InVivoMAb anti-mouse/human/rat/monkey/hamster/canine/bovine TGF-β
Product Description
Specifications
| Isotype | Mouse IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb mouse IgG1 isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Bovine TGFβ isoform 2 |
| Reported Applications |
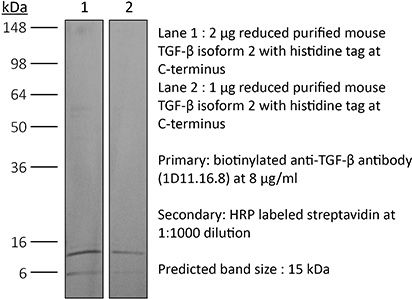
in vivo TGFβ neutralization in vitro TGFβ neutralization Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107757 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo TGFβ neutralization
Komai, T., et al (2018). "Transforming Growth Factor-beta and Interleukin-10 Synergistically Regulate Humoral Immunity via Modulating Metabolic Signals" Front Immunol 9: 1364.
PubMed
Inhibitory cytokines, such as transforming growth factor-beta (TGF-beta) and interleukin-10 (IL-10), are humoral factors involved in the suppressive function of regulatory T cells and play critical roles in maintaining immune homeostasis. However, TGF-beta and IL-10 also have pleiotropic effects and induce humoral immune responses depending on conditions, and thus their therapeutic application to autoimmune diseases remains limited. Here, we show that a combination of TGF-beta and IL-10, but not single cytokine, is required to suppress B cell activation induced by toll-like receptor (TLR) stimulation. In in vivo analyses, the simultaneous presence of TGF-beta and IL-10 effectively suppressed TLR-mediated antigen-specific immune responses and ameliorated pathologies in imiquimod (TLR7 agonist)-induced lupus model and lupus-prone MRL/lpr mice. Intriguingly, TGF-beta and IL-10 synergistically modulated transcriptional programs and suppressed cellular energetics of both glycolysis and oxidative phosphorylation via inhibition of the mammalian target of rapamycin complex 1 (mTORC1)/S6 kinase 1 (S6K1) pathway in TLR-stimulated B cells. On the other hand, enhancement of mTOR signaling and mitochondrial biosynthesis in TLR-stimulated B cells counteracted the synergistic inhibitory effects. The inhibitory cytokine synergy of TGF-beta and IL-10 via suppression of energy metabolism was also observed in human TLR-stimulated B cells. There is increasing evidence supporting the importance of adequate metabolic signals in various immune cells to exert their immune function. In this study, we have shown that a previously unrecognized synergy of inhibitory cytokines regulates systemic humoral immune responses via modulating immunometabolism in B cells. Our findings indicate that inhibition of B cell metabolism mediated by two synergistic cytokines contributes to the induction of immune tolerance and could be a new therapeutic strategy for autoimmune diseases such as systemic lupus erythematosus.
in vivo TGFβ neutralization
Clemente-Casares, X., et al (2016). "Expanding antigen-specific regulatory networks to treat autoimmunity" Nature 530(7591): 434-440.
PubMed
Regulatory T cells hold promise as targets for therapeutic intervention in autoimmunity, but approaches capable of expanding antigen-specific regulatory T cells in vivo are currently not available. Here we show that systemic delivery of nanoparticles coated with autoimmune-disease-relevant peptides bound to major histocompatibility complex class II (pMHCII) molecules triggers the generation and expansion of antigen-specific regulatory CD4(+) T cell type 1 (TR1)-like cells in different mouse models, including mice humanized with lymphocytes from patients, leading to resolution of established autoimmune phenomena. Ten pMHCII-based nanomedicines show similar biological effects, regardless of genetic background, prevalence of the cognate T-cell population or MHC restriction. These nanomedicines promote the differentiation of disease-primed autoreactive T cells into TR1-like cells, which in turn suppress autoantigen-loaded antigen-presenting cells and drive the differentiation of cognate B cells into disease-suppressing regulatory B cells, without compromising systemic immunity. pMHCII-based nanomedicines thus represent a new class of drugs, potentially useful for treating a broad spectrum of autoimmune conditions in a disease-specific manner.
in vitro TGFβ neutralization
Choi, Y. S., et al (2015). "LEF-1 and TCF-1 orchestrate TFH differentiation by regulating differentiation circuits upstream of the transcriptional repressor Bcl6" Nat Immunol 16(9): 980-990.
PubMed
Follicular helper T cells (TFH cells) are specialized effector CD4(+) T cells that help B cells develop germinal centers (GCs) and memory. However, the transcription factors that regulate the differentiation of TFH cells remain incompletely understood. Here we report that selective loss of Lef1 or Tcf7 (which encode the transcription factor LEF-1 or TCF-1, respectively) resulted in TFH cell defects, while deletion of both Lef1 and Tcf7 severely impaired the differentiation of TFH cells and the formation of GCs. Forced expression of LEF-1 enhanced TFH differentiation. LEF-1 and TCF-1 coordinated such differentiation by two general mechanisms. First, they established the responsiveness of naive CD4(+) T cells to TFH cell signals. Second, they promoted early TFH differentiation via the multipronged approach of sustaining expression of the cytokine receptors IL-6Ralpha and gp130, enhancing expression of the costimulatory receptor ICOS and promoting expression of the transcriptional repressor Bcl6.
in vitro TGFβ neutralization
Bodogai, M., et al (2015). "Immunosuppressive and Prometastatic Functions of Myeloid-Derived Suppressive Cells Rely upon Education from Tumor-Associated B Cells" Cancer Res 75(17): 3456-3465.
PubMed
Myeloid-derived suppressive cells (MDSC) have been reported to promote metastasis, but the loss of cancer-induced B cells/B regulatory cells (tBreg) can block metastasis despite MDSC expansion in cancer. Here, using multiple murine tumor models and human MDSC, we show that MDSC populations that expand in cancer have only partially primed regulatory function and limited prometastatic activity unless they are fully educated by tBregs. Cancer-induced tBregs directly activate the regulatory function of both the monocyte and granulocyte subpopulations of MDSC, relying, in part, on TgfbetaR1/TgfbetaR2 signaling. MDSC fully educated in this manner exhibit an increased production of reactive oxygen species and NO and more efficiently suppress CD4(+) and CD8(+) T cells, thereby promoting tumor growth and metastasis. Thus, loss of tBregs or TgfbetaR deficiency in MDSC is sufficient to disable their suppressive function and to block metastasis. Overall, our data indicate that cancer-induced B cells/B regulatory cells are important regulators of the immunosuppressive and prometastatic functions of MDSC.
in vivo TGFβ neutralization
Greco, S. H., et al (2015). "TGF-beta Blockade Reduces Mortality and Metabolic Changes in a Validated Murine Model of Pancreatic Cancer Cachexia" PLoS One 10(7): e0132786.
PubMed
Cancer cachexia is a debilitating condition characterized by a combination of anorexia, muscle wasting, weight loss, and malnutrition. This condition affects an overwhelming majority of patients with pancreatic cancer and is a primary cause of cancer-related death. However, few, if any, effective therapies exist for both treatment and prevention of this syndrome. In order to develop novel therapeutic strategies for pancreatic cancer cachexia, appropriate animal models are necessary. In this study, we developed and validated a syngeneic, metastatic, murine model of pancreatic cancer cachexia. Using our model, we investigated the ability of transforming growth factor beta (TGF-beta) blockade to mitigate the metabolic changes associated with cachexia. We found that TGF-beta inhibition using the anti-TGF-beta antibody 1D11.16.8 significantly improved overall mortality, weight loss, fat mass, lean body mass, bone mineral density, and skeletal muscle proteolysis in mice harboring advanced pancreatic cancer. Other immunotherapeutic strategies we employed were not effective. Collectively, we validated a simplified but useful model of pancreatic cancer cachexia to investigate immunologic treatment strategies. In addition, we showed that TGF-beta inhibition can decrease the metabolic changes associated with cancer cachexia and improve overall survival.
in vivo TGFβ neutralization
Manlove, L. S., et al (2015). "Adaptive Immunity to Leukemia Is Inhibited by Cross-Reactive Induced Regulatory T Cells" J Immunol .
PubMed
BCR-ABL+ acute lymphoblastic leukemia patients have transient responses to current therapies. However, the fusion of BCR to ABL generates a potential leukemia-specific Ag that could be a target for immunotherapy. We demonstrate that the immune system can limit BCR-ABL+ leukemia progression although ultimately this immune response fails. To address how BCR-ABL+ leukemia escapes immune surveillance, we developed a peptide: MHC class II tetramer that labels endogenous BCR-ABL-specific CD4+ T cells. Naive mice harbored a small population of BCR-ABL-specific T cells that proliferated modestly upon immunization. The small number of naive BCR-ABL-specific T cells was due to negative selection in the thymus, which depleted BCR-ABL-specific T cells. Consistent with this observation, we saw that BCR-ABL-specific T cells were cross-reactive with an endogenous peptide derived from ABL. Despite this cross-reactivity, the remaining population of BCR-ABL reactive T cells proliferated upon immunization with the BCR-ABL fusion peptide and adjuvant. In response to BCR-ABL+ leukemia, BCR-ABL-specific T cells proliferated and converted into regulatory T (Treg) cells, a process that was dependent on cross-reactivity with self-antigen, TGF-beta1, and MHC class II Ag presentation by leukemic cells. Treg cells were critical for leukemia progression in C57BL/6 mice, as transient Treg cell ablation led to extended survival of leukemic mice. Thus, BCR-ABL+ leukemia actively suppresses antileukemia immune responses by converting cross-reactive leukemia-specific T cells into Treg cells.
in vivo TGFβ neutralization
Leon, B., et al (2014). "FoxP3+ regulatory T cells promote influenza-specific Tfh responses by controlling IL-2 availability" Nat Commun 5: 3495.
PubMed
Here, we test the role of FoxP3(+) regulatory T cells (Tregs) in controlling T follicular helper (Tfh) and germinal centre (GC) B-cell responses to influenza. In contrast to the idea that Tregs suppress T-cell responses, we find that Treg depletion severely reduces the Tfh cell response to influenza virus. Furthermore, Treg depletion prevents the accumulation of influenza-specific GCs. These effects are not due to alterations in TGFbeta availability or a precursor-progeny relationship between Tregs and Tfh cells, but are instead mediated by increased availability of IL-2, which suppresses the differentiation of Tfh cells and as a consequence, compromises the GC B response. Thus, Tregs promote influenza-specific GC responses by preventing excessive IL-2 signalling, which suppresses Tfh cell differentiation.
in vivo TGFβ neutralization
Li, W., et al (2014). "Tgfbr2 disruption in postnatal smooth muscle impairs aortic wall homeostasis" J Clin Invest 124(2): 755-767.
PubMed
TGF-beta is essential for vascular development; however, excess TGF-beta signaling promotes thoracic aortic aneurysm and dissection in multiple disorders, including Marfan syndrome. Since the pathology of TGF-beta overactivity manifests primarily within the arterial media, it is widely assumed that suppression of TGF-beta signaling in vascular smooth muscle cells will ameliorate aortic disease. We tested this hypothesis by conditional inactivation of Tgfbr2, which encodes the TGF-beta type II receptor, in smooth muscle cells of postweanling mice. Surprisingly, the thoracic aorta rapidly thickened, dilated, and dissected in these animals. Tgfbr2 disruption predictably decreased canonical Smad signaling, but unexpectedly increased MAPK signaling. Type II receptor-independent effects of TGF-beta and pathological responses by nonrecombined smooth muscle cells were excluded by serologic neutralization. Aortic disease was caused by a perturbed contractile apparatus in medial cells and growth factor production by adventitial cells, both of which resulted in maladaptive paracrine interactions between the vessel wall compartments. Treatment with rapamycin restored a quiescent smooth muscle phenotype and prevented dissection. Tgfbr2 disruption in smooth muscle cells also accelerated aneurysm growth in a murine model of Marfan syndrome. Our data indicate that basal TGF-beta signaling in smooth muscle promotes postnatal aortic wall homeostasis and impedes disease progression.
in vivo TGFβ neutralization
Ring, S., et al (2013). "Targeting of autoantigens to DEC205(+) dendritic cells in vivo suppresses experimental allergic encephalomyelitis in mice" J Immunol 191(6): 2938-2947.
PubMed
The dendritic and epithelial cell receptor with a m.w. of 205 kDa (DEC205) is expressed by dendritic cells (DCs) and facilitates Ag presentation. After injection of Ags coupled to Abs specific for DEC205 into mice, Ag presentation occurs by nonactivated DCs, which leads to induction of regulatory T cells (Tregs). To test this system for tolerance induction in experimental allergic encephalomyelitis (EAE), we created single-chain fragment variables (scFv) specific for DEC205 and fused the scFv to the self-Ag myelin oligodendrocyte glycoprotein (MOG; scFv DEC:MOG). An anti-beta-galactosidase scFv:MOG fusion protein (scFv GL117:MOG) served as isotype control. After staining of DCs in vitro with purified scFv DEC:MOG, binding to DCs and colocalization with MHC class II was apparent, whereas isotype controls did not bind. We next injected scFv DEC:MOG into mice and observed elevated numbers of highly activated, IL-10-producing CD4(+)CD25(+)Foxp3(+) Tregs (17% of CD4) in spleens, as compared with isotype controls and uninjected mice (12% of CD4). Furthermore, DCs isolated from scFv DEC:MOG-injected animals produced significantly increased levels of TGF-beta. Most importantly, when EAE was induced in scFv DEC:MOG-injected mice, 90% of the mice were protected from EAE, whereas all mice in the isotype controls (scFv GL117:MOG) experienced development of EAE. When applying scFv DEC:MOG to mice that had already experienced EAE symptoms, abrogation of the disease in 90% of the animals was apparent, whereas all animals in the control groups experienced development of severe EAE. Thus, these data indicate that targeting of MOG to “steady-state” DCs in vivo may provide a tool to prevent and to treat EAE by a DC/Treg-driven mechanism.
in vitro TGFβ neutralization
Tai, N., et al (2013). "TLR9 deficiency promotes CD73 expression in T cells and diabetes protection in nonobese diabetic mice" J Immunol 191(6): 2926-2937.
PubMed
TLR9-deficient (TLR9(-)/(-)) NOD mice develop a significantly reduced incidence of diabetes. This study was to investigate the molecular mechanisms of the protective role of TLR9 deficiency. Through gene screening and confirmation by both mRNA and protein expression, we found a significant increase in CD73-expressing immune cells from peripheral lymphoid tissues in TLR9(-)/(-) NOD mice. The elevated frequency of CD73-expressing immune cells seemed to be specific for TLR9 deficiency and was MyD88 independent. Moreover, the increased frequency of CD73 expression was limited to the NOD background. Increased frequency of CD73 expression was also associated with lower levels of proinflammatory cytokines and more anti-inflammatory cytokine production in CD4(+) T cells in TLR9(-)/(-) NOD mice. Purified CD73(+)CD4(+) T cells showed stronger immunosuppressive function in vitro and delayed diabetes development in vivo. The immunosuppression appeared to be mediated by TGF-beta. In addition, elevated frequency of CD73-expressing cells was associated with improved beta cell function. Our observations were further confirmed by protection from diabetes with similar alterations in CD73 in the NY8.3 TCR NOD mouse model crossed with TLR9(-)/(-) mice and by the use of a TLR9 inhibitor in NOD mice. Our novel findings suggest an important immune-regulatory role of CD73 in regulation of diabetes development and may offer a new therapeutic strategy for specific intervention to prevent type 1 diabetes.
in vivo TGFβ neutralization
in vitro TGFβ neutralization
Worthington, J. J., et al (2013). "Loss of the TGFbeta-activating integrin alphavbeta8 on dendritic cells protects mice from chronic intestinal parasitic infection via control of type 2 immunity" PLoS Pathog 9(10): e1003675.
PubMed
Chronic intestinal parasite infection is a major global health problem, but mechanisms that promote chronicity are poorly understood. Here we describe a novel cellular and molecular pathway involved in the development of chronic intestinal parasite infection. We show that, early during development of chronic infection with the murine intestinal parasite Trichuris muris, TGFbeta signalling in CD4+ T-cells is induced and that antibody-mediated inhibition of TGFbeta function results in protection from infection. Mechanistically, we find that enhanced TGFbeta signalling in CD4+ T-cells during infection involves expression of the TGFbeta-activating integrin alphavbeta8 by dendritic cells (DCs), which we have previously shown is highly expressed by a subset of DCs in the intestine. Importantly, mice lacking integrin alphavbeta8 on DCs were completely resistant to chronic infection with T. muris, indicating an important functional role for integrin alphavbeta8-mediated TGFbeta activation in promoting chronic infection. Protection from infection was dependent on CD4+ T-cells, but appeared independent of Foxp3+ Tregs. Instead, mice lacking integrin alphavbeta8 expression on DCs displayed an early increase in production of the protective type 2 cytokine IL-13 by CD4+ T-cells, and inhibition of this increase by crossing mice to IL-4 knockout mice restored parasite infection. Our results therefore provide novel insights into how type 2 immunity is controlled in the intestine, and may help contribute to development of new therapies aimed at promoting expulsion of gut helminths.
in vivo TGFβ neutralization
Garidou, L., et al (2012). "Therapeutic blockade of transforming growth factor beta fails to promote clearance of a persistent viral infection" J Virol 86(13): 7060-7071.
PubMed
Persistent viral infections often overburden the immune system and are a major cause of disease in humans. During many persistent infections, antiviral T cells are maintained in a state of immune exhaustion characterized by diminished effector and helper functions. In mammalian systems, an extensive immune regulatory network exists to limit unwanted, potentially fatal immunopathology by inducing T cell exhaustion. However, this regulatory network at times overprotects the host and fosters viral persistence by severely dampening adaptive immune responsiveness. Importantly, recent studies have shown that T cell exhaustion is mediated in part by host immunoregulatory pathways (e.g., programmed death 1 [PD-1], interleukin 10 [IL-10]) and that therapeutic blockade of these pathways either before or during persistent infection can promote viral clearance. Transforming growth factor beta (TGF-beta) is another immunosuppressive cytokine known to impede both self- and tumor-specific T cells, but its role in regulating antiviral immunity is not entirely understood. In this study, we inhibited TGF-beta with three potent antagonists to determine whether neutralization of this regulatory molecule is a viable approach to control a persistent viral infection. Our results revealed that these inhibitors modestly elevate the number of antiviral T cells following infection with a persistent variant of lymphocytic choriomeningitis virus (LCMV) but have no impact on viral clearance. These data suggest that therapeutic neutralization of TGF-beta is not an efficacious means to promote clearance of a persistent viral infection.
in vivo TGFβ neutralization
Kurkjian, C., et al (2012). "Alveolar macrophages in neonatal mice are inherently unresponsive to Pneumocystis murina infection" Infect Immun 80(8): 2835-2846.
PubMed
Pneumocystis pneumonia was first diagnosed in malnourished children and has more recently been found in children with upper respiratory symptoms. We previously reported that there is a significant delay in the immune response in newborn mice infected with Pneumocystis compared to adults (Garvy BA, Harmsen AG, Infect. Immun. 64:3987-3992, 1996, and Garvy BA, Qureshi M, J. Immunol. 165:6480-6486, 2000). This delay is characterized by the failure of neonatal lungs to upregulate proinflammatory cytokines and attract T cells into the alveoli. Here, we report that regardless of the age at which we infected the mice, they failed to mount an inflammatory response in the alveolar spaces until they were 21 days of age or older. Anti-inflammatory cytokines had some role in dampening inflammation, since interleukin-10 (IL-10)-deficient pups cleared Pneumocystis faster than wild-type pups and the neutralization of transforming growth factor beta (TGF-beta) with specific antibody enhanced T cell migration into the lungs at later time points. However, the clearance kinetics were similar to those of control pups, suggesting that there is an intrinsic deficiency in the ability of innate immunity to control Pneumocystis. We found, using an adoptive transfer strategy, that the lung environment contributes to association of Pneumocystis organisms with alveolar macrophages, implying no intrinsic deficiency in the binding of Pneumocystis by neonatal macrophages. Using both in vivo and in vitro assays, we found that Pneumocystis organisms were less able to stimulate translocation of NF-kappaB to the nucleus of alveolar macrophages from neonatal mice. These data indicate that there is an early unresponsiveness of neonatal alveolar macrophages to Pneumocystis infection that is both intrinsic and related to the immunosuppressive environment found in neonatal lungs.
Product Citations
-
-
Immunology and Microbiology
-
COVID-19
IL-4 and TGF-β regulate inflammatory cytokines and cellular infiltration in the lung and systemic IL-6 in mouse-adapted SARS-CoV-2 infection.
In Immunohorizons on 25 August 2025 by Taye Sima, S., Puebla-Clark, L., et al.
PubMed
The pathology of severe COVID-19 is due to a hyperinflammatory immune response persisting after viral clearance. To understand how the immune response to SARS-CoV-2 is regulated to avoid severe COVID-19, we tested relevant immunoregulatory cytokines. Transforming growth factor β (TGF-β), interleukin (IL)-10, and IL-4 were neutralized upon infection with mouse-adapted SARS-CoV-2 (CMA3p20), a model of mild disease; lung inflammation was quantified by histology and flow cytometry at early and late time points. Mild weight loss and lung inflammation including consolidation and alveolar thickening were evident 3 d postinfection (dpi), and inflammation persisted to 7 dpi. Coinciding with early monocytic infiltrates, CCL2 and granulocyte colony-stimulating factor were transiently produced 3 dpi, while IL-12 and CCL5 persisted to 7 dpi, modeling viral and inflammatory phases of disease. Neutralization of TGF-β, but not IL-10 or IL-4, significantly increased lung inflammatory monocytes and elevated serum but not lung IL-6. Neutralization of IL-4 prolonged weight loss and increased early perivascular infiltration without changing viral titer. Anti-IL-4 reduced expression of Arg1, a gene associated with alternative activation of macrophages. Neutralizing TGF-β and IL-4 had differential effects on pathology after virus control. Lung perivascular infiltration was reduced 7 dpi by neutralization of IL-4 or TGF-β, and periairway inflammation was affected by anti-TGF-β, while alveolar infiltrates were not affected by either. Anti-IL-4 prolonged IL-12 to 7 dpi along with reduced IL-10 in lungs. Overall, the immunoregulatory cytokines TGF-β and IL-4 dampen initial inflammation in this mouse-adapted SARS-CoV-2 infection, suggesting that promotion of immunoregulation could help patients in early stages of disease.
-
-
-
Cancer Research
SMAD4 Deficiency Promotes Pancreatic Cancer Progression and Confers Susceptibility to TGFβ Inhibition.
In Cancer Res on 15 August 2025 by Murimwa, G. Z., Williams, N. E., et al.
PubMed
The 5-year overall survival rate for pancreatic cancer remains ∼13%, underscoring the urgent need for improved treatment strategies. TGFβ is a promising target due to its significant involvement in the desmoplasia, immune suppression, and chemoresistance characteristics of pancreatic cancer. More than 300 clinical trials targeting TGFβ have been conducted in unselected patient cohorts; however, none of the therapies have gained FDA approval. Nevertheless, TGFβ blockade may hold promise for a subset of cancers with nonfunctional TGFβ signaling. More than 25% of pancreatic cancers carry mutations in SMAD4, a key component of canonical TGFβ signaling. In this study, we investigated the potential for stratifying patients based on SMAD4 mutational status to identify tumors susceptible to TGFβ inhibition. Analysis of SMAD4 expression in human pancreatic tumors revealed that SMAD4 mutation or loss is associated with worse disease-free survival. Intriguingly, intratumoral SMAD4 expression displayed heterogeneity among human pancreatic cancer samples. SMAD4-deficient genetically engineered mouse models and orthotopic SMAD4 knockout tumor models exhibited reduced survival, increased metastasis, and alterations in the tumor microenvironment compared with SMAD4 wild-type controls, consistent with gene and protein expression changes in the absence of functional SMAD4. Importantly, treating mice bearing SMAD4-deficient tumors with a blocking TGFβ antibody reduced tumor weight and improved survival. These findings suggest that genomic stratification by TGFβ axis alterations, such as SMAD4 mutations, may be a promising approach to identifying patients likely to benefit from a TGFβ inhibitor.
-
-
Integrin-mediated mTOR signaling drives TGF-β overactivity and myxomatous mitral valve degeneration in hypomorphic fibrillin-1 mice.
In J Clin Invest on 15 July 2025 by Gao, F., Chen, Q., et al.
PubMed
Mitral valve prolapse is often benign, but progression to mitral regurgitation may require invasive intervention and there is no specific medical therapy. An association of mitral valve prolapse with Marfan syndrome resulting from pathogenic FBN1 variants supports the use of hypomorphic fibrillin-1 mgR mice to investigate mechanisms and therapy for mitral valve disease. mgR mice developed severe myxomatous mitral valve degeneration with mitral regurgitation by 12 weeks of age. Persistent activation of TGF-β and mTOR signaling along with macrophage recruitment preceded histological changes at 4 weeks of age. Short-term mTOR inhibition with rapamycin from 4 to 5 weeks of age prevented TGF-β overactivity and leukocytic infiltrates, while long-term inhibition of mTOR or TGF-β signaling from 4 to 12 weeks of age rescued mitral valve leaflet degeneration. Transcriptomic analysis identified integrins as key receptors in signaling interactions, and serologic neutralization of integrin signaling or a chimeric integrin receptor altering signaling prevented mTOR activation. We confirmed increased mTOR signaling and a conserved transcriptome signature in human specimens of sporadic mitral valve prolapse. Thus, mTOR activation from abnormal integrin-dependent cell-matrix interactions drives TGF-β overactivity and myxomatous mitral valve degeneration, and mTOR inhibition may prevent disease progression of mitral valve prolapse.
-
-
Immunology and Microbiology
Th1 differentiation and function are inhibited in neonates following human metapneumovirus infection.
In J Immunol on 1 July 2025 by Brown, E., Lan, J., et al.
PubMed
Human metapneumovirus (HMPV) is a leading cause of lower respiratory tract infection in children accounting for 7% of acute care visits and hospitalizations. In particular, neonates and infants have worse outcomes with HMPV infection. The neonatal immune system is regulated to favor anti-inflammatory and tolerogenic responses compared to adults, including prior work demonstrating epigenetic factors in neonatal CD4+ T cells promoting Th2 formation rather than antiviral Th1 differentiation. To interrogate the neonatal immune response to HMPV, 4-to-6 day-old mice or adult 6-to-8 week-old mice were infected with HMPV. Neonates had a decreased Th1 population and increased Th2 and regulatory T-cell (Treg) populations compared to adults. Neonatal Th1 function, but not cell number, was restrained by surface PD-1 expression. To assess if neonatal Th1 formation was intrinsically inhibited after HMPV, neonatal and adult CD4s were transferred into immunocompetent or immunodeficient neonates. Both adult and neonatal CD4s demonstrated reduced Th1 differentiation in the immunocompetent neonates, but robust Th1 differentiation in immunodeficient neonates and immunocompetent adults, suggesting an extrinsic mechanism. Loss of neonatal Tregs led to increased Th1 differentiation after HMPV infection. Neonatal Tregs had increased TGF-β production compared to adult Tregs, and disruption of TGF-β signaling increased Th1 induction. These data demonstrate Tregs provide extrinsic regulation of Th1 formation in the context of respiratory viral infections, rather than an intrinsic limitation of neonatal CD4s. Collectively, these findings identify a nuanced neonatal response to respiratory viruses limiting Th1 formation and function.
-
-
-
Immunology and Microbiology
Mucosal unadjuvanted booster vaccines elicit local IgA responses by conversion of pre-existing immunity in mice.
In Nat Immunol on 1 June 2025 by Kwon, D. I., Mao, T., et al.
PubMed
Mucosal delivery of vaccine boosters induces robust local protective immune responses even without any adjuvants. Yet, the mechanisms by which antigen alone induces mucosal immunity in the respiratory tract remain unclear. Here we show that an intranasal booster with an unadjuvanted recombinant SARS-CoV-2 spike protein, after intramuscular immunization with 1 μg of mRNA-LNP vaccine encoding the full-length SARS-CoV-2 spike protein (Pfizer/BioNTech BNT162b2), elicits protective mucosal immunity by retooling the lymph node-resident immune cells. On intranasal boosting, peripheral lymph node-primed B cells rapidly migrated to the lung through CXCR3-CXCL9 and CXCR3-CXCL10 signaling and differentiated into antigen-specific IgA-secreting plasma cells. Memory CD4+ T cells in the lung served as a natural adjuvant for developing mucosal IgA by inducing the expression of chemokines CXCL9 and CXCL10 for memory B cell recruitment. Furthermore, CD40 and TGFβ signaling had important roles in mucosal IgA development. Repeated mucosal boosting with an unadjuvanted protein amplified anamnestic IgA responses in both the upper and the lower respiratory tracts. These findings help explain why nasal boosters do not require an adjuvant to induce robust mucosal immunity at the respiratory mucosa and can be used to design safe and effective vaccines against respiratory pathogens.
-
-
TP53 mutations and TET2 deficiency cooperate to drive leukemogenesis and establish an immunosuppressive environment.
In J Clin Invest on 15 May 2025 by Zhang, P., Whipp, E. C., et al.
PubMed
Mutations and deletions in TP53 are associated with adverse outcomes in patients with myeloid malignancies, and there is an urgent need for the development of improved therapies for TP53-mutant leukemias. Here, we identified mutations in TET2 as the most common co-occurring mutation in patients with TP53-mutant acute myeloid leukemia (AML). In mice, combined hematopoietic-specific deletion of TET2 and TP53 resulted in enhanced self-renewal compared with deletion of either gene alone. Tp53/Tet2 double-KO mice developed serially transplantable AML. Both mice and patients with AML with combined TET2/TP53 alterations upregulated innate immune signaling in malignant granulocyte-monocyte progenitors, which had leukemia-initiating capacity. A20 governs the leukemic maintenance by triggering aberrant noncanonical NF-κB signaling. Mice with Tp53/Tet2 loss had expansion of monocytic myeloid-derived suppressor cells (MDSCs), which impaired T cell proliferation and activation. Moreover, mice and patients with AML with combined TP53/TET2 alterations displayed increased expression of the TIGIT ligand, CD155, on malignant cells. TIGIT-blocking antibodies augmented NK cell-mediated killing of Tp53/Tet2 double-mutant AML cells, reduced leukemic burden, and prolonged survival in Tp53/Tet2 double-KO mice. These findings describe a leukemia-promoting link between TET2 and TP53 mutations and highlight therapeutic strategies to overcome the immunosuppressive bone marrow environment in this adverse subtype of AML.
-
-
Cancer Research
-
Immunology and Microbiology
Single-cell sequencing unveils the transcriptomic landscape of castration-resistant prostate cancer-associated fibroblasts and their association with prognosis and immunotherapy response.
In BMC Cancer on 30 April 2025 by Qiu, Y., Wang, Y., et al.
PubMed
The tumor microenvironment (TME) is increasingly acknowledged as a determinant in the malignant transformation and progression of castration-resistant prostate cancer (CRPC). Cancer-associated fibroblasts (CAFs), as a pivotal stromal cellular component in TME, are implicated in tumor progression and immune escape. However, the molecular characteristics and biological functions of CRPC-CAFs in prostate cancer necessitate further investigation.
-
-
-
Immunohistochemistry
-
Immunohistochemistry
-
Cancer Research
-
Immunology and Microbiology
The Combination of Oncolytic Virus and Antibody Blockade of TGF-β Enhances the Efficacy of αvβ6-Targeting CAR T Cells Against Pancreatic Cancer in an Immunocompetent Model.
In Cancers (Basel) on 30 April 2025 by Zhao, Z., Cutmore, L. C., et al.
PubMed
CAR T cell therapy, as a rapidly advancing immuno-oncology modality, has achieved significant success in the treatment of leukaemia and lymphoma. However, its application in solid tumours remains limited. The challenges include the heterogeneity of tumours, local immunosuppression, poor trafficking and infiltration, life-threatening toxicity and the lack of precise representative immunocompetent research models. Considering its typically dense and immunosuppressive tumour microenvironment (TME) and early metastasis, pancreatic ductal adenocarcinoma (PDAC) was employed as a model to address the challenges that hinder CAR T cell therapies against solid tumours and to expand immunotherapeutic options for advanced disease.
-
-
Augmented expression of superoxide dismutase 2 mitigates progression and rupture of experimental abdominal aortic aneurysm.
In Theranostics on 11 April 2025 by Yan, H., Hu, Y., et al.
PubMed
Rationale: Oxidative stress is implicated in the pathogenesis and progression of abdominal aortic aneurysm (AAA). It is suggested that an excess in reactive oxygen species (ROS) over endogenous antioxidant activities can lead to endothelial and mitochondrial dysfunction, which promotes tissue inflammation, extracellular matrix degradation, and cellular apoptosis, all pathologic features characteristic of AAA. While elevated levels of ROS in human and experimental AAA appear well established, the contribution of endogenous antioxidant systems to aneurysm formation and progression remains controversial. We demonstrate that the antioxidant enzyme superoxide dismutase 2 (SOD2), the resident mitochondrial form of SODs that protects against mitochondrial damage, is relatively deficient in established preclinical AAA. We hypothesize that augmented expression of SOD2 will protect against oxidative stress and mitigate aneurysm progression. Methods: Herein, we employ a peptide-based nanoplatform to overexpress a key modulator of oxidative stress, SOD2. The efficacy of systemic delivery of murine SOD2 mRNA as an antioxidant nanotherapeutic agent was studied in two different murine AAA models. Unbiased mass spectrometry-enabled proteomics and high-dimensional bioinformatics were used to examine pathways modulated by SOD2 overexpression. Results: Using two different murine models of AAA, we show that in vivo augmentation of SOD2 expression via mRNA-based nanotherapy mitigates the expansion of small aneurysms and largely prevents rupture. Mitigation of AAA is accompanied by concomitant suppression of ROS, ROS surrogate markers, and apoptotic cell death. Proteomic profiling of AAA tissue and gene set enrichment analysis show that SOD2 overexpression is associated with modulation of oxidative phosphorylation, respiratory electron transport, and fatty acid metabolism. In addition, SOD2 overexpression inhibits platelet activation, downregulates mitogen-activated protein kinase signaling, and augments levels of microRNAs miR-181a-5p and miR17-5p targets that regulate vascular inflammation and cell apoptosis, respectively. Conclusions: These results confirm that SOD2 plays a pivotal role in the pathogenesis of experimental AAA and identify its potential as a therapeutic target.
-
-
Homo sapiens (Human)
Suppression of TGF-β/SMAD signaling by an inner nuclear membrane phosphatase complex.
In Nat Commun on 11 April 2025 by Ji, Z., Siu, W. S., et al.
PubMed
Cytokines of the TGF-β superfamily control essential cell fate decisions via receptor regulated SMAD (R-SMAD) transcription factors. Ligand-induced R-SMAD phosphorylation in the cytosol triggers their activation and nuclear accumulation. We determine how R-SMADs are inactivated by dephosphorylation in the cell nucleus to counteract signaling by TGF-β superfamily ligands. We show that R-SMAD dephosphorylation is mediated by an inner nuclear membrane associated complex containing the scaffold protein MAN1 and the CTDNEP1-NEP1R1 phosphatase. Structural prediction, domain mapping and mutagenesis reveals that MAN1 binds independently to the CTDNEP1-NEP1R1 phosphatase and R-SMADs to promote their inactivation by dephosphorylation. Disruption of this complex causes nuclear accumulation of R-SMADs and aberrant signaling, even in the absence of TGF-β ligands. These findings establish CTDNEP1-NEP1R1 as the R-SMAD phosphatase, reveal the mechanistic basis for TGF-β signaling inactivation and highlight how this process is disrupted by disease-associated MAN1 mutations.
-
-
-
Cancer Research
LTA4H improves the tumor microenvironment and prevents HCC progression via targeting the HNRNPA1/LTBP1/TGF-β axis.
In Cell Rep Med on 18 March 2025 by Yang, S., Qiu, X., et al.
PubMed
Leukotriene A4 hydrolase (LTA4H), an inflammatory mediator, has garnered attention for its role in the development of chronic lung diseases and various cancers. Our study highlights the protective role of LTA4H in hepatocellular carcinoma (HCC) occurrence and progression. LTA4H is downregulated in clinical and mouse HCC tumors. LTA4H deficiency exacerbates hepatocyte damage by restraining JNK activation and promotes CD206+ macrophage polarization through the upregulation of LTBP1 expression and downstream transforming growth factor β (TGF-β) secretion and activation. Mechanistically, LTA4H induces heterogeneous nuclear ribonucleoprotein A1 (HNRNPA1) phosphorylation, enhancing their interaction and leading to the functional inhibition of HNRNPA1 in regulating Ltbp1 mRNA maturation and processing in the nucleus. LTA4H-deficient patients exhibit poor prognosis and immunotherapy resistance. Combination therapy targeting TGF-β and PD-1 significantly improves the immunotherapy resistance of LTA4H-knockout Hepa1-6 tumors. Our findings reveal the previously unreported role of LTA4H in regulating the tumor microenvironment and provide insights into potential diagnostic and therapeutic strategies for patients with LTA4H-deficient HCC.
-
-
Single-cell and chromatin accessibility profiling reveals regulatory programs of pathogenic Th2 cells in allergic asthma.
In Nat Commun on 15 March 2025 by Khan, M., Alteneder, M., et al.
PubMed
Lung pathogenic T helper type 2 (pTh2) cells are important in mediating allergic asthma, but fundamental questions remain regarding their heterogeneity and epigenetic regulation. Here we investigate immune regulation in allergic asthma by single-cell RNA sequencing in mice challenged with house dust mite, in the presence and absence of histone deacetylase 1 (HDAC1) function. Our analyses indicate two distinct highly proinflammatory subsets of lung pTh2 cells and pinpoint thymic stromal lymphopoietin (TSLP) and Tumour Necrosis Factor Receptor Superfamily (TNFRSF) members as important drivers to generate pTh2 cells in vitro. Using our in vitro model, we uncover how signalling via TSLP and a TNFRSF member shapes chromatin accessibility at the type 2 cytokine gene loci by modulating HDAC1 repressive function. In summary, we have generated insights into pTh2 cell biology and establish an in vitro model for investigating pTh2 cells that proves useful for discovering molecular mechanisms involved in pTh2-mediated allergic asthma.
-
-
Immunology and Microbiology
-
Neuroscience
STING Deficiency Promotes Th17-Like Tfh to Aggravate the Experimental Autoimmune Uveitis.
In Invest Ophthalmol Vis Sci on 3 March 2025 by Li, Z., Liu, X., et al.
PubMed
The purpose of this study was to explore the underlying mechanism that Th17-like T follicular helper cells (Tfh) orchestrated by STING signaling have a pathogenic role in experimental autoimmune uveitis (EAU).
-
-
-
Immunology and Microbiology
TBX3 shapes an immunosuppressive microenvironment and induces immunotherapy resistance.
In Theranostics on 3 February 2025 by Liu, Z., Zhang, C., et al.
PubMed
Background: Identifying biomarkers that predict immunotherapy efficacy and discovering new targets for combination therapies are critical elements for improving the prognosis of bladder cancer (BLCA) patients. Methods: Firstly, we explored the expression patterns of TBX3 in normal and pan-cancer tissues and the correlation between TBX3 and the immune microenvironment using data from multiple public databases. Then, we combined various techniques, including bulk RNA sequencing, single-cell RNA sequencing, high-throughput cytokine arrays, functional experiments, ProcartaPlex multiplex immunoassays and TissueFAXS panoramic tissue quantification assays, to demonstrate that TBX3 shapes an immunosuppressive tumor microenvironment (TME) in BLCA. Results: We identified TBX3 as a key factor associated with the immunosuppressive microenvironment in BLCA through a systematic multi-omics analysis. We found that TBX3 is primarily expressed in malignant cells, where TBX3high tumor cells increase the secretion of TGFβ1, which promotes the infiltration of cancer-associated fibroblasts (CAFs), thereby forming an immunosuppressive microenvironment. We further demonstrated that TBX3 enhances TGFβ1 expression by binding to the TGFβ1 promoter, and blocking TGFβ1 counteracts the immunosuppressive effects of TBX3. Moreover, TBX3 reduced the cancer-killing efficiency of CD8+ T cells by decreasing the proportion of GZMB+ CD8+ T cells, and knocking down TBX3 combined with anti-PD-1 treatment increased CD8+ T cell infiltration and reduced CAFs in vivo. We also validated the inverse relationship between TBX3+ malignant cells and CD8+ T cells and the positive relationship with CAFs in tissue microarrays. Lastly, we found that TBX3 predicted immunotherapy efficacy in our real-world immunotherapy cohort and multiple public cohorts. Conclusion: In summary, TBX3 promotes BLCA progression and immunotherapy resistance by inducing an immunosuppressive microenvironment, and targeting TBX3 could enhance the efficacy of immunotherapy for BLCA.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
Aberrant cytoplasmic expression of UHRF1 restrains the MHC-I-mediated anti-tumor immune response.
In Nat Commun on 3 October 2024 by Tan, L. M., Yin, T., et al.
PubMed
Immunotherapy successfully complements traditional cancer treatment. However, primary and acquired resistance might limit efficacy. Reduced antigen presentation by MHC-I has been identified as potential resistance factor. Here we show that the epigenetic regulator ubiquitin-like with PHD and ring finger domains 1 (UHRF1), exhibits altered expression and aberrant cytosolic localization in cancerous tissues, where it promotes MHC-I ubiquitination and degradation. Cytoplasmic translocation of UHRF1 is induced by its phosphorylation on a specific serine in response to signals provided by factors present in the tumor microenvironment (TME), such as TGF-β, enabling UHRF1 to bind MHC-I. Downregulation of MHC-I results in suppression of the antigen presentation pathway to establish an immune hostile TME. UHRF1 inactivation by genetic deletion synergizes with immune checkpoint blockade (ICB) treatment and induces an anti-tumour memory response by evoking low-affinity T cells. Our study adds to the understanding of UHRF1 in cancer immune evasion and provides a potential target to synergize with immunotherapy and overcome immunotherapeutic resistance.
-
-
Suppression of TGF-β/SMAD signaling by an inner nuclear membrane phosphatase complex
In bioRxiv on 23 September 2024 by Ji, Z., Siu, W. S., et al.
-
Adrenal gland macrophages regulate glucocorticoid production through Trem2 and TGF-β.
In JCI Insight on 13 June 2024 by Xu, Y., Patterson, M. T., et al.
PubMed
Glucocorticoid synthesis by adrenal glands (AGs) is regulated by the hypothalamic-pituitary-adrenal axis to facilitate stress responses when the host is exposed to stimuli. Recent studies implicate macrophages as potential steroidogenic regulators, but the molecular mechanisms by which AG macrophages exert such influence remain unclear. In this study, we investigated the role of AG macrophages in response to cold challenge or atherosclerotic inflammation as physiologic models of acute or chronic stress. Using single-cell RNA sequencing, we observed dynamic AG macrophage polarization toward classical activation and lipid-associated phenotypes following acute or chronic stimulation. Among transcriptional alterations induced in macrophages, triggering receptor expressed on myeloid cells 2 (Trem2) was highlighted because of its upregulation following stress. Conditional deletion of macrophage Trem2 revealed a protective role in stress responses. Mechanistically, Trem2 deletion led to increased AG macrophage death, abolished the TGF-β-producing capacity of AG macrophages, and resulted in enhanced glucocorticoid production. In addition, enhanced glucocorticoid production was replicated by blockade of TGF-β signaling. Together, these observations suggest that AG macrophages restrict steroidogenesis through Trem2 and TGF-β, which opens potential avenues for immunotherapeutic interventions to resolve stress-related disorders.
-
-
Cancer Research
-
Immunology and Microbiology
Chemoradiotherapy-induced ACKR2+ tumor cells drive CD8+ T cell senescence and cervical cancer recurrence.
In Cell Rep Med on 21 May 2024 by Dai, D., Pei, Y., et al.
PubMed
Tumor recurrence after chemoradiotherapy is challenging to overcome, and approaches to predict the recurrence remain elusive. Here, human cervical cancer tissues before and after concurrent chemoradiotherapy (CCRT) analyzed by single-cell RNA sequencing reveal that CCRT specifically promotes CD8+ T cell senescence, driven by atypical chemokine receptor 2 (ACKR2)+ CCRT-resistant tumor cells. Mechanistically, ACKR2 expression is increased in response to CCRT and is also upregulated through the ligation of CC chemokines that are produced by activated myeloid and T cells. Subsequently, ACKR2+ tumor cells are induced to produce transforming growth factor β to drive CD8+ T cell senescence, thereby compromising antitumor immunity. Moreover, retrospective analysis reveals that ACKR2 expression and CD8+ T cell senescence are enhanced in patients with cervical cancer who experienced recurrence after CCRT, indicating poor prognosis. Overall, we identify a subpopulation of CCRT-resistant ACKR2+ tumor cells driving CD8+ T cell senescence and tumor recurrence and highlight the prognostic value of ACKR2 and CD8+ T cell senescence for chemoradiotherapy recurrence.
-
-
-
Immunology and Microbiology
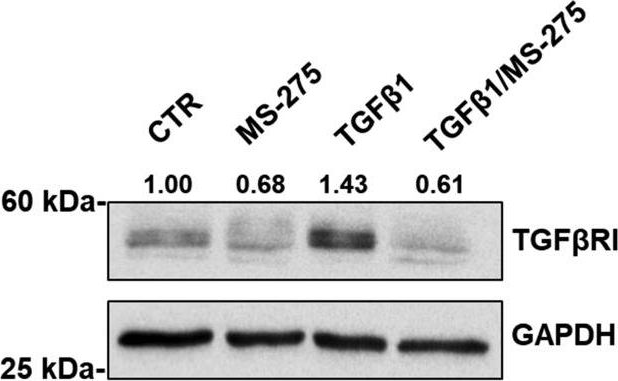
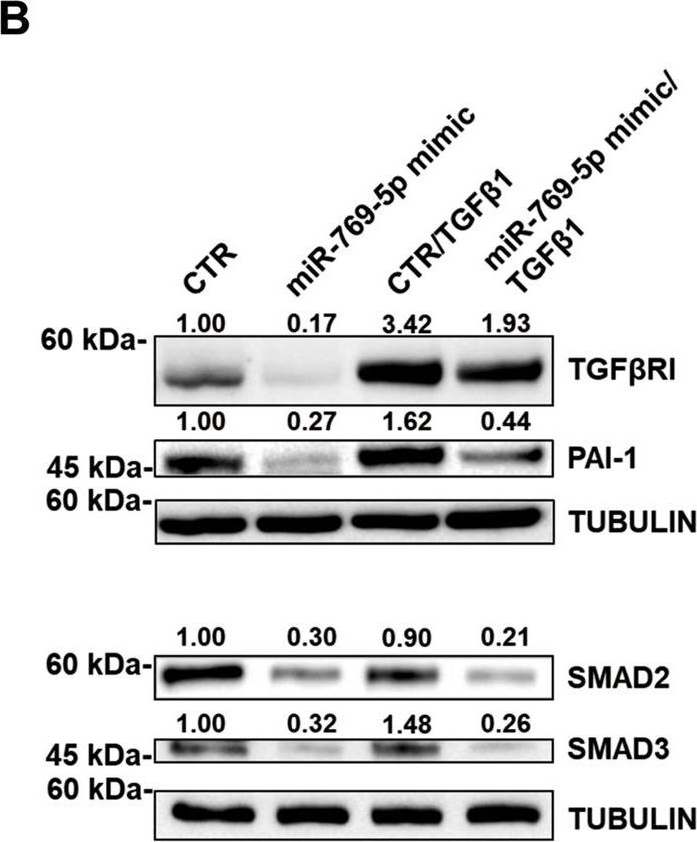
TGF-β1 induces PD-1 expression in macrophages through SMAD3/STAT3 cooperative signaling in chronic inflammation.
In JCI Insight on 5 March 2024 by Lei, Z., Tang, R., et al.
PubMed
Programmed cell death protein 1 (PD-1), a coinhibitory T cell checkpoint, is also expressed on macrophages in pathogen- or tumor-driven chronic inflammation. Increasing evidence underscores the importance of PD-1 on macrophages for dampening immune responses. However, the mechanism governing PD-1 expression in macrophages in chronic inflammation remains largely unknown. TGF-β1 is abundant within chronic inflammatory microenvironments. Here, based on public databases, significantly positive correlations between PDCD1 and TGFB1 gene expression were observed in most human tumors. Of note, among immune infiltrates, macrophages as the predominant infiltrate expressed higher PDCD1 and TGFBR1/TGFBR2 genes. MC38 colon cancer and Schistosoma japonicum infection were used as experimental models for chronic inflammation. PD-1hi macrophages from chronic inflammatory tissues displayed an immunoregulatory pattern and expressed a higher level of TGF-β receptors. Either TGF-β1-neutralizing antibody administration or macrophage-specific Tgfbr1 knockdown largely reduced PD-1 expression on macrophages in animal models. We further demonstrated that TGF-β1 directly induced PD-1 expression on macrophages. Mechanistically, TGF-β1-induced PD-1 expression on macrophages was dependent on SMAD3 and STAT3, which formed a complex at the Pdcd1 promoter. Collectively, our study shows that macrophages adapt to chronic inflammation through TGF-β1-triggered cooperative SMAD3/STAT3 signaling that induces PD-1 expression and modulates macrophage function.
-
-
-
Cancer Research
UPP1 promotes lung adenocarcinoma progression through the induction of an immunosuppressive microenvironment.
In Nat Commun on 8 February 2024 by Li, Y., Jiang, M., et al.
PubMed
The complexity of the tumor microenvironment (TME) is a crucial factor in lung adenocarcinoma (LUAD) progression. To gain deeper insights into molecular mechanisms of LUAD, we perform an integrative single-cell RNA sequencing (scRNA-seq) data analysis of 377,574 cells from 117 LUAD patient samples. By linking scRNA-seq data with bulk gene expression data, we identify a cluster of prognostic-related UPP1high tumor cells. These cells, primarily situated at the invasive front of tumors, display a stronger association with the immunosuppressive components in the TME. Our cytokine array analysis reveals that the upregulation of UPP1 in tumor cells leads to the increased release of various immunosuppressive cytokines, with TGF-β1 being particularly prominent. Furthermore, this UPP1 upregulation also elevates the expression of PD-L1 through the PI3K/AKT/mTOR pathway, which contributes to the suppression of CD8 + T cells. Cytometry by time-of-flight (CyTOF) analysis provides additional evidence of the role of UPP1 in shaping the immunosuppressive nature of the TME. Using patient-derived organoids (PDOs), we discover that UPP1high tumors exhibit relatively increased sensitivity to Bosutinib and Dasatinib. Collectively, our study highlights the immunosuppressive role of UPP1 in LUAD, and these findings may provide insights into the molecular features of LUAD and facilitate the development of personalized treatment strategies.
-