfr:Tfh cell ratio.
in vivo PD-L1 blockade
Tkachev, V., et al. (2015). "Programmed death-1 controls T cell survival by regulating oxidative metabolism" J Immunol 194(12): 5789-5800.
PubMed
The coinhibitory receptor programmed death-1 (PD-1) maintains immune homeostasis by negatively regulating T cell function and survival. Blockade of PD-1 increases the severity of graft-versus-host disease (GVHD), but the interplay between PD-1 inhibition and T cell metabolism is not well studied. We found that both murine and human alloreactive T cells concomitantly upregulated PD-1 expression and increased levels of reactive oxygen species (ROS) following allogeneic bone marrow transplantation. This PD-1(Hi)ROS(Hi) phenotype was specific to alloreactive T cells and was not observed in syngeneic T cells during homeostatic proliferation. Blockade of PD-1 signaling decreased both mitochondrial H2O2 and total cellular ROS levels, and PD-1-driven increases in ROS were dependent upon the oxidation of fatty acids, because treatment with etomoxir nullified changes in ROS levels following PD-1 blockade. Downstream of PD-1, elevated ROS levels impaired T cell survival in a process reversed by antioxidants. Furthermore, PD-1-driven changes in ROS were fundamental to establishing a cell’s susceptibility to subsequent metabolic inhibition, because blockade of PD-1 decreased the efficacy of later F1F0-ATP synthase modulation. These data indicate that PD-1 facilitates apoptosis in alloreactive T cells by increasing ROS in a process dependent upon the oxidation of fat. In addition, blockade of PD-1 undermines the potential for subsequent metabolic inhibition, an important consideration given the increasing use of anti-PD-1 therapies in the clinic.
in vivo PD-L1 blockade
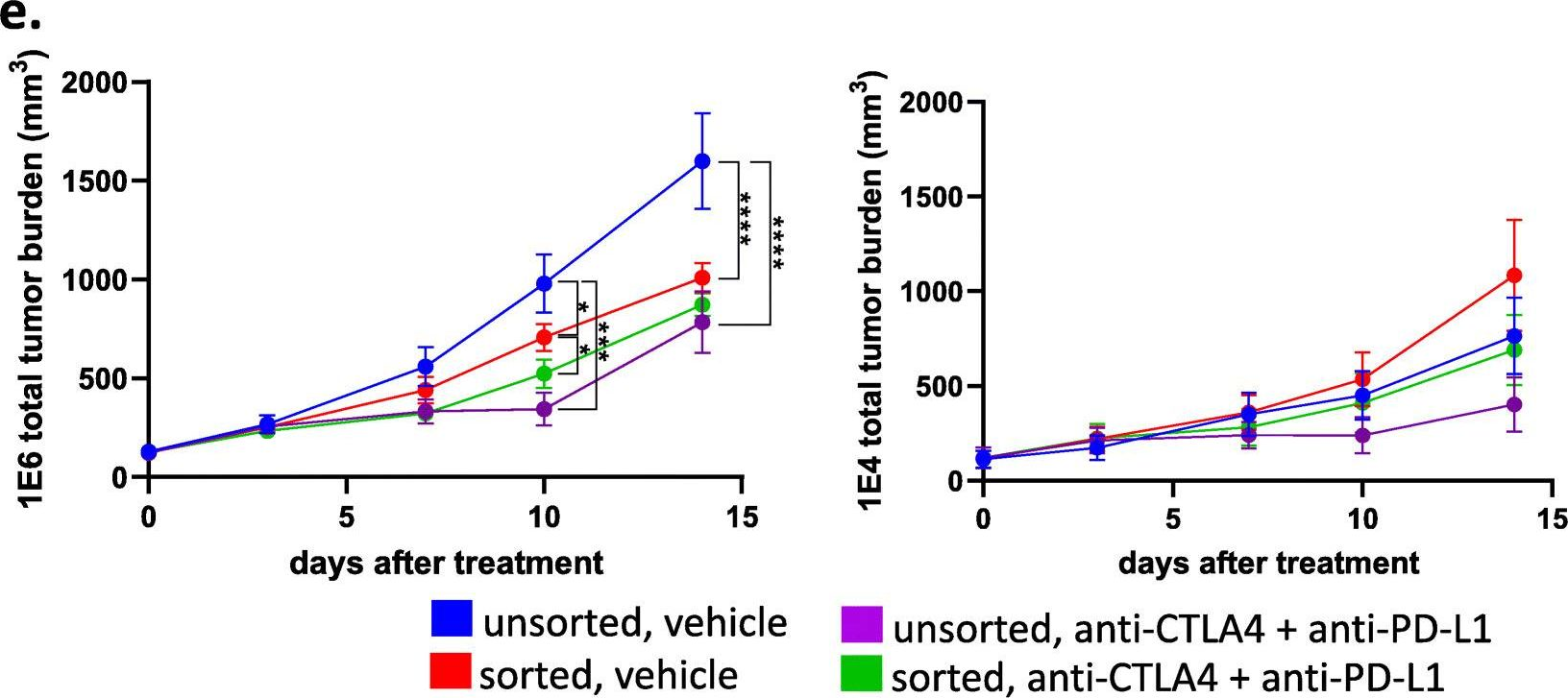
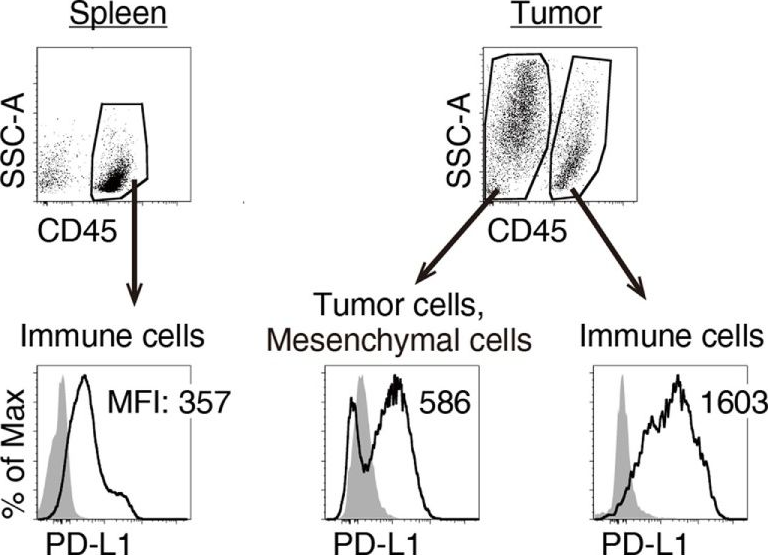
Twyman-Saint Victor, C., et al. (2015). "Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer" Nature 520(7547): 373-377.
PubMed
Immune checkpoint inhibitors result in impressive clinical responses, but optimal results will require combination with each other and other therapies. This raises fundamental questions about mechanisms of non-redundancy and resistance. Here we report major tumour regressions in a subset of patients with metastatic melanoma treated with an anti-CTLA4 antibody (anti-CTLA4) and radiation, and reproduced this effect in mouse models. Although combined treatment improved responses in irradiated and unirradiated tumours, resistance was common. Unbiased analyses of mice revealed that resistance was due to upregulation of PD-L1 on melanoma cells and associated with T-cell exhaustion. Accordingly, optimal response in melanoma and other cancer types requires radiation, anti-CTLA4 and anti-PD-L1/PD-1. Anti-CTLA4 predominantly inhibits T-regulatory cells (Treg cells), thereby increasing the CD8 T-cell to Treg (CD8/Treg) ratio. Radiation enhances the diversity of the T-cell receptor (TCR) repertoire of intratumoral T cells. Together, anti-CTLA4 promotes expansion of T cells, while radiation shapes the TCR repertoire of the expanded peripheral clones. Addition of PD-L1 blockade reverses T-cell exhaustion to mitigate depression in the CD8/Treg ratio and further encourages oligoclonal T-cell expansion. Similarly to results from mice, patients on our clinical trial with melanoma showing high PD-L1 did not respond to radiation plus anti-CTLA4, demonstrated persistent T-cell exhaustion, and rapidly progressed. Thus, PD-L1 on melanoma cells allows tumours to escape anti-CTLA4-based therapy, and the combination of radiation, anti-CTLA4 and anti-PD-L1 promotes response and immunity through distinct mechanisms.
in vivo PD-L1 blockade
Zander, R. A., et al. (2015). "PD-1 Co-inhibitory and OX40 Co-stimulatory Crosstalk Regulates Helper T Cell Differentiation and Anti-Plasmodium Humoral Immunity" Cell Host Microbe 17(5): 628-641.
PubMed
The differentiation and protective capacity of Plasmodium-specific T cells are regulated by both positive and negative signals during malaria, but the molecular and cellular details remain poorly defined. Here we show that malaria patients and Plasmodium-infected rodents exhibit atypical expression of the co-stimulatory receptor OX40 on CD4 T cells and that therapeutic enhancement of OX40 signaling enhances helper CD4 T cell activity, humoral immunity, and parasite clearance in rodents. However, these beneficial effects of OX40 signaling are abrogated following coordinate blockade of PD-1 co-inhibitory pathways, which are also upregulated during malaria and associated with elevated parasitemia. Co-administration of biologics blocking PD-1 and promoting OX40 signaling induces excessive interferon-gamma that directly limits helper T cell-mediated support of humoral immunity and decreases parasite control. Our results show that targeting OX40 can enhance Plasmodium control and that crosstalk between co-inhibitory and co-stimulatory pathways in pathogen-specific CD4 T cells can impact pathogen clearance.
in vivo PD-L1 blockade
Kim, J., et al. (2015). "Memory programming in CD8(+) T-cell differentiation is intrinsic and is not determined by CD4 help" Nat Commun 6: 7994.
PubMed
CD8(+) T cells activated without CD4(+) T-cell help are impaired in memory expansion. To understand the underlying cellular mechanism, here we track the dynamics of helper-deficient CD8(+) T-cell response to a minor histocompatibility antigen by phenotypic and in vivo imaging analyses. Helper-deficient CD8(+) T cells show reduced burst expansion, rapid peripheral egress, delayed antigen clearance and continuous activation, and are eventually exhausted. Contrary to the general consensus that CD4 help encodes memory programmes in CD8(+) T cells and helper-deficient CD8(+) T cells are abortive, these cells can differentiate into effectors and memory precursors. Importantly, accelerating antigen clearance or simply increasing the burst effector size enables generation of memory cells by CD8(+) T cells, regardless of CD4 help. These results suggest that the memory programme is CD8(+) T-cell-intrinsic, and provide insight into the role of CD4 help in CD8(+) T-cell responses.
in vivo PD-L1 blockade
Jaworska, K., et al. (2015). "Both PD-1 ligands protect the kidney from ischemia reperfusion injury" J Immunol 194(1): 325-333.
PubMed
Acute kidney injury (AKI) is a common problem in hospitalized patients that enhances morbidity and mortality and promotes the development of chronic and end-stage renal disease. Ischemia reperfusion injury (IRI) is one of the major causes of AKI and is characterized by uncontrolled renal inflammation and tubular epithelial cell death. Our recent studies demonstrated that regulatory T cells (Tregs) protect the kidney from ischemia reperfusion-induced inflammation and injury. Blockade of programmed death-1 (PD-1) on the surface of Tregs, prior to adoptive transfer, negates their ability to protect against ischemic kidney injury. The present study was designed to investigate the role of the known PD-1 ligands, PD-L1 and PD-L2, in kidney IRI. Administration of PD-L1 or PD-L2 blocking Abs prior to mild or moderate kidney IRI significantly exacerbated the loss of renal function, renal inflammation, and acute tubular necrosis compared with mice receiving isotype control Abs. Interestingly, blockade of both PD-1 ligands resulted in worse injury, dysfunction, and inflammation than did blocking either ligand alone. Genetic deficiency of either PD-1 ligand also exacerbated kidney dysfunction and acute tubular necrosis after subthreshold ischemia. Bone marrow chimeric studies revealed that PD-L1 expressed on non-bone marrow-derived cells is critical for this resistance to IRI. Finally, blockade of either PD-1 ligand negated the protective ability of adoptively transferred Tregs in IRI. These findings suggest that PD-L1 and PD-L2 are nonredundant aspects of the natural protective response to ischemic injury and may be novel therapeutic targets for AKI.
in vivo PD-L1 blockade
Flow Cytometry
Ngiow, S. F., et al. (2015). "A Threshold Level of Intratumor CD8+ T-cell PD1 Expression Dictates Therapeutic Response to Anti-PD1" Cancer Res 75(18): 3800-3811.
PubMed
Despite successes, thus far, a significant proportion of the patients treated with anti-PD1 antibodies have failed to respond. We use mouse tumor models of anti-PD1 sensitivity and resistance and flow cytometry to assess tumor-infiltrating immune cells immediately after therapy. We demonstrate that the expression levels of T-cell PD1 (PD1(lo)), myeloid, and T-cell PDL1 (PDL1(hi)) in the tumor microenvironment inversely correlate and dictate the efficacy of anti-PD1 mAb and function of intratumor CD8(+) T cells. In sensitive tumors, we reveal a threshold for PD1 downregulation on tumor-infiltrating CD8(+) T cells below which the release of adaptive immune resistance is achieved. In contrast, PD1(hi) T cells in resistant tumors fail to be rescued by anti-PD1 therapy and remain dysfunctional unless intratumor PDL1(lo) immune cells are targeted. Intratumor Tregs are partly responsible for the development of anti-PD1-resistant tumors and PD1(hi) CD8(+) T cells. Our analyses provide a framework to interrogate intratumor CD8(+) T-cell PD1 and immune PDL1 levels and response in human cancer. Cancer Res; 75(18); 3800-11. (c)2015 AACR.
in vivo PD-L1 blockade
Yang, X., et al. (2014). "Targeting the tumor microenvironment with interferon-beta bridges innate and adaptive immune responses" Cancer Cell 25(1): 37-48.
PubMed
Antibodies (Abs) that preferentially target oncogenic receptors have been increasingly used for cancer therapy, but tumors often acquire intrinsic Ab resistance after prolonged and costly treatment. Herein we armed the Ab with IFNbeta and observed that it is more potent than the first generation of Ab for controlling Ab-resistant tumors. This strategy controls Ab resistance by rebridging suppressed innate and adaptive immunity in the tumor microenvironment. Mechanistically, Ab-IFNbeta therapy primarily and directly targets intratumoral dendritic cells, which reactivate CTL by increasing antigen cross-presentation within the tumor microenvironment. Additionally, blocking PD-L1, which is induced by Ab-IFNbeta treatment, overcomes treatment-acquired resistance and completely eradicates established tumors. This study establishes a next-generation Ab-based immunotherapy that targets and eradicates established Ab-resistant tumors.
in vivo PD-L1 blockade
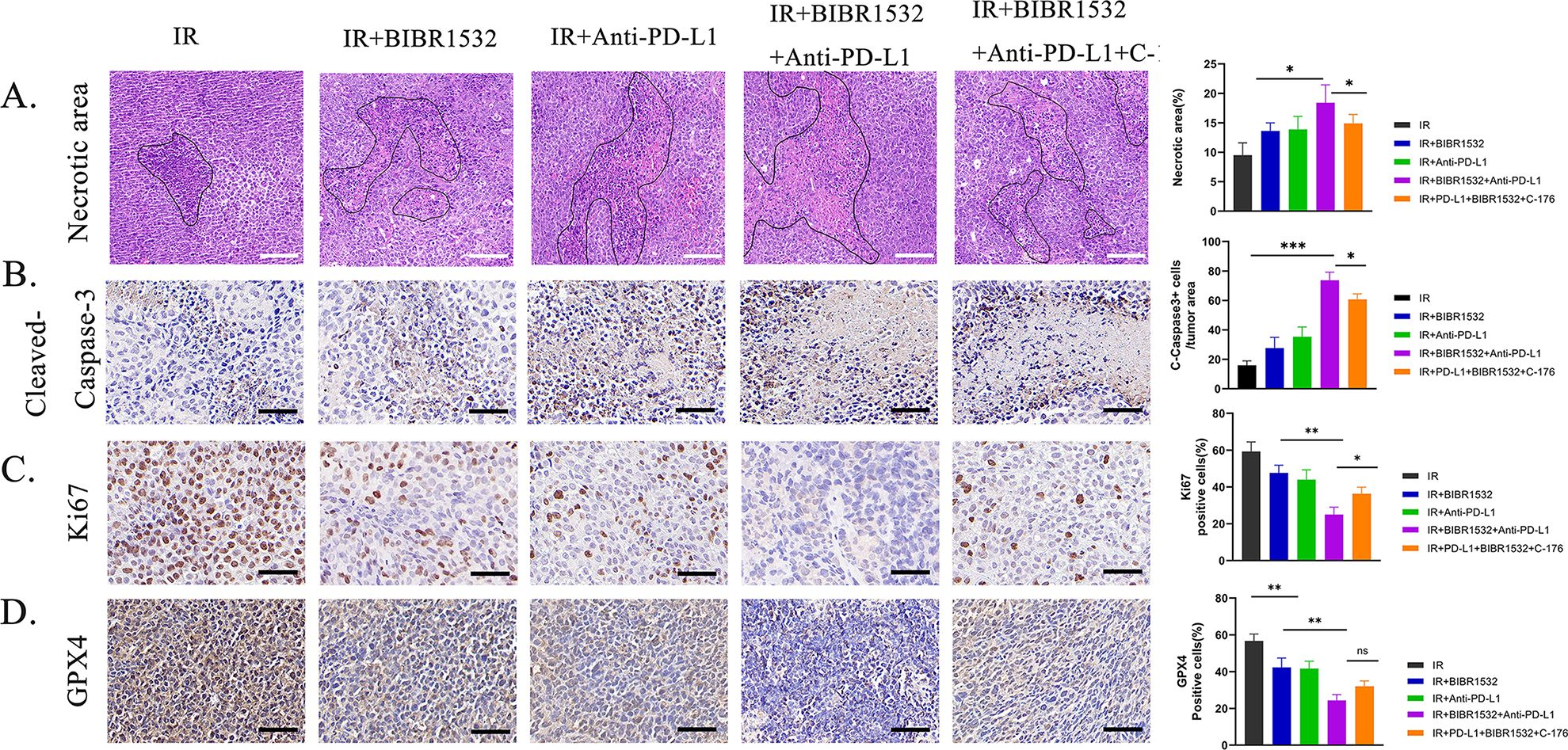
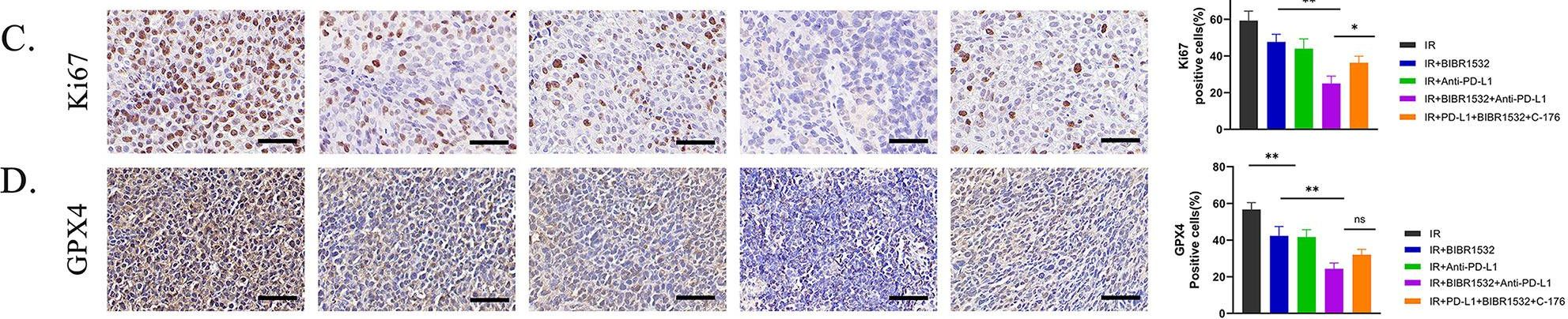
Deng, L., et al. (2014). "Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice" J Clin Invest 124(2): 687-695.
PubMed
High-dose ionizing irradiation (IR) results in direct tumor cell death and augments tumor-specific immunity, which enhances tumor control both locally and distantly. Unfortunately, local relapses often occur following IR treatment, indicating that IR-induced responses are inadequate to maintain antitumor immunity. Therapeutic blockade of the T cell negative regulator programmed death-ligand 1 (PD-L1, also called B7-H1) can enhance T cell effector function when PD-L1 is expressed in chronically inflamed tissues and tumors. Here, we demonstrate that PD-L1 was upregulated in the tumor microenvironment after IR. Administration of anti-PD-L1 enhanced the efficacy of IR through a cytotoxic T cell-dependent mechanism. Concomitant with IR-mediated tumor regression, we observed that IR and anti-PD-L1 synergistically reduced the local accumulation of tumor-infiltrating myeloid-derived suppressor cells (MDSCs), which suppress T cells and alter the tumor immune microenvironment. Furthermore, activation of cytotoxic T cells with combination therapy mediated the reduction of MDSCs in tumors through the cytotoxic actions of TNF. Our data provide evidence for a close interaction between IR, T cells, and the PD-L1/PD-1 axis and establish a basis for the rational design of combination therapy with immune modulators and radiotherapy.
in vivo PD-L1 blockade
Dolina, J. S., et al. (2014). "Liver-primed CD8+ T cells suppress antiviral adaptive immunity through galectin-9-independent T-cell immunoglobulin and mucin 3 engagement of high-mobility group box 1 in mice" Hepatology 59(4): 1351-1365.
PubMed
The liver is a tolerogenic environment exploited by persistent infections, such as hepatitis B (HBV) and C (HCV) viruses. In a murine model of intravenous hepatotropic adenovirus infection, liver-primed antiviral CD8(+) T cells fail to produce proinflammatory cytokines and do not display cytolytic activity characteristic of effector CD8(+) T cells generated by infection at an extrahepatic, that is, subcutaneous, site. Importantly, liver-generated CD8(+) T cells also appear to have a T-regulatory (Treg) cell function exemplified by their ability to limit proliferation of antigen-specific T-effector (Teff ) cells in vitro and in vivo via T-cell immunoglobulin and mucin 3 (Tim-3) expressed by the CD8(+) Treg cells. Regulatory activity did not require recognition of the canonical Tim-3 ligand, galectin-9, but was dependent on CD8(+) Treg cell-surface Tim-3 binding to the alarmin, high-mobility group box 1 (HMGB-1). CONCLUSION: Virus-specific Tim-3(+) CD8(+) T cells operating through HMGB-1 recognition in the setting of acute and chronic viral infections of the liver may act to dampen hepatic T-cell responses in the liver microenvironment and, as a consequence, limit immune-mediated tissue injury or promote the establishment of persistent infections.
in vivo PD-L1 blockade
Flow Cytometry
Rutigliano, J. A., et al. (2014). "Highly pathological influenza A virus infection is associated with augmented expression of PD-1 by functionally compromised virus-specific CD8+ T cells" J Virol 88(3): 1636-1651.
PubMed
One question that continues to challenge influenza A research is why some strains of virus are so devastating compared to their more mild counterparts. We approached this question from an immunological perspective, investigating the CD8(+) T cell response in a mouse model system comparing high- and low-pathological influenza virus infections. Our findings reveal that the early (day 0 to 5) viral titer was not the determining factor in the outcome of disease. Instead, increased numbers of antigen-specific CD8(+) T cells and elevated effector function on a per-cell basis were found in the low-pathological infection and correlated with reduced illness and later-time-point (day 6 to 10) viral titer. High-pathological infection was associated with increased PD-1 expression on influenza virus-specific CD8(+) T cells, and blockade of PD-L1 in vivo led to reduced virus titers and increased CD8(+) T cell numbers in high- but not low-pathological infection, though T cell functionality was not restored. These data show that high-pathological acute influenza virus infection is associated with a dysregulated CD8(+) T cell response, which is likely caused by the more highly inflamed airway microenvironment during the early days of infection. Therapeutic approaches specifically aimed at modulating innate airway inflammation may therefore promote efficient CD8(+) T cell activity. We show that during a severe influenza virus infection, one type of immune cell, the CD8 T cell, is less abundant and less functional than in a more mild infection. This dysregulated T cell phenotype correlates with a lower rate of virus clearance in the severe infection and is partially regulated by the expression of a suppressive coreceptor called PD-1. Treatment with an antibody that blocks PD-1 improves T cell functionality and increases virus clearance.
in vivo PD-L1 blockade
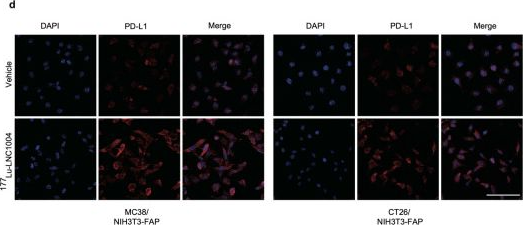
Immunofluorescence
Willimsky, G., et al. (2013). "Virus-induced hepatocellular carcinomas cause antigen-specific local tolerance" J Clin Invest 123(3): 1032-1043.
PubMed
T cell surveillance is often effective against virus-associated tumors because of their high immunogenicity. It is not clear why surveillance occasionally fails, particularly against hepatitis B virus- or hepatitis C virus-associated hepatocellular carcinoma (HCC). We established a transgenic murine model of virus-induced HCC by hepatocyte-specific adenovirus-induced activation of the oncogenic SV40 large T antigen (TAg). Adenovirus infection induced cytotoxic T lymphocytes (CTLs) targeted against the virus and TAg, leading to clearance of the infected cells. Despite the presence of functional, antigen-specific T cells, a few virus-infected cells escaped immune clearance and progressed to HCC. These cells expressed TAg at levels similar to HCC isolated from neonatal TAg-tolerant mice, suggesting that CTL clearance does not select for cells with low immunogenicity. Virus-infected mice revealed significantly greater T cell infiltration in early-stage HCC compared with that in late-stage HCC, demonstrating progressive local immune suppression through inefficient T cell infiltration. Programmed cell death protein-1 (PD-1) and its ligand PD-L1 were expressed in all TAg-specific CD8+ T cells and HCC, respectively, which contributed to local tumor-antigen-specific tolerance. Thus, we have developed a model of virus-induced HCC that may allow for a better understanding of human HCC.
in vivo PD-L1 blockade
Dietze, K. K., et al. (2013). "Combining regulatory T cell depletion and inhibitory receptor blockade improves reactivation of exhausted virus-specific CD8+ T cells and efficiently reduces chronic retroviral loads" PLoS Pathog 9(12): e1003798.
PubMed
Chronic infections with human viruses, such as HIV and HCV, or mouse viruses, such as LCMV or Friend Virus (FV), result in functional exhaustion of CD8(+) T cells. Two main mechanisms have been described that mediate this exhaustion: expression of inhibitory receptors on CD8(+) T cells and expansion of regulatory T cells (Tregs) that suppress CD8(+) T cell activity. Several studies show that blockage of one of these pathways results in reactivation of CD8(+) T cells and partial reduction in chronic viral loads. Using blocking antibodies against PD-1 ligand and Tim-3 and transgenic mice in which Tregs can be selectively ablated, we compared these two treatment strategies and combined them for the first time in a model of chronic retrovirus infection. Blocking inhibitory receptors was more efficient than transient depletion of Tregs in reactivating exhausted CD8(+) T cells and reducing viral set points. However, a combination therapy was superior to any single treatment and further augmented CD8(+) T cell responses and resulted in a sustained reduction in chronic viral loads. These results demonstrate that Tregs and inhibitory receptors are non-overlapping factors in the maintenance of chronic viral infections and that immunotherapies targeting both pathways may be a promising strategy to treat chronic infectious diseases.
in vivo PD-L1 blockade
Hafalla, J. C., et al. (2012). "The CTLA-4 and PD-1/PD-L1 inhibitory pathways independently regulate host resistance to Plasmodium-induced acute immune pathology" PLoS Pathog 8(2): e1002504.
PubMed
The balance between pro-inflammatory and regulatory immune responses in determining optimal T cell activation is vital for the successful resolution of microbial infections. This balance is maintained in part by the negative regulators of T cell activation, CTLA-4 and PD-1/PD-L, which dampen effector responses during chronic infections. However, their role in acute infections, such as malaria, remains less clear. In this study, we determined the contribution of CTLA-4 and PD-1/PD-L to the regulation of T cell responses during Plasmodium berghei ANKA (PbA)-induced experimental cerebral malaria (ECM) in susceptible (C57BL/6) and resistant (BALB/c) mice. We found that the expression of CTLA-4 and PD-1 on T cells correlates with the extent of pro-inflammatory responses induced during PbA infection, being higher in C57BL/6 than in BALB/c mice. Thus, ECM develops despite high levels of expression of these inhibitory receptors. However, antibody-mediated blockade of either the CTLA-4 or PD-1/PD-L1, but not the PD-1/PD-L2, pathways during PbA-infection in ECM-resistant BALB/c mice resulted in higher levels of T cell activation, enhanced IFN-gamma production, increased intravascular arrest of both parasitised erythrocytes and CD8(+) T cells to the brain, and augmented incidence of ECM. Thus, in ECM-resistant BALB/c mice, CTLA-4 and PD-1/PD-L1 represent essential, independent and non-redundant pathways for maintaining T cell homeostasis during a virulent malaria infection. Moreover, neutralisation of IFN-gamma or depletion of CD8(+) T cells during PbA infection was shown to reverse the pathologic effects of regulatory pathway blockade, highlighting that the aetiology of ECM in the BALB/c mice is similar to that in C57BL/6 mice. In summary, our results underscore the differential and complex regulation that governs immune responses to malaria parasites.
Immunohistochemistry (frozen)
Immunofluorescence
Riella, L. V., et al. (2011). "Essential role of PDL1 expression on nonhematopoietic donor cells in acquired tolerance to vascularized cardiac allografts" Am J Transplant 11(4): 832-840.
PubMed
The PD1:PDL1 pathway is an essential negative costimulatory pathway that plays a key role in regulating the alloimune response. PDL1 is expressed not only on antigen-presenting cells (APCs) but also cardiac endothelium. In this study, we investigated the importance of PDL1 expression on donor cardiac allograft in acquired transplantation tolerance in a fully MHC-mismatched model. We generated PDL1 chimeric mice on B6 background that expressed PDL1 on either hematopoietic cells or nonhematopoietic cells of the heart. Sham animals were used as controls. These hearts were then transplanted into BALB/c recipients and treated with CTLA4-Ig to induce tolerance. Cardiac endothelium showed significant expression of PDL1, which was upregulated upon transplantation. While the absence of PDL1 on hematopoietic cells of the heart resulted in delayed rejection and prevented long-term tolerance in most but not all recipients, we observed an accelerated and early graft rejection of all donor allografts that lacked PDL1 on the endothelium. Moreover, PDL1-deficient endothelium hearts had significant higher frequency of IFN-gamma-producing alloreactive cells as well as higher frequency of CD8(+) effector T cells. These findings demonstrate that PDL1 expression mainly on donor endothelium is functionally important in a fully allogeneic mismatched model for the induction of cardiac allograft tolerance
in vivo PD-L1 blockade
Zhang, L., et al. (2009). "PD-1/PD-L1 interactions inhibit antitumor immune responses in a murine acute myeloid leukemia model" Blood 114(8): 1545-1552.
PubMed
Negative regulatory mechanisms within the solid tumor microenvironment inhibit antitumor T-cell function, leading to evasion from immune attack. One inhibitory mechanism is up-regulation of programmed death-ligand 1 (PD-L1) expressed on tumor or stromal cells which binds to programmed death-1 (PD-1) on activated T cells. PD-1/PD-L1 engagement results in diminished antitumor T-cell responses and correlates with poor outcome in murine and human solid cancers. In contrast to available data in solid tumors, little is known regarding involvement of the PD-1/PD-L1 pathway in immune escape by hematopoietic cancers, such as acute myeloid leukemia (AML). To investigate this hypothesis, we used the murine leukemia, C1498. When transferred intravenously, C1498 cells grew progressively and apparently evaded immune destruction. Low levels of PD-L1 expression were found on C1498 cells grown in vitro. However, PD-L1 expression was up-regulated on C1498 cells when grown in vivo. PD-1(-/-) mice challenged with C1498 cells generated augmented antitumor T-cell responses, showed decreased AML burden in the blood and other organs, and survived significantly longer than did wild-type mice. Similar results were obtained with a PD-L1 blocking antibody. These data suggest the importance of the PD-1/PD-L1 pathway in immune evasion by a hematologic malignancy, providing a rationale for clinical trials targeting this pathway in leukemia patients.
Product Citations
-
-
Cancer Research
Potentiating cancer immunotherapies with modular albumin-hitchhiking nanobody-STING agonist conjugates.
In Nat Biomed Eng on 11 June 2025 by Kimmel, B. R., Arora, K., et al.
PubMed
The enhancement of antitumour immunity via agonists of the stimulator of interferon genes (STING) pathway is limited by pharmacological barriers. Here we show that the covalent conjugation of a STING agonist to anti-albumin nanobodies via site-selective bioconjugation chemistries prolongs the circulation of the agonist in the blood and increases its accumulation in tumour tissue, stimulating innate immune programmes that increased the infiltration of activated natural killer cells and T cells, which potently inhibited the growth of mouse tumours. The technology is modular, as demonstrated by the recombinant integration of a second nanobody domain targeting programmed death-ligand 1 (PD-L1), which further increased the accumulation of the agonist in tumours while blocking immunosuppressive PD-1/PD-L1 interactions. The bivalent nanobody-STING agonist conjugate stimulated robust antigen-specific T-cell responses and long-lasting immunological memory and conferred enhanced therapeutic efficacy. It was also effective as a neoadjuvant treatment to adoptive T-cell therapy. As a modular approach, hitchhiking STING agonists on serum albumin may serve as a broadly applicable strategy for augmenting the potency of systemically administered cancer immunotherapies.
-
-
-
Cancer Research
-
Immunology and Microbiology
Glutamate transporter SLC1A6 promotes resistance to immunotherapy in cancer.
In Cancer Immunol Immunother on 7 June 2025 by Li, C., Lin, Y., et al.
PubMed
Resistance to immune checkpoint inhibitors remains a significant challenge in the treatment of cancer. Emerging evidence suggests that metabolic reprogramming plays a crucial role in tumor metabolism and progression. Our study strived to investigate the role and underlying mechanisms of the glutamate transporter SLC1A6 in resistance to immunotherapy of cancer.
-
-
-
Cancer Research
Oral ENPP1 inhibitor designed using generative AI as next generation STING modulator for solid tumors.
In Nat Commun on 23 May 2025 by Pu, C., Cui, H., et al.
PubMed
Despite the STING-type-I interferon pathway playing a key role in effective anti-tumor immunity, the therapeutic benefit of direct STING agonists appears limited. In this study, we use several artificial intelligence techniques and patient-based multi-omics data to show that Ectonucleotide Pyrophosphatase/Phosphodiesterase 1 (ENPP1), which hydrolyzes STING-activating cyclic GMP-AMP (cGAMP), is a safer and more effective STING-modulating target than direct STING agonism in multiple solid tumors. We then leverage our generative chemistry artificial intelligence-based drug design platform to facilitate the design of ISM5939, an orally bioavailable ENPP1-selective inhibitor capable of stabilizing extracellular cGAMP and activating bystander antigen-presenting cells without inducing either toxic inflammatory cytokine release or tumor-infiltrating T-cell death. In murine syngeneic models across cancer types, ISM5939 synergizes with targeting the PD-1/PD-L1 axis and chemotherapy in suppressing tumor growth with good tolerance. Our findings provide evidence supporting ENPP1 as an innate immune checkpoint across solid tumors and reports an AI design-aided ENPP1 inhibitor, ISM5939, as a cutting-edge STING modulator for cancer therapy, paving a path for immunotherapy advancements.
-
-
-
Cardiovascular biology
Opposing role for myeloid and smooth muscle cell STING in pulmonary hypertension.
In JCI Insight on 22 May 2025 by Pham, A. T., Virk, S., et al.
PubMed
There is an emerging role for stimulator of interferon genes (STING) signaling in pulmonary hypertension (PH) development. Related to this, prior research has demonstrated the relevance of immune checkpoint protein programmed death ligand 1 (PD-L1) expression by immunoregulatory myeloid cells in PH. However, there remains a need to elucidate the cell-specific role of STING expression, and the STING/PD-L1 signaling axis in PH, before readily available disease-modifying therapies can be applied for patients with the disease. Here, through generation of bone marrow chimeric mice, we show that STING-/- mice receiving WT bone marrow were protected against PH secondary to chronic hypoxia. We further demonstrate a cellular dichotomous role for STING in PH development, with STING expression by smooth muscle cells contributing to PH and its activation on myeloid cells being pivotal in severe disease prevention. Finally, we provide evidence that a STING/PD-L1 axis modulates disease severity, suggesting the potential for future therapeutic applications. Overall, these data provide evidence of STING's involvement in PH in a cell-specific manner, establishing the biologic plausibility of developing cell-targeted STING-related therapies for PH.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
Novel Pt@PCN-Cu-induced cuproptosis amplifies αPD-L1 immunotherapy in pancreatic ductal adenocarcinoma through mitochondrial HK2-mediated PD-L1 upregulation.
In J Exp Clin Cancer Res on 17 May 2025 by Wang, P., Guo, W., et al.
PubMed
Copper accumulation triggers mitochondrial-driven cell death, known as cuproptosis, offering a promising mechanism for targeted cancer therapy. Recent studies have highlighted the critical role of intratumoral copper levels in regulating the expression of programmed cell death ligand-1 (PD-L1), suggesting that copper-induced cuproptosis not only enhances cancer cell death but may also amplify the effects of anti-PD-L1 antibodies (αPD-L1). However, in tumors where monotherapy with αPD-L1 shows limited efficacy, particularly in pancreatic ductal adenocarcinoma (PDAC), the role of copper-induced cuproptosis in enhancing αPD-L1 treatment efficacy and its underlying mechanisms remain unclear. Meanwhile, inadequate tumor drug accumulation and glycolysis significantly restrict the efficacy of cuproptosis. To address these challenges, we have synthesized a novel nanozyme, Pt@PCN-Cu, designed to stabilize intracellular copper accumulation and effectively induce cuproptosis. Additionally, we aim to determine whether this strong induction of cuproptosis can synergize with αPD-L1 to enhance cancer therapy, ultimately paving the way for novel strategies to improve PDAC treatment.
-
-
-
Cancer Research
-
Immunology and Microbiology
STAT5 and STAT3 balance shapes dendritic cell function and tumour immunity.
In Nature on 14 May 2025 by Zhou, J., Tison, K., et al.
PubMed
Immune checkpoint blockade (ICB) has transformed cancer therapy1,2. The efficacy of immunotherapy depends on dendritic cell-mediated tumour antigen presentation, T cell priming and activation3,4. However, the relationship between the key transcription factors in dendritic cells and ICB efficacy remains unknown. Here we found that ICB reprograms the interplay between the STAT3 and STAT5 transcriptional pathways in dendritic cells, thereby activating T cell immunity and enabling ICB efficacy. Mechanistically, STAT3 restrained the JAK2 and STAT5 transcriptional pathway, determining the fate of dendritic cell function. As STAT3 is often activated in the tumour microenvironment5, we developed two distinct PROTAC (proteolysis-targeting chimera) degraders of STAT3, SD-36 and SD-2301. STAT3 degraders effectively degraded STAT3 in dendritic cells and reprogrammed the dendritic cell-transcriptional network towards immunogenicity. Furthermore, STAT3 degrader monotherapy was efficacious in treatment of advanced tumours and ICB-resistant tumours without toxicity in mice. Thus, the crosstalk between STAT3 and STAT5 transcriptional pathways determines the dendritic cell phenotype in the tumour microenvironment and STAT3 degraders hold promise for cancer immunotherapy.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
Intrapleural dual blockade of IL-6 and PD-L1 reprograms CAF dynamics and the tumor microenvironment in lung cancer-associated malignant pleural effusion.
In Respir Res on 10 May 2025 by Cheng, Q., Zuo, X., et al.
PubMed
Malignant pleural effusion (MPE) is a severe complication in lung cancer, characterized by an immunosuppressive tumor microenvironment (TME) and limited therapeutic options. This study investigates the role of IL-6 in regulating immune suppression and tumor progression in MPE and evaluates the efficacy of dual IL-6 and PD-L1 blockade.
-
-
-
Biochemistry and Molecular biology
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
Metabolic reprogramming nanomedicine potentiates colon cancer sonodynamic immunotherapy by inhibiting the CD39/CD73/ADO pathway.
In Acta Pharm Sin B on 1 May 2025 by Zhang, Y., Jin, W., et al.
PubMed
Sonodynamic therapy (SDT) can potentially induce immunogenic cell death in tumor cells, leading to the release of ATP, and facilitating the initiation of an immune response. Nevertheless, the enzymes CD39 and CD73 can swiftly convert ATP into immunosuppressive adenosine (ADO), resulting in an immunosuppressive tumor microenvironment (TME). This study introduced a nanomedicine (QD/POM1@NP@M) engineered to reprogram TME by modulating the CD39/CD73/ADO pathway. The nanomedicine encapsulated sonosensitizers silver sulfide quantum dots, and the CD39 inhibitor POM1, while also incorporating homologous tumor cell membranes to enhance targeting capabilities. This integrated approach, on the one hand, stimulates the release of ATP via SDT, thereby initiating the immune response. In addition, it reduced the accumulation of ADO by inhibiting CD39 activity, which ameliorated the immunosuppressive TME. Upon administration, the nanomedicine demonstrated substantial anti-tumor efficacy by facilitating the infiltration of anti-tumor immune cells, while reducing the immunosuppressive cells. This modulation effectively transformed the TME from an immunologically "cold" state to a "hot" state. Furthermore, combined with the checkpoint inhibitor α-PDL1, the nanomedicine augmented systemic anti-tumor immunity and promoted the establishment of long-term immune memory. This study provides an innovative strategy for combining non-invasive SDT and ATP-driven immunotherapy, offering new ideas for future cancer treatment.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Comprehensive analysis of UPK3B as a marker for prognosis and immunity in pancreatic adenocarcinoma.
In Sci Rep on 13 April 2025 by Jian, Z., Pan, T., et al.
PubMed
The low immunogenicity of pancreatic cancer inhibits effective antitumor immune responses, primarily due to the immune evasion mediated by low expression of the major histocompatibility complex (MHC). Through comprehensive analysis, our study identifies UPK3B as a gene closely associated with low MHC expression and low immunogenicity in pancreatic cancer. UPK3B has been reported as a marker of primary mesothelial cells, mature epicardium and promotes extracellular matrix signaling. However, the role of UPK3B in pancreatic cancer remain unclear. We found that UPK3B is highly predictive of overall survival (OS) in patients with pancreatic ductal adenocarcinoma (PDAC) and is significantly related to clinical features, immune cell infiltration, and response to immune checkpoint inhibitor (ICI) therapy. Gene enrichment analysis revealed significant downregulation of immune regulatory and BCR signaling pathways in the UPK3B high-expression group. Additionally, UPK3B is positively correlated with immunosuppressive cells, suggesting that high UPK3B expression may inhibit antitumor immune responses by promoting low MHC expression. UPK3B is also positively correlated with immune checkpoints, indicating that tumors with high UPK3B expression may not benefit from ICI therapy. Therefore, UPK3B may serve as a novel biomarker and therapeutic target for pancreatic cancer.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Targeting B7-H3 inhibition-induced activation of fatty acid synthesis boosts anti-B7-H3 immunotherapy in triple-negative breast cancer.
In J Immunother Cancer on 12 April 2025 by Jiang, Y., Qian, Z., et al.
PubMed
Triple-negative breast cancer (TNBC) is the most malignant breast cancer, highlighting the need for effective immunotherapeutic targets. The immune checkpoint molecule B7-H3 has recently gained attention as a promising therapeutic target due to its pivotal role in promoting tumorigenesis and cancer progression. However, the therapeutic impact of B7-H3 inhibitors (B7-H3i) remains unclear.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Combined anti-PD-L1 and anti-VEGFR2 therapy promotes the antitumor immune response in GBM by reprogramming tumor microenvironment.
In Cell Death Discov on 3 April 2025 by Yao, L., Wang, H., et al.
PubMed
Inhibitors of programmed cell death ligand 1 (PD-L1) and vascular endothelial growth factor receptor 2 (VEGFR2) are commonly used in the clinic, but they are beneficial for only a minority of glioblastoma multiforme (GBM) patients. GBM has significant immunosuppressive properties, and there are many immunosuppressive cells and dysfunctional effector T cells in the tumor microenvironment (TME), which is one of the important reasons for the failure of clinical treatment of GBM. Here, we have identified P21 activated kinase 4 (PAK4) as a pivotal immune suppressor in the TME. PAK4 is a threonine protein kinase, and PAK4 knockdown attenuates vascular abnormalities and promotes T-cell infiltration. In this study, our results showed that the expression of PAK4 was significantly downregulated after VEGFR2 knockdown. Next, we constructed a coculture system of CD8+ T cells and GBM cells. Our findings showed that combined anti-PD-L1 and anti-VEGFR2 therapy can regulate the TME and inhibit GBM cells' immune escape; overexpression of PAK4 can reverse this effect. Finally, we tested the combination therapy in mouse intracranial graft tumor models and found that combination therapy can prolong mouse survival. These findings suggest that anti-VEGFR2 therapy can downregulate PAK4, reprogram the TME by increasing cytotoxic CD8+ T cells infiltration and activation, and enhance the therapeutic effect of anti-PD-L1 therapy on GBM cells.
-
-
-
Cancer Research
-
Immunology and Microbiology
Intermittent fasting reverses T cell lymphopenia via inosine to mitigate brain tumors
In Research Square on 18 March 2025 by Wang, Y., Ye, C., et al.
-
-
-
Biochemistry and Molecular biology
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
Interleukin-16 enhances anti-tumor immune responses by establishing a Th1 cell-macrophage crosstalk through reprogramming glutamine metabolism in mice.
In Nat Commun on 10 March 2025 by Wen, Z., Liu, T., et al.
PubMed
Overcoming immunosuppression in the tumor microenvironment (TME) is crucial for developing novel cancer immunotherapies. Here, we report that IL-16 administration enhances the polarization of T helper 1 (Th1) cells by inhibiting glutamine catabolism through the downregulation of glutaminase in CD4+ T cells and increases the production of Th1 effector cytokine IFN-γ, thus improving anti-tumor immune responses. Moreover, we find that establishing an IL-16-dependent, Th1-dominant TME relies on mast cell-produced histamine and results in the increased expression of the CXCR3 ligands in tumor-associated macrophages (TAM), thereby improving the therapeutic effectiveness of immune checkpoint blockade (ICB). Cancer patients exhibit impaired production of IL-16, which correlates with poorer prognosis. Additionally, low IL-16 production is associated with unresponsiveness to immunotherapy in cancer patients. Collectively, our findings provided new insights into the biological function of IL-16, emphasizing its potential clinical significance as a therapeutic approach to augment anti-tumor immunity and sensitize ICB-based cancer immunotherapy.
-
-
-
Cancer Research
-
Immunology and Microbiology
Targeted nanoparticle delivery system for tumor-associated macrophage reprogramming to enhance TNBC therapy.
In Cell Biol Toxicol on 8 March 2025 by Dong, X., Wang, X., et al.
PubMed
Triple-negative breast cancer (TNBC) poses as a daunting and intricate manifestation of breast cancer, highlighted by few treatment options and a poor outlook. The crucial element in fostering tumor growth and immune resistance is the polarization of tumor-associated macrophages (TAMs) into the M2 state within the tumor microenvironment (TME). To address this, we developed M2 targeting peptide-chitosan-curcumin nanoparticles (M2pep-Cs-Cur NPs), a targeted delivery system utilizing chitosan (Cs) as a carrier, curcumin (Cur) as a therapeutic agent, and targeting peptides for specificity. These NPs effectively inhibited TNBC cell proliferation (~ 70%) and invasion (~ 70%), while increasing the responsiveness of tumors to anti-PD-L1 treatment (~ 50% survival enhancement) in vitro and in vivo. Bioinformatics analysis suggested that Cur modulates TAM polarization by influencing key genes such as COX-2, offering insights into its underlying mechanisms. This study highlights the potential of M2pep-Cs-Cur NPs to reverse M2 polarization in TAMs, providing a promising targeted therapeutic strategy to overcome immunotherapy resistance and improve TNBC outcomes.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
PRMT3 drives PD-L1-mediated immune escape through activating PDHK1-regulated glycolysis in hepatocellular carcinoma.
In Cell Death Dis on 6 March 2025 by Ding, C. H., Yan, F. Z., et al.
PubMed
Aberrant expression of programmed death ligand-1 (PD-L1) facilitates tumor immune evasion. Protein arginine methyltransferase 3 (PRMT3), a member of type I PRMT family, mediates asymmetric dimethylarginine (ADMA) modification of various substrate proteins. This study investigates the role of PRMT3 in PD-L1-associated tumor immunosuppression in hepatocellular carcinoma (HCC). Hepatocyte-specific knockout of Prmt3 significantly suppressed HCC progression in DEN-CCL4-treated mice. Knockout of Prmt3 in HCC cells markedly increased CD8+ T cell infiltration, and reduced lactate production in tumors. PRMT3 interacted with pyruvate dehydrogenase kinase 1 (PDHK1), asymmetric dimethylation of PDHK1 at arginine 363 and 368 residues and increased its kinase activity. The R363/368 K mutant or inhibition of PDHK1 by JX06 blocked the effect of PRMT3 on lactate production. JX06 treatment also attenuated the tumor-promoting role of PRMT3 in HCC in vitro and in vivo. Furthermore, RNA-seq analysis revealed that knockout of PRMT3 downregulates the tumor-associated immune checkpoint, PD-L1, in tumor tissues. Chromatin immunoprecipitation (ChIP) assay demonstrated that PRMT3 promotes lactate-induced PD-L1 expression by enhancing the direct binding of histone H3 lysine 18 lactylation (H3K18la) to the PD-L1 promoter. Tissue microarray analysis showed a positive correlation between PRMT3 and PD-L1 expression in HCC patients. Anti-PD-L1 treatment reversed PRMT3-induced tumor growth and restored CD8+ T cell infiltration. Our research links PRMT3-mediated metabolic reprogramming and immune evasion, revealing that the PRMT3-PDHK1-lactate-PD-L1 axis may be a potential target for improving the efficacy of immunotherapy in HCC.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
A covalent peptide-based lysosome-targeting protein degradation platform for cancer immunotherapy.
In Nat Commun on 6 February 2025 by Xiao, Y., He, Z., et al.
PubMed
The lysosome-targeting chimera (LYTAC) strategy provided a very powerful tool for the degradation of membrane proteins. However, the synthesis of LYTACs, antibody-small molecule conjugates, is challenging. The ability of antibody-based LYTACs to penetrate solid tumor is limited as well, especially to cross the blood-brain barrier (BBB). Here, we propose a covalent chimeric peptide-based targeted degradation platform (Pep-TACs) by introducing a long flexible aryl sulfonyl fluoride group, which allows proximity-enabled cross-linking upon binding with the protein of interest. The Pep-TACs platform facilitates the degradation of target proteins through the mechanism of recycling transferrin receptor (TFRC)-mediated lysosomal targeted endocytosis. Biological experiments demonstrate that covalent Pep-TACs can significantly degrade the expression of PD-L1 on tumor cells, dendritic cells and macrophages, especially under acidic conditions, and markedly enhance the function of T cells and tumor phagocytosis by macrophages. Furthermore, both in anti-PD-1-responsive and -resistant tumor models, the Pep-TACs exert significant anti-tumor immune response. It is noteworthy that Pep-TACs can cross the BBB and prolong the survival of mice with in situ brain tumor. As a proof-of-concept, this study introduces a modular TFRC-based covalent peptide degradation platform for the degradation of membrane protein, and especially for the immunotherapy of brain tumors.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Biochemistry and Molecular biology
-
Cell Biology
Plant-nanoparticles enhance anti-PD-L1 efficacy by shaping human commensal microbiota metabolites.
In Nat Commun on 3 February 2025 by Teng, Y., Luo, C., et al.
PubMed
Diet has emerged as a key impact factor for gut microbiota function. However, the complexity of dietary components makes it difficult to predict specific outcomes. Here we investigate the impact of plant-derived nanoparticles (PNP) on gut microbiota and metabolites in context of cancer immunotherapy with the humanized gnotobiotic mouse model. Specifically, we show that ginger-derived exosome-like nanoparticle (GELN) preferentially taken up by Lachnospiraceae and Lactobacillaceae mediated by digalactosyldiacylglycerol (DGDG) and glycine, respectively. We further demonstrate that GELN aly-miR159a-3p enhances anti-PD-L1 therapy in melanoma by inhibiting the expression of recipient bacterial phospholipase C (PLC) and increases the accumulation of docosahexaenoic acid (DHA). An increased level of circulating DHA inhibits PD-L1 expression in tumor cells by binding the PD-L1 promoter and subsequently prevents c-myc-initiated transcription of PD-L1. Colonization of germ-free male mice with gut bacteria from anti-PD-L1 non-responding patients supplemented with DHA enhances the efficacy of anti-PD-L1 therapy compared to controls. Our findings reveal a previously unknown mechanistic impact of PNP on human tumor immunotherapy by modulating gut bacterial metabolic pathways.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
AIEgen-self-assembled nanoparticles with anti-PD-L1 antibody functionalization realize enhanced synergistic photodynamic therapy and immunotherapy against malignant melanoma.
In Mater Today Bio on 1 February 2025 by Li, L., Xu, Q., et al.
PubMed
Immune checkpoint inhibitors (ICIs) become integral in clinical practice, yet their application in cancer therapy is constrained by low overall response rates and the primary resistance of cancers to ICIs. Herein, this study proposes aggregation-induced emission (AIE)-based nanoparticles (NPs) for a more effective and synergistic approach combining immunotherapy and photodynamic therapy (PDT) to achieve higher responses than anti-PD-L1 monotherapy. The TBP@aPD-L1 NPs are constructed by functionalizing azide group-modified TBP-2 (TBP-N3) with anti-PD-L1 antibodies via the DBCO-S-S-PEG2000-COOH linker. The anti-PD-L1 target the tumor cells and promote the TBP-N3 accumulation in tumors for enhanced PDT. Notably, the TBP-N3, featuring aggregation-induced emission, boosts reactive oxygen species (ROS) generation through both type I and type II processes for enhanced PDT. The TBP@aPD-L1-mediated PDT induces more powerful effects of direct tumor cell-killing and further elicits effective immunogenic cell death (ICD), which exerts anti-tumor immunity by activating T cells for ICI treatment and reshapes the tumor immune microenvironment (TIME), thereby enhancing the efficacy of PD-L1 blockade of anti-PD-L1. Consequently, TBP@aPD-L1 NPs demonstrated significantly enhanced inhibition of tumor growth in the mouse model of malignant melanoma (MM). Our NPs act as a facile and effective drug delivery platform for enhanced immunotherapy combined with enhanced PDT in treating MM.
-
-
-
Cancer Research
-
Immunology and Microbiology
Cholesterol Targeted Catalytic Hydrogel Fueled by Tumor Debris can Enhance Microwave Ablation Therapy and Anti-Tumor Immune Response.
In Adv Sci (Weinh) on 1 February 2025 by Shen, L., Yang, Z., et al.
PubMed
The immunosuppressive residual tumor microenvironment (IRTM) is a key factor in the high recurrence and metastasis rates of hepatocellular carcinoma (HCC) after microwave ablation (MWA). Cholesterol-rich tumor fragments significantly contribute to IRTM deterioration. This study developed a cholesterol-targeted catalytic hydrogel, DA-COD-OD-HCS, to enhance the synergy between MWA and immune checkpoint inhibitors (ICIs) for HCC treatment. Cholesterol oxidase (COD), modified with dimethyl maleic anhydride (DA) for release in acidic IRTM, is used to degrade cholesterol. Oxydextran (OD) and hemin-chitosan (HCS) formed a dual network gel, ensuring long-term fixation of COD and hemin in the IRTM post-MWA. In both in vitro and in vivo HCC models, DA-COD-OD-HCS effectively released COD, degraded cholesterol, and induced tumor cell ferroptosis, enhancing the antitumor immune response. Combined with anti-PD-L1 immunotherapy, this strategy inhibited primary tumor growth and distant metastases, without side effects on adjacent tissues. This work highlights that cholesterol-targeting catalytic hydrogels fueled by tumor debris can significantly improve the efficacy of MWA and ICIs, offering a novel therapeutic approach for HCC.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Chiral polypeptide hydrogels regulating local immune microenvironment and anti-tumor immune response.
In Nat Commun on 31 January 2025 by Ding, J., Wang, T., et al.
PubMed
The impact of chirality on immune response has attracted great interest in cancer vaccine research recently. However, the study of chiral synthetic polypeptide hydrogels as cancer vaccines as well as of the impact of biomaterials themselves for antitumor immunotherapy has rarely been reported. Here, we show the key role of residue chirality of polypeptide hydrogels in antitumor immunity and local immune microenvironment regulation. Compared to poly(γ-ethyl-L-glutamate)-based hydrogels (L-Gel), poly(γ-ethyl-D-glutamate)-based hydrogels (D-Gel) induces enhanced level of immune cell infiltration. However, D-Gel causes higher levels of suppressive markers on antigen-presenting cells and even induces stronger T cell exhaustion than L-Gel. Finally, D-Gel establishes a local chronic inflammatory and immunosuppressive microenvironment and shows insufficient anti-tumor effects. Conversely, the milder host immune responses induced by L-Gel leads to more effective tumor inhibition. This study provides insights on the role of residue chirality in the regulation of local immune microenvironment and affecting antitumor immune response.
-