Chronic lung diseases such as emphysema are shaped not only by inflammation, but by persistent and dysregulated interactions between immune cells, stromal niches, and epithelial stem cell populations. While tissue-resident lymphocytes (TRLs) play a critical role in antiviral defense at barrier surfaces, their long-term presence may come at a cost to tissue repair and regeneration. In a study published in
Immunity Wang et al. combine human lung single-cell profiling, genetically engineered mouse models, and immune–epithelial organoid systems to uncover how aberrant tissue niches potentiate resident lymphocytes to suppress alveolar stem cell renewal. Their work provides a mechanistic framework linking immune residency, interferon signaling, and progressive epithelial loss in emphysema.
Defining a Stromal Niche for Tissue-Resident Lymphocytes
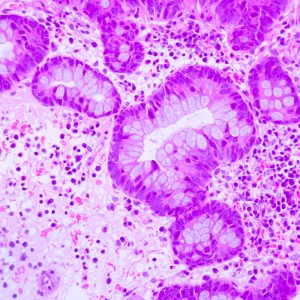
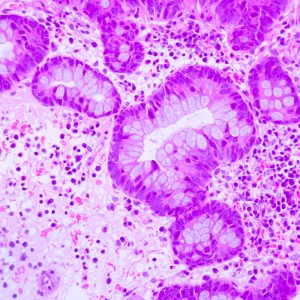
To begin establishing the immune landscape of emphysema, the authors first performed single-cell RNA sequencing of human lung explants from emphysema patients and age-matched controls. These analyses revealed a marked expansion of CD3⁺ tissue-resident lymphocytes expressing canonical residency markers, including CD69, CD44, and IL7R, particularly within alveolar regions. Pathway analysis showed that TRLs in emphysema lungs were enriched for antiviral and interferon-associated signaling, with TRLs identified as the primary source of IFNγ.
Using complementary C57BL/6-based murine models, the researchers identified a stromal niche that supports TRL maintenance in the lung adventitia. Gli1⁺ fibroblasts were shown to produce IL-7 in response to hedgehog signaling, creating a localized survival and expansion signal for resident lymphocytes.
Importantly, this niche is modulated by HHIP, a disease-associated gene downregulated in emphysema. Stromal-specific loss of HHIP resulted in exaggerated IL-7 production, expansion of TRLs, and their redistribution from adventitial regions into the alveolar space.
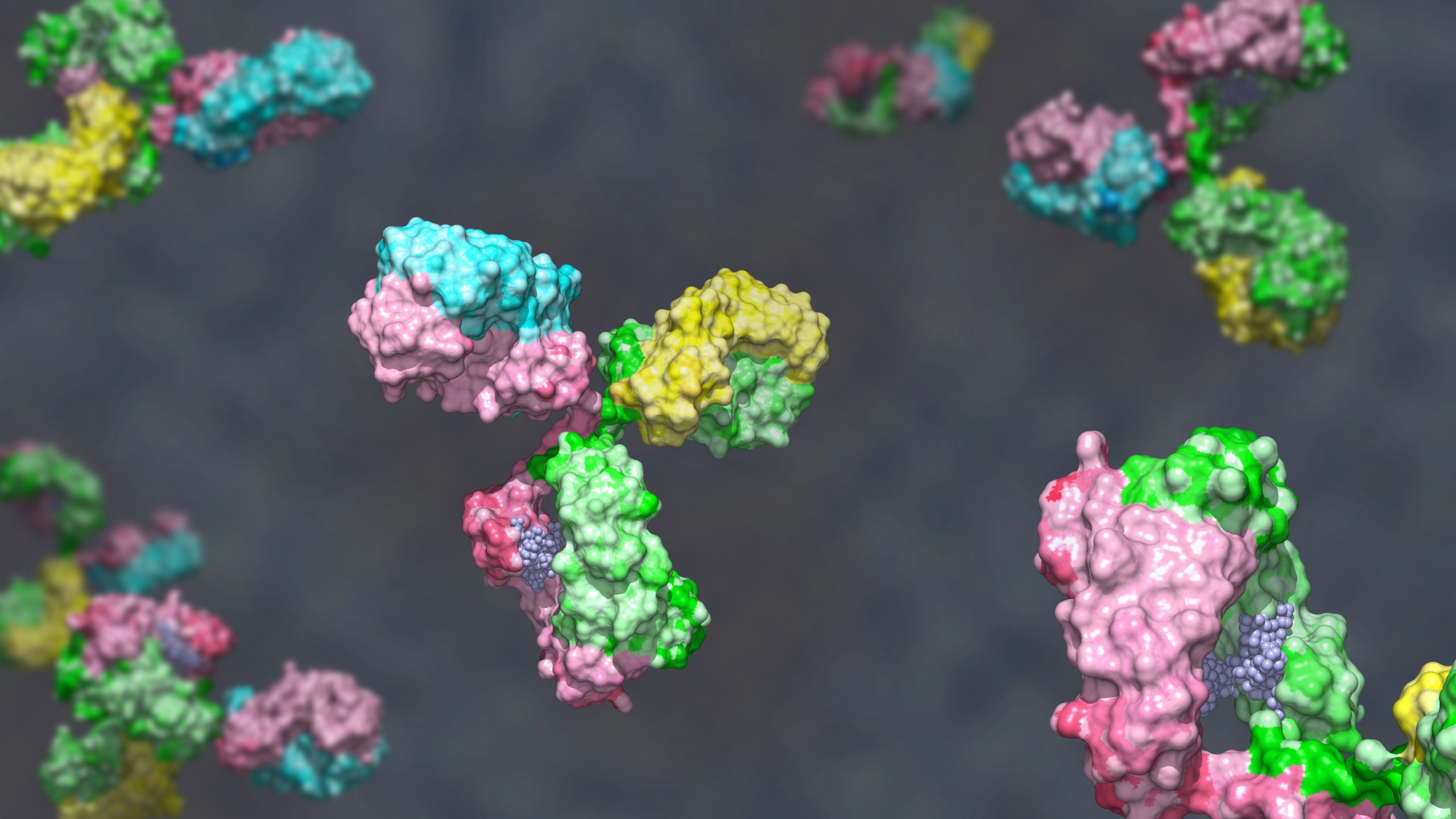
This portion of the author’s work used the following antibodies for blocking and depletion of T cells
in vivo:
Immune–Epithelial Crosstalk Revealed by Organoid Models
To directly test how expanded TRLs affect epithelial regeneration, Wang et al. developed immune–epithelial organoid systems that enabled controlled paracrine interactions between lymphocytes and alveolar type 2 (AT2) stem cells. In murine AT2 organoids, co-culture with TRLs significantly suppressed organoid growth, an effect that was recapitulated by recombinant IFNγ treatment.
Crucially, neutralization of IFNγ using blocking antibodies partially rescued AT2 proliferation both
in vitro and
in vivo, demonstrating that TRL-derived IFNγ is a key mediator of epithelial suppression. Parallel experiments targeting IL-7R similarly limited TRL expansion and mitigated emphysematous changes following viral challenge. These functional studies establish IFNγ as both necessary and sufficient to drive alveolar stem cell loss in the context of chronic immune residency.
This portion of the author’s work used the following antibodies in organoid-based AT2 assays:
Translational Relevance and Antibody-Enabled Mechanistic Insight
By combining human lung profiling with immune–epithelial organoid systems and
in vivo perturbation, this study demonstrates how tissue-resident immunity can actively reshape regenerative capacity in chronic disease. The ability to isolate specific immune signals within complex microenvironments was central to uncovering the IFNγ-dependent suppression of alveolar stem cells described here. Bio X Cell antibodies were used to selectively block IFNγ and IL-7R signaling across organoid cultures and animal models, enabling direct tests of necessity and reversibility. These experiments highlight how well-characterized, endotoxin-controlled antibodies support reproducible immune modulation in demanding systems and reinforce their value in studies aimed at dissecting tissue-specific immune pathology and evaluating targeted intervention strategies.
 Chronic lung diseases such as emphysema are shaped not only by inflammation, but by persistent and dysregulated interactions between immune cells, stromal niches, and epithelial stem cell populations. While tissue-resident lymphocytes (TRLs) play a critical role in antiviral defense at barrier surfaces, their long-term presence may come at a cost to tissue repair and regeneration. In a study published in Immunity Wang et al. combine human lung single-cell profiling, genetically engineered mouse models, and immune–epithelial organoid systems to uncover how aberrant tissue niches potentiate resident lymphocytes to suppress alveolar stem cell renewal. Their work provides a mechanistic framework linking immune residency, interferon signaling, and progressive epithelial loss in emphysema.
Chronic lung diseases such as emphysema are shaped not only by inflammation, but by persistent and dysregulated interactions between immune cells, stromal niches, and epithelial stem cell populations. While tissue-resident lymphocytes (TRLs) play a critical role in antiviral defense at barrier surfaces, their long-term presence may come at a cost to tissue repair and regeneration. In a study published in Immunity Wang et al. combine human lung single-cell profiling, genetically engineered mouse models, and immune–epithelial organoid systems to uncover how aberrant tissue niches potentiate resident lymphocytes to suppress alveolar stem cell renewal. Their work provides a mechanistic framework linking immune residency, interferon signaling, and progressive epithelial loss in emphysema.