InVivoMAb anti-mouse PD-L1 (B7-H1)
Product Details
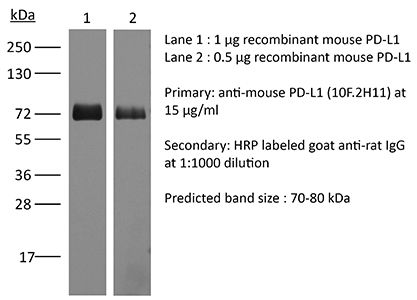
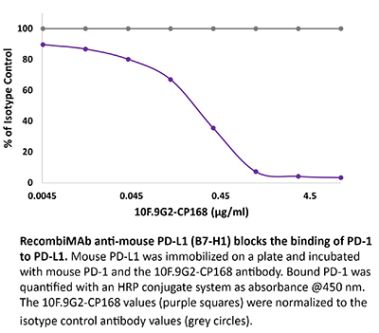
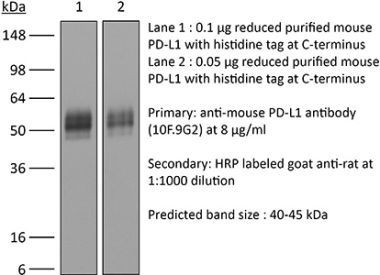
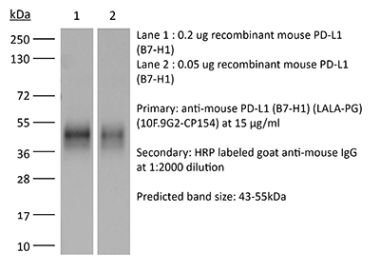
The 10F.2H11 monoclonal antibody reacts with mouse PD-L1 (programmed death ligand 1) also known as B7-H1 or CD274. PD-L1 is a 40 kDa type I transmembrane protein that belongs to the B7 family of the Ig superfamily. PD-L1 is expressed on T lymphocytes, B lymphocytes, NK cells, dendritic cells, as well as IFNγ stimulated monocytes, epithelial cells and endothelial cells. PD-L1 binds to its receptor, PD-1, found on CD4 and CD8 thymocytes as well as activated T and B lymphocytes and myeloid cells. Engagement of PD-L1 with PD-1 leads to inhibition of TCR-mediated T cell proliferation and cytokine production. PD-L1 is thought to play an important role in tumor immune evasion. Induced PD-L1 expression is common in many tumors and results in increased resistance of tumor cells to CD8 T cell mediated lysis. The 10F.2H11 antibody has been shown to sterically and functionally block PD-L1/CD80 (B7-1) interactions and does not block PD-L1/PD-1 interactions.Specifications
| Isotype | Rat IgG2b, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2b isotype control, anti-keyhole limpet hemocyanin |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Murine PD-L1 expressing CHO cells |
| Reported Applications |
in vivo blocking of PD-L1/CD80 (B7-1) interactions in vitro blocking of PD-L1/CD80 (B7-1) interactions ELISA Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Purification | Protein G |
| RRID | AB_2927503 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
in vitro blocking of PD-L1/CD80 (B7-1) interactions
Mott, K. R., et al. (2014). "Inclusion of CD80 in HSV targets the recombinant virus to PD-L1 on DCs and allows productive infection and robust immune responses" PLoS One 9(1): e87617. PubMed
CD80 plays a critical role in stimulation of T cells and subsequent control of infection. To investigate the effect of CD80 on HSV-1 infection, we constructed a recombinant HSV-1 virus that expresses two copies of the CD80 gene in place of the latency associated transcript (LAT). This mutant virus (HSV-CD80) expressed high levels of CD80 and had similar virus replication kinetics as control viruses in rabbit skin cells. In contrast to parental virus, this CD80 expressing recombinant virus replicated efficiently in immature dendritic cells (DCs). Additionally, the susceptibility of immature DCs to HSV-CD80 infection was mediated by CD80 binding to PD-L1 on DCs. This interaction also contributed to a significant increase in T cell activation. Taken together, these results suggest that inclusion of CD80 as a vaccine adjuvant may promote increased vaccine efficacy by enhancing the immune response directly and also indirectly by targeting to DC.
in vivo blocking of PD-L1/CD80 (B7-1) interactions
Yang, J., et al. (2011). "The novel costimulatory programmed death ligand 1/B7.1 pathway is functional in inhibiting alloimmune responses in vivo" J Immunol 187(3): 1113-1119. PubMed
The programmed death ligand 1 (PDL1)/programmed death 1 (PD1) costimulatory pathway plays an important role in the inhibition of alloimmune responses as well as in the induction and maintenance of peripheral tolerance. It has been demonstrated recently that PDL1 also can bind B7.1 to inhibit T cell responses in vitro. Using the bm12 into B6 heart transplant model, we investigated the functional significance of this interaction in alloimmune responses in vivo. PD1 blockade unlike PDL1 blockade failed to accelerate bm12 allograft rejection, suggesting a role for an additional binding partner for PDL1 other than PD1 in transplant rejection. PDL1 blockade was able to accelerate allograft rejection in B7.2-deficient recipients but not B7.1-deficient recipients, indicating that PDL1 interaction with B7.1 was important in inhibiting rejection. Administration of the novel 2H11 anti-PDL1 mAb, which only blocks the PDL1-B7.1 interaction, aggravated chronic injury of bm12 allografts in B6 recipients. Aggravated chronic injury was associated with an increased frequency of alloreactive IFN-gamma-, IL-4-, and IL-6-producing splenocytes and a decreased percentage of regulatory T cells in the recipients. Using an in vitro cell culture assay, blockade of the interaction of PDL1 on dendritic cells with B7.1 on T cells increased IFN-gamma production from alloreactive CD4(+) T cells, whereas blockade of dendritic cell B7.1 interaction with T cell PDL1 did not. These data indicate that PDL1 interaction with B7.1 plays an important role in the inhibition of alloimmune responses in vivo and suggests a dominant direction for PDL1 and B7.1 interaction.
in vivo blocking of PD-L1/CD80 (B7-1) interactions, in vitro blocking of PD-L1/CD80 (B7-1) interactions, ELISA, Flow Cytometry
Paterson, A. M., et al. (2011). "The programmed death-1 ligand 1:B7-1 pathway restrains diabetogenic effector T cells in vivo" J Immunol 187(3): 1097-1105. PubMed
Programmed death-1 ligand 1 (PD-L1) is a coinhibitory molecule that negatively regulates multiple tolerance checkpoints. In the NOD mouse model, PD-L1 regulates the development of diabetes. PD-L1 has two binding partners, programmed death-1 and B7-1, but the significance of the PD-L1:B7-1 interaction in regulating self-reactive T cell responses is not yet clear. To investigate this issue in NOD mice, we have compared the effects of two anti-PD-L1 Abs that have different blocking activities. Anti-PD-L1 mAb 10F.2H11 sterically and functionally blocks only PD-L1:B7-1 interactions, whereas anti-PD-L1 mAb 10F.9G2 blocks both PD-L1:B7-1 and PD-L1:programmed death-1 interactions. Both Abs had potent, yet distinct effects in accelerating diabetes in NOD mice: the single-blocker 10F.2H11 mAb was more effective at precipitating diabetes in older (13-wk-old) than in younger (6- to 7-wk-old) mice, whereas the dual-blocker 10F.9G2 mAb rapidly induced diabetes in NOD mice of both ages. Similarly, 10F.2H11 accelerated diabetes in recipients of T cells from diabetic, but not prediabetic mice, whereas 10F.9G2 was effective in both settings. Both anti-PD-L1 mAbs precipitated diabetes in adoptive transfer models of CD4(+) and CD8(+) T cell-driven diabetes. Taken together, these data demonstrate that the PD-L1:B7-1 pathway inhibits potentially pathogenic self-reactive effector CD4(+) and CD8(+) T cell responses in vivo, and suggest that the immunoinhibitory functions of this pathway may be particularly important during the later phases of diabetogenesis.
- Cancer Research,
- Genetics
Cancer cell genetics shaping of the tumor microenvironment reveals myeloid cell-centric exploitable vulnerabilities in hepatocellular carcinoma.
In Nature Communications on 22 March 2024 by Ramirez, C. F. A., Taranto, D., et al.
PubMed
Myeloid cells are abundant and plastic immune cell subsets in the liver, to which pro-tumorigenic, inflammatory and immunosuppressive roles have been assigned in the course of tumorigenesis. Yet several aspects underlying their dynamic alterations in hepatocellular carcinoma (HCC) progression remain elusive, including the impact of distinct genetic mutations in shaping a cancer-permissive tumor microenvironment (TME). Here, in newly generated, clinically-relevant somatic female HCC mouse models, we identify cancer genetics' specific and stage-dependent alterations of the liver TME associated with distinct histopathological and malignant HCC features. Mitogen-activated protein kinase (MAPK)-activated, NrasG12D-driven tumors exhibit a mixed phenotype of prominent inflammation and immunosuppression in a T cell-excluded TME. Mechanistically, we report a NrasG12D cancer cell-driven, MEK-ERK1/2-SP1-dependent GM-CSF secretion enabling the accumulation of immunosuppressive and proinflammatory monocyte-derived Ly6Clow cells. GM-CSF blockade curbs the accumulation of these cells, reduces inflammation, induces cancer cell death and prolongs animal survival. Furthermore, GM-CSF neutralization synergizes with a vascular endothelial growth factor (VEGF) inhibitor to restrain HCC outgrowth. These findings underscore the profound alterations of the myeloid TME consequential to MAPK pathway activation intensity and the potential of GM-CSF inhibition as a myeloid-centric therapy tailored to subsets of HCC patients. © 2024. The Author(s).
- Cancer Research,
- Immunology and Microbiology
Converting bacteria into autologous tumor vaccine via surface biomineralization of calcium carbonate for enhanced immunotherapy.
In Acta Pharmaceutica Sinica. B on 1 December 2023 by Guo, L., Ding, J., et al.
PubMed
Autologous cancer vaccine that stimulates tumor-specific immune responses for personalized immunotherapy holds great potential for tumor therapy. However, its efficacy is still suboptimal due to the immunosuppressive tumor microenvironment (ITM). Here, we report a new type of bacteria-based autologous cancer vaccine by employing calcium carbonate (CaCO3) biomineralized Salmonella (Sal) as an in-situ cancer vaccine producer and systematical ITM regulator. CaCO3 can be facilely coated on the Sal surface with calcium ionophore A23187 co-loading, and such biomineralization did not affect the bioactivities of the bacteria. Upon intratumoral accumulation, the CaCO3 shell was decomposed at an acidic microenvironment to attenuate tumor acidity, accompanied by the release of Sal and Ca2+/A23187. Specifically, Sal served as a cancer vaccine producer by inducing cancer cells' immunogenic cell death (ICD) and promoting the gap junction formation between tumor cells and dendritic cells (DCs) to promote antigen presentation. Ca2+, on the other hand, was internalized into various types of immune cells with the aid of A23187 and synergized with Sal to systematically regulate the immune system, including DCs maturation, macrophages polarization, and T cells activation. As a result, such bio-vaccine achieved remarkable efficacy against both primary and metastatic tumors by eliciting potent anti-tumor immunity with full biocompatibility. This work demonstrated the potential of bioengineered bacteria as bio-active vaccines for enhanced tumor immunotherapy. © 2023 Chinese Pharmaceutical Association and Institute of Materia Medica, Chinese Academy of Medical Sciences. Production and hosting by Elsevier B.V.
- Cancer Research,
- Genetics
Cancer cell genetics shaping of the tumor microenvironment reveals myeloid cell-centric exploitable vulnerabilities in hepatocellular carcinoma
Preprint on BioRxiv : the Preprint Server for Biology on 1 November 2023 by Ramirez, C. F., Taranto, D., et al.
PubMed
Myeloid cells are abundant and plastic immune cell subsets in the liver, to which pro-tumorigenic, inflammatory and immunosuppressive roles have been assigned in the course of tumorigenesis. Yet several aspects underlying their dynamic alterations in hepatocellular carcinoma (HCC) progression remain elusive, including the impact of distinct genetic mutations in shaping a cancer-permissive tumor microenvironment (TME). Here, we generated somatic HCC mouse models bearing clinically-relevant oncogenic driver combinations and subsequent pathway activation that faithfully recapitulated different human HCC subclasses. We identified cancer genetics’ specific and stage-dependent alterations of the liver TME associated with distinct histopathological and malignant HCC features. These models ranged from T cell-rich, more indolent HCC to aggressive tumors exhibiting heightened myeloid cell infiltration. Interestingly, MAPK-activated, Nras G12D -driven tumors presented a mixed phenotype of prominent inflammation and immunosuppression in a T cell-excluded TME, contrasting with Nras G12V HCC, enriched in adaptive immune cells. Mechanistically, we identified a Nras G12D cancer cell-driven, MEK-ERK1/2-SP1-dependent GM-CSF secretion enabling the accumulation of immunosuppressive and proinflammatory monocyte-derived Ly6C low cells. GM-CSF blockade curbed the accumulation of this myeloid cell subset, reduced inflammation, induced cancer cell death and prolonged animal survival. Furthermore, the anti-tumor effect of GM-CSF neutralization synergized with the clinically-approved inhibition of the vascular endothelial growth factor (VEGF) to inhibit HCC outgrowth. These findings underscore the striking alterations of the myeloid TME consequential to MAPK pathway activation intensity and the potential of GM-CSF inhibition as a myeloid-centric therapy tailored to subsets of HCC patients.
- Cancer Research
IL-2 is inactivated by the acidic pH environment of tumors enabling engineering of a pH-selective mutein.
In Science Immunology on 9 December 2022 by Gaggero, S., Martinez-Fabregas, J., et al.
PubMed
Cytokines interact with their receptors in the extracellular space to control immune responses. How the physicochemical properties of the extracellular space influence cytokine signaling is incompletely elucidated. Here, we show that the activity of interleukin-2 (IL-2), a cytokine critical to T cell immunity, is profoundly affected by pH, limiting IL-2 signaling within the acidic environment of tumors. Generation of lactic acid by tumors limits STAT5 activation, effector differentiation, and antitumor immunity by CD8+ T cells and renders high-dose IL-2 therapy poorly effective. Directed evolution enabled selection of a pH-selective IL-2 mutein (Switch-2). Switch-2 binds the IL-2 receptor subunit IL-2Rα with higher affinity, triggers STAT5 activation, and drives CD8+ T cell effector function more potently at acidic pH than at neutral pH. Consequently, high-dose Switch-2 therapy induces potent immune activation and tumor rejection with reduced on-target toxicity in normal tissues. Last, we show that sensitivity to pH is a generalizable property of a diverse range of cytokines with broad relevance to immunity and immunotherapy in healthy and diseased tissues.
- In Vivo,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
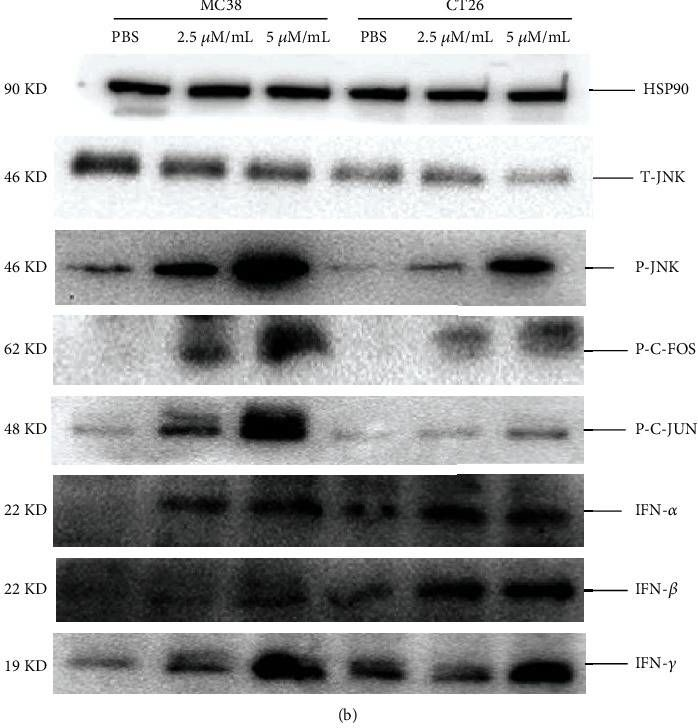
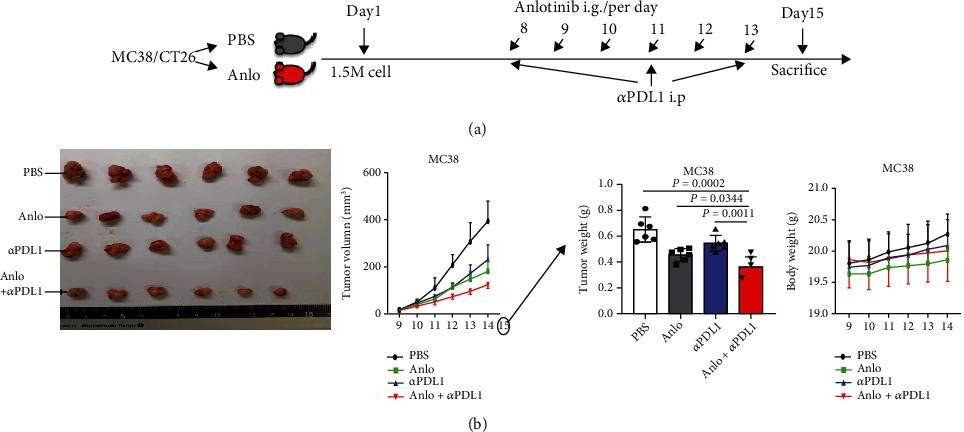
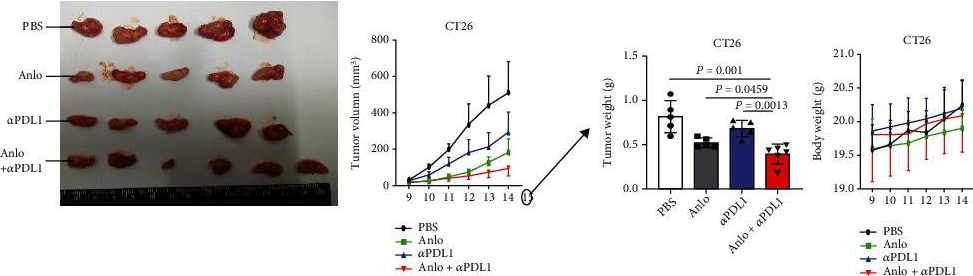
Anlotinib Benefits the αPDL1 Immunotherapy by Activating ROS/JNK/AP-1 Pathway to Upregulate PDL1 Expression in Colorectal Cancer.
In Oxidative Medicine and Cellular Longevity on 15 October 2022 by Luo, B., Zhang, S., et al.
PubMed
Colorectal cancer (CRC) is one of the prevalent malignant tumors. This study is aimed at evaluating the mechanism of anlotinib (anlo) on tumor microenvironment (TME) in CRC, and its effects in combination with immune checkpoint inhibitors (ICIs) therapy. Firstly, MC38 and CT26 cells were both exposed to different gradient concentrations of anlo for 72 h, to investigate the cell viability and synergetic therapy efficacy with ICIs by CCK8. The results showed that anlo could obviously inhibit cell growth and showed no synergistic efficacy therapy in combination with αPDL1 in vitro. Then, we found the upregulation of programmed cell death ligand 1(PDL1) expression both in vitro and in vivo after anlo treatment. In vivo, anlo could enhance the percentage of natural killer (NK) cells and M1 macrophage cells and decrease the percentage of M2 macrophage cells in TME. Moreover, we explored the mechanism and we proved that anlo could activate reactive oxygen species (ROS)/c-Jun N-terminal kinase (JNK)/activator protein-1 (AP-1) signaling pathway to increase the expression levels of PDL1, IFN-α/β/γ, and CXCL2 in two cell lines in vitro. We also proved that anlo had synergistic effects with ICIs in vivo. Finally, it could also increase the mRNA and protein PDL1 expression levels in human cell lines, which was consistent with mouse CRC cell lines. However, there are still a few limitations. On one hand, the ROS/JNK/AP-1 pathway needs to be proved whether it can be activated in human cell lines. On the other hand, the mechanism behind ROS promoting phosphorylation of JNK needs to be explored. Copyright © 2022 Bixian Luo et al.
- In Vitro,
- Mus musculus (House mouse),
- Immunology and Microbiology
Reprogramming alveolar macrophage responses to TGF-β reveals CCR2+ monocyte activity that promotes bronchiolitis obliterans syndrome.
In The Journal of Clinical Investigation on 3 October 2022 by Liu, Z., Liao, F., et al.
PubMed
Bronchiolitis obliterans syndrome (BOS) is a major impediment to lung transplant survival and is generally resistant to medical therapy. Extracorporeal photophoresis (ECP) is an immunomodulatory therapy that shows promise in stabilizing BOS patients, but its mechanisms of action are unclear. In a mouse lung transplant model, we show that ECP blunts alloimmune responses and inhibits BOS through lowering airway TGF-β bioavailability without altering its expression. Surprisingly, ECP-treated leukocytes were primarily engulfed by alveolar macrophages (AMs), which were reprogrammed to become less responsive to TGF-β and reduce TGF-β bioavailability through secretion of the TGF-β antagonist decorin. In untreated recipients, high airway TGF-β activity stimulated AMs to express CCL2, leading to CCR2+ monocyte-driven BOS development. Moreover, we found TGF-β receptor 2-dependent differentiation of CCR2+ monocytes was required for the generation of monocyte-derived AMs, which in turn promoted BOS by expanding tissue-resident memory CD8+ T cells that inflicted airway injury through Blimp-1-mediated granzyme B expression. Thus, through studying the effects of ECP, we have identified an AM functional plasticity that controls a TGF-β-dependent network that couples CCR2+ monocyte recruitment and differentiation to alloimmunity and BOS.
- Mus musculus (House mouse),
- Immunology and Microbiology
Reprogramming Alveolar Macrophage Responses to TGF-β Reveals CCR2sup>+/sup> Monocyte Activity that Promotes Bronchiolitis Obliterans Syndrome
Preprint on BioRxiv : the Preprint Server for Biology on 28 January 2022 by Liu, Z., Liao, F., et al.
PubMed
Bronchiolitis obliterans syndrome (BOS) is a major impediment to lung transplant survival and is generally resistant to medical therapy. Extracorporeal photophoresis (ECP) is an immunomodulatory therapy that shows promise in stabilizing BOS patients but its mechanisms of action are unclear. In a mouse lung transplant model, we show that ECP blunts alloimmune responses and inhibits BOS through lowering airway TGF-β bioavailability without altering its expression. Surprisingly, ECP-treated leukocytes are engulfed primarily by alveolar macrophages (AM), which become reprogrammed to become less responsive to TGF-β and reduce TGF-β bioavailability through secretion of the TGF-β antagonist Decorin. In untreated recipients, high airway TGF-β activity stimulates AM to express CCL2 leading to CCR2 + monocyte-driven BOS development. Moreover, we find TGF-β receptor 2-dependent differentiation of CCR2 + monocytes is required for the generation of monocyte-derived AM, which in turn promote BOS by expanding tissue-resident memory CD8 + T cells that inflict airway injury through Blimp-1-mediated Granzyme B expression. Thus, through studying the effects of ECP, we have identified an AM functional plasticity that controls a TGF-β-dependent network, which couples CCR2 + monocyte recruitment and differentiation to alloimmunity and BOS. Alveolar macrophage plasticity can be harnessed to prevent Bronchiolitis Obliterans Syndrome.
- Cancer Research,
- Immunology and Microbiology
The Interplay Between Regular T Cells and Immunotherapy in Cervical Cancer
Preprint on Research Square on 30 December 2020 by Xu, F., Zhang, F., et al.
PubMed
h4>Background: /h4> Immune checkpoint blockade inhibitors have aroused great expectation on many types of tumor eradication. However, the therapeutic effect of anti-PD-L1 treatment on cervical cancer is unsatisfactory and the potential antagonist is not very clear. Here, we investigated the therapeutic effect of anti-PD-L1 in cervical tumor mouse model and identified the potential threats for anti-PD-L1 therapeutic efficacy. h4>Results: /h4> we found that PD-L1 had a moderate expression in human and mouse cervical tumor cell lines and clinical samples compared to other tumor types and para-tumor tissue. Interestingly, our results showed that the anti-PD-L1 treated mice were dichotomously divided into responsive and unresponsive group even with the same genome background C57BL/6 syngeneic tumor model. The unresponsive tumors showed less immune cell infiltration and higher Tregs population induced immunosuppression activity than the responsive ones. Furthermore, we found that anti-PD-L1 autonomously upregulated Tregs proliferation and frequency in multiple immune organs, and, most importantly, Tregs depletion more significantly depressed the tumor growth rate and tumor weight than either anti-PD-L1 or anti-CD25 alone. Finally, we observed that the upregulating effector CD8+ T cell is associated with the better therapeutic effect of anti-PD-L1 therapy post Tregs depletion. h4>Conclusion: /h4> In conclusion, anti-PD-L1 therapy upregulates Tregs frequency and proliferation in tumor model, and the depletion of Tregs may be a useful adjuvant strategy for anti-PD-L1 therapy in the immunotherapy of cervical cancer.