Pancreatic ductal adenocarcinoma (PDAC) is one of the most lethal cancers, driven in part by a uniquely immunosuppressive tumor microenvironment. Despite the presence of PD-L1 expression in nearly one-third of PDAC tumors, immune checkpoint therapies such as anti-PD-1 antibodies have shown limited clinical success. A study published in
Cancers (
Holokai et al. 2020) applied a stepwise mouse-to-human workflow that integrates orthotopic mouse models with matched mouse and patient-derived organoid–immune cell co-cultures. This parallel approach revealed that resistance to PD-1 blockade is conserved across species and is driven by suppressive myeloid biology rather than loss of PD-1/PD-L1 engagement, providing a translational framework for prioritizing immune-modulatory combinations before clinical testing.
Background
Tumor cells in PDAC evade immune surveillance through both intrinsic checkpoint pathways and extrinsic immunosuppressive cell populations. While PD-L1 can inhibit CD8⁺ T cell effector function via PD-1 binding, multiple redundant suppressive mechanisms are also active. Myeloid-derived suppressor cells (MDSCs), particularly the polymorphonuclear subset (PMN-MDSCs), are known to interfere with T cell proliferation and activity by depleting amino acids such as L-arginine and generating reactive oxygen species. Their accumulation has been documented in early lesions and maintained throughout tumor progression. In both human and murine systems, high PMN-MDSC levels correlate with reduced CD8⁺ T cell responses and poor prognosis.
A Dual-Targeting Strategy
To interrogate both PD-L1–mediated T cell suppression and the immunosuppressive influence of PMN-MDSCs in a physiologically relevant setting, the study authors developed matched human and murine organoid models co-cultured with immune cells. These systems enabled direct evaluation of therapeutic antibodies and their effects on T cell activation in the context of suppressive myeloid cells. Among the reagents tested, Bio X Cell’s
InVivoPlus™ anti-mouse PD-1 antibody (
Catalog #BP0146) was used to block PD-1 signaling in 7 days post-orthotopic transplantation C57BL/6 mice, revealing that PD-L1 blockade alone was insufficient to restore full cytotoxic function in the presence of active PMN-MDSCs. Only when PMN-MDSCs were depleted did CD8⁺ T cell activity improve, suggesting a synergistic therapeutic opportunity through combinatorial intervention.
This study demonstrates that PD-1/PD-L1 resistance in pancreatic cancer is not simply a target failure, but a consequence of immune suppression within the tumor microenvironment driven by PMN-MDSCs. By using matched human and murine organoid systems, the researchers revealed a consistent failure of checkpoint blockade across models, underscoring the translational relevance of their findings. This parallel breakdown highlights that traditional models often miss key immunosuppressive dynamics, and that physiologically relevant co-culture systems are essential to capturing the immune complexity of PDAC.
Considerations for Antibody Use in Organoid Models
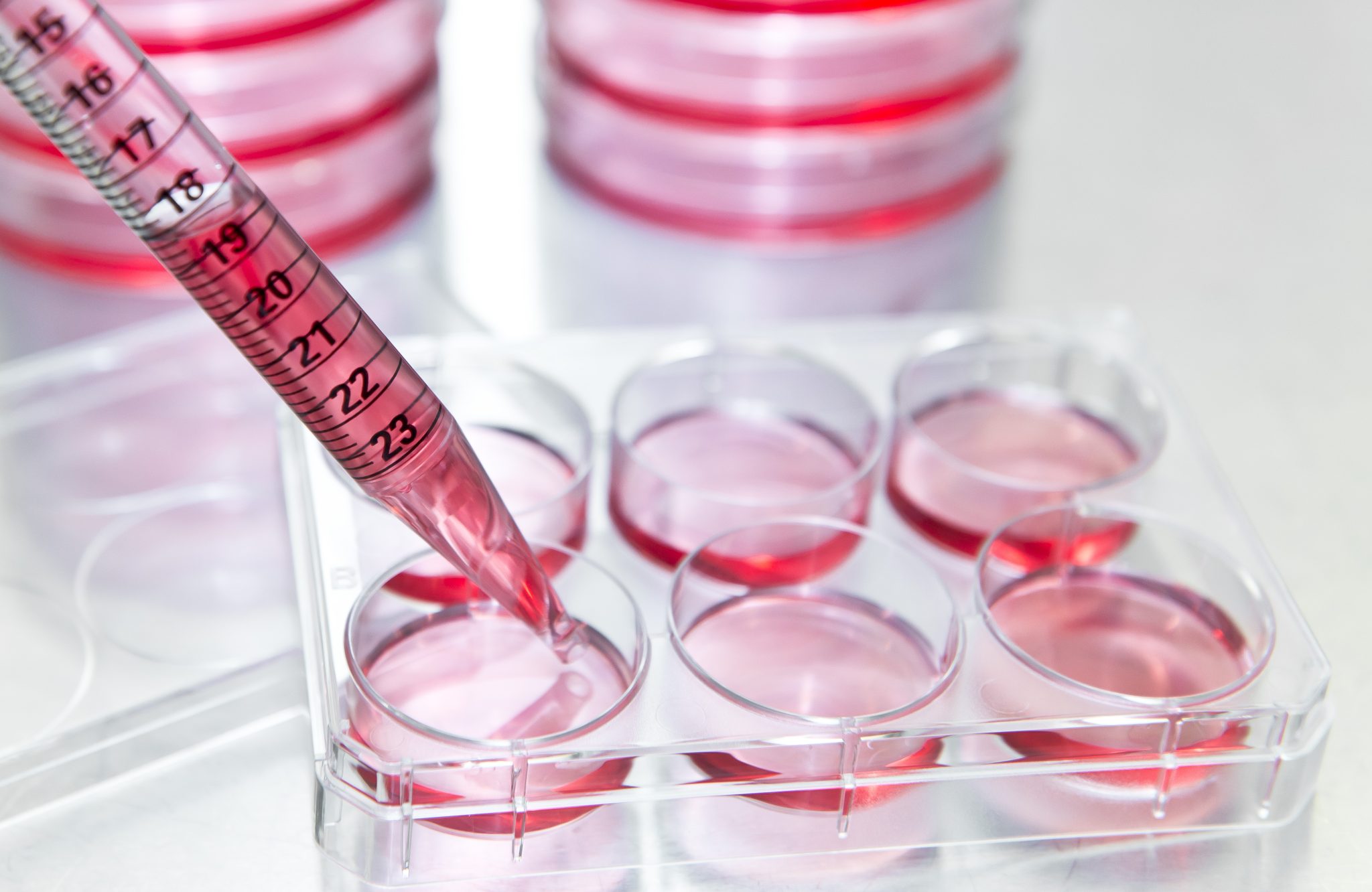
As researchers increasingly adopt organoid–immune co-cultures to simulate complex
in vivo biology, antibody quality becomes a critical factor in experimental success. For these studies to be both reproducible and translatable, antibodies should meet key criteria:
- Model Compatibility: Performance across models, both in vitro and in vivo applications
- Ultrapure Formulation: Low endotoxin levels and high specificity
- Additive-Free: No carrier proteins or preservatives that could alter cell behavior
- Trusted Documentation: Transparent QC and validation processes
Bio X Cell’s
InVivoPlus antibodies are engineered for consistency and performance in complex systems like organoid–immune co-cultures. With offerings that target both human and murine antigens, they enable translational studies that bridge preclinical and clinical insights. Each lot is rigorously tested for endotoxin levels, aggregation, and purity to ensure consistency and reliability across models in demanding applications including immune-oncology research.
Scientific and Translational Impact
This study from
Holokai et al. adds to a growing body of work using Bio X Cell antibodies to uncover the cellular and molecular crosstalk within the tumor microenvironment. From foundational studies by
Clark et al. and
Stromnes et al. to this organoid-based approach, these tools have enabled researchers to dissect immune evasion and identify more effective intervention points. As organoid models continue to evolve in complexity and relevance, having access to application-ready, reproducible antibodies like those from Bio X Cell becomes essential for advancing both mechanistic insight and translational impact.
 Pancreatic ductal adenocarcinoma (PDAC) is one of the most lethal cancers, driven in part by a uniquely immunosuppressive tumor microenvironment. Despite the presence of PD-L1 expression in nearly one-third of PDAC tumors, immune checkpoint therapies such as anti-PD-1 antibodies have shown limited clinical success. A study published in Cancers (Holokai et al. 2020) applied a stepwise mouse-to-human workflow that integrates orthotopic mouse models with matched mouse and patient-derived organoid–immune cell co-cultures. This parallel approach revealed that resistance to PD-1 blockade is conserved across species and is driven by suppressive myeloid biology rather than loss of PD-1/PD-L1 engagement, providing a translational framework for prioritizing immune-modulatory combinations before clinical testing.
Pancreatic ductal adenocarcinoma (PDAC) is one of the most lethal cancers, driven in part by a uniquely immunosuppressive tumor microenvironment. Despite the presence of PD-L1 expression in nearly one-third of PDAC tumors, immune checkpoint therapies such as anti-PD-1 antibodies have shown limited clinical success. A study published in Cancers (Holokai et al. 2020) applied a stepwise mouse-to-human workflow that integrates orthotopic mouse models with matched mouse and patient-derived organoid–immune cell co-cultures. This parallel approach revealed that resistance to PD-1 blockade is conserved across species and is driven by suppressive myeloid biology rather than loss of PD-1/PD-L1 engagement, providing a translational framework for prioritizing immune-modulatory combinations before clinical testing.