InVivoMAb anti-human CTLA-4 (CD152)
Product Details
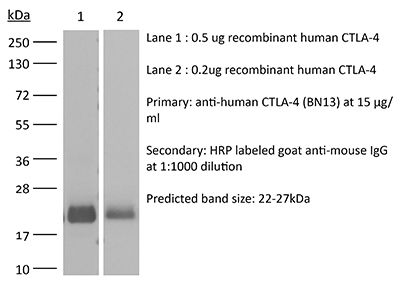
The BN13 monoclonal antibody reacts with human CTLA-4 (cytotoxic T lymphocyte antigen-4) also known as CD152. CTLA-4 is a 33 kDa cell surface receptor encoded by the Ctla4 gene that belongs to the CD28 family of the Ig superfamily. CTLA-4 is expressed on activated T and B lymphocytes. CTLA-4 is structurally similar to the T-cell co-stimulatory protein, CD28, and both molecules bind to the B7 family members B7-1 (CD80) and B7-2 (CD86). Upon ligand binding, CTLA-4 negatively regulates cell-mediated immune responses. CTLA-4 plays roles in induction and/or maintenance of immunological tolerance, thymocyte development, and regulation of protective immunity. The critical role of CTLA-4 in immune down-regulation has been demonstrated in CTLA-4 deficient mice, which succumb at 3-5 weeks of age due to the development of a lymphoproliferative disease. CTLA-4 is among a group of inhibitory receptors being explored as cancer treatment targets through immune checkpoint blockade. The BN13 antibody has been shown to neutralize CTLA-4 in vitro.Specifications
| Isotype | Mouse IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb mouse IgG2a isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Human CTLA-4 recombinant protein |
| Reported Applications |
in vitro CTLA-4 neutralization Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
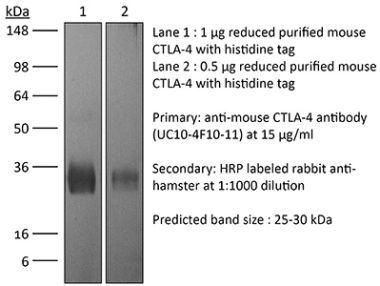
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10950635 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
Flow Cytometry
Bhela, S., et al. (2015). "Nonapoptotic and extracellular activity of granzyme B mediates resistance to regulatory T cell (Treg) suppression by HLA-DR-CD25hiCD127lo Tregs in multiple sclerosis and in response to IL-6" J Immunol 194(5): 2180-2189. PubMed
In autoimmune patients, regulatory T cells (Tregs) are increasingly found to be unable to suppress patient-derived T cells, an outcome referred to as Treg resistance. In this study, we show that CD4 T cells from patients with multiple sclerosis resist suppression by patient-derived or healthy donor-derived ex vivo Tregs. Importantly, we report that granzyme B (GzmB) contributes to this Treg resistance via a novel, apoptosis-independent mechanism. We show that memory CD4(+)CD127(lo)FOXP3(+) Treg subsets do not express GzmB, whereas activated, nonregulatory CD4 T cells isolated from patients with multiple sclerosis express higher levels of GzmB than do cells from healthy donors. In contrast to the intracellular GzmB that mediates apoptosis, GzmB can be found in extracellular fluids where it is hypothesized to regulate other cellular processes. In this study, we show that providing extracellular GzmB strongly inhibits Treg suppression, without altering Treg viability. However, when GzmB and GzmB-specific inhibitor are both provided to the cocultures, Treg suppression occurs. Thus, these data suggest that a novel activity of extracellular GzmB is to regulate Treg suppression. Additionally, we find that the suppression-abrogating cytokine IL-6 augments GzmB expression by human CD4 T cells, and it inhibits Treg suppression via this nonapoptotic GzmB-mediated mechanism. Lastly, in examining the mechanism whereby GzmB inhibits Treg function, we show that extracellular GzmB reduces Treg expression of CD39 and programmed death ligand 1. Collectively, these data indicate that extracellular GzmB plays an unexpected, nonapoptotic role in regulating Treg suppression and suggest that inactivation of specifically the extracellular activity of GzmB may be an efficacious therapeutic in autoimmunity.
Flow Cytometry
Gideon, H. P., et al. (2015). "Variability in tuberculosis granuloma T cell responses exists, but a balance of pro- and anti-inflammatory cytokines is associated with sterilization" PLoS Pathog 11(1): e1004603. PubMed
Lung granulomas are the pathologic hallmark of tuberculosis (TB). T cells are a major cellular component of TB lung granulomas and are known to play an important role in containment of Mycobacterium tuberculosis (Mtb) infection. We used cynomolgus macaques, a non-human primate model that recapitulates human TB with clinically active disease, latent infection or early infection, to understand functional characteristics and dynamics of T cells in individual granulomas. We sought to correlate T cell cytokine response and bacterial burden of each granuloma, as well as granuloma and systemic responses in individual animals. Our results support that each granuloma within an individual host is independent with respect to total cell numbers, proportion of T cells, pattern of cytokine response, and bacterial burden. The spectrum of these components overlaps greatly amongst animals with different clinical status, indicating that a diversity of granulomas exists within an individual host. On average only about 8% of T cells from granulomas respond with cytokine production after stimulation with Mtb specific antigens, and few “multi-functional” T cells were observed. However, granulomas were found to be “multi-functional” with respect to the combinations of functional T cells that were identified among lesions from individual animals. Although the responses generally overlapped, sterile granulomas had modestly higher frequencies of T cells making IL-17, TNF and any of T-1 (IFN-gamma, IL-2, or TNF) and/or T-17 (IL-17) cytokines than non-sterile granulomas. An inverse correlation was observed between bacterial burden with TNF and T-1/T-17 responses in individual granulomas, and a combinatorial analysis of pair-wise cytokine responses indicated that granulomas with T cells producing both pro- and anti-inflammatory cytokines (e.g. IL-10 and IL-17) were associated with clearance of Mtb. Preliminary evaluation suggests that systemic responses in the blood do not accurately reflect local T cell responses within granulomas.
Flow Cytometry
Otani, T., et al. (2011). "Stromal cells’ B7-1 is a key stimulatory molecule for interleukin-10 production by HOZOT, a multifunctional regulatory T-cell line" Immunol Cell Biol 89(2): 246-254. PubMed
We have previously shown that xenogeneic stromal cell stimulation of naive T cells resulted in the generation of a new type of regulatory T (Treg) cell termed HOZOT, which has multifunctional properties and a CD4/CD8 double-positive phenotype. Even after the establishment of HOZOT, stromal cells can function as an antigen-presenting cell (APC) by inducing these cells to produce interleukin (IL)-10. When compared with other stimuli, stromal cells showed an IL-10-producing ability comparable to anti-CD3 antibody (Ab) stimulation, and much greater than dendritic cell (DC) stimulation. Distinct from professional APCs, stromal cells express only major histocompatibility complex (MHC) class I and B7-1 costimulatory molecules, and not MHC class II or other costimulatory molecules, such as ICOSL (CD275), PD-L1 (CD274), PD-L2 (CD273), CD40, OX40L (CD252) and 4-1BBL (CD137L) in the absence of stimulation. Blocking experiments revealed that, in addition to anti-H-2K(d) Ab and anti-human CD8 Ab, anti-mouse B7-1 Ab could effectively block IL-10 production, indicating a key role of the B7-1/CD28 pathway. Using stromal cells expressing different levels of B7-1, IL-10 production correlated with the levels of B7-1 expression. Distinct from ICOSL or PD-L1 expressed on DCs (which are regarded as IL-10-inducing costimulatory molecules), this study showed that B7-1 on stromal cells is a key molecule regulating IL-10 production by multifunctional Treg cells, HOZOT.
in vitro CTLA-4 neutralization
Che, K. F., et al. (2010). "HIV-1 impairs in vitro priming of naive T cells and gives rise to contact-dependent suppressor T cells" Eur J Immunol 40(8): 2248-2258. PubMed
Priming of T cells in lymphoid tissues of HIV-infected individuals occurs in the presence of HIV-1. DC in this milieu activate T cells and disseminate HIV-1 to newly activated T cells, the outcome of which may have serious implications in the development of optimal antiviral responses. We investigated the effects of HIV-1 on DC-naive T-cell interactions using an allogeneic in vitro system. Our data demonstrate a dramatic decrease in the primary expansion of naive T cells when cultured with HIV-1-exposed DC. CD4(+) and CD8(+) T cells showed enhanced expression of PD-1 and TRAIL, whereas CTLA-4 expression was observed on CD4(+) T cells. It is worth noting that T cells primed in the presence of HIV-1 suppressed priming of other naive T cells in a contact-dependent manner. We identified PD-1, CTLA-4, and TRAIL pathways as responsible for this suppresion, as blocking these negative molecules restored T-cell proliferation to a higher degree. In conclusion, the presence of HIV-1 during DC priming produced cells with inhibitory effects on T-cell activation and proliferation, i.e. suppressor T cells, a mechanism that could contribute to the enhancement of HIV-1 pathogenesis.
Flow Cytometry
Barboza, L., et al. (2007). "Antigen-induced regulatory T cells in HBV chronically infected patients" Virology 368(1): 41-49. PubMed
T cell response against HBV is vigorous in patients with acute hepatitis who clear the virus, whereas it is weak and narrowly focused in patients with chronic disease. We report that following incubation with HBcAg, a population of CD4+FoxP3+ cells expressing phenotypic markers of both natural and induced Tregs, can be antigen-induced from peripheral mononuclear cells. Conversely, naive and naturally immune subjects did not increase CD4+FoxP3+ Tregs following stimulation with HBcAg, supporting the idea that natural Tregs are able to respond specifically to HBV antigen. Furthermore, increased frequencies of antigen-induced CD4+FoxP3+IL-10+ Tregs correlated with viral load, suggesting that antigen-induced Tregs could contribute to an inadequate response against the virus, leading to chronic infection and support the view that specific natural Tregs may be implicated in host immune tolerance during HBV infection.
Flow Cytometry
Pistillo, M. P., et al. (2003). "CTLA-4 is not restricted to the lymphoid cell lineage and can function as a target molecule for apoptosis induction of leukemic cells" Blood 101(1): 202-209. PubMed
The expression of cytotoxic T-lymphocyte antigen-4 (CTLA-4) molecule in human normal and neoplastic hematopoietic cells, both on the cell membrane and in the intracellular compartment, was evaluated. Flow cytometric analysis carried out with a panel of anti-CTLA-4 human single-chain fragment of variable domain (scFv) antibodies revealed that CTLA-4 was not expressed on the surface, whereas it was highly expressed within the cytoplasm, in freshly isolated peripheral blood mononuclear cells (PBMCs), T cells, B cells, CD34(+) stem cells, and granulocytes. Various treatments with agents able to specifically activate each cell type induced CTLA-4 expression on the surface of these cells. Similarly, increased CTLA-4 expression was observed in different hematopoietic cell lines although they also expressed surface CTLA-4, at different degrees of intensity, before activation. Surprisingly, CTLA-4 RNA transcripts were detectable in such cell lines only after nested polymerase chain reaction (PCR) specific for CTLA-4 extracellular domain, suggesting a very fast CTLA-4 RNA processing accompanied by prolonged CTLA-4 protein accumulation. We further demonstrated surface expression of CTLA-4 in a variety of acute and chronic myeloid leukemias (AMLs and CMLs) and B- and T-lymphoid leukemias, either adult or pediatric. CTLA-4 was expressed in 25% to 85% of AMLs and CMLs depending on the leukemia subtype and the epitope analyzed, whereas in acute B- and T-leukemias CTLA-4 expression was mainly cytoplasmic. Chronic B leukemias appeared to express CTLA-4, both on the surface and in cytoplasm, whereas few cases tested of chronic T leukemias were negative. Two anti-CTLA-4 immunotoxins (scFvs-saporin) induced in vitro apoptosis of neoplastic cells from a representative AML, suggesting a novel immunotherapeutic approach to AML based on CTLA-4 targeting.
- Cancer Research,
- Immunology and Microbiology
The novel reversible LSD1 inhibitor SP-2577 promotes anti-tumor immunity in SWItch/Sucrose-NonFermentable (SWI/SNF) complex mutated ovarian cancer.
In PLoS ONE on 11 July 2020 by Soldi, R., Ghosh Halder, T., et al.
PubMed
Mutations of the SWI/SNF chromatin remodeling complex occur in 20% of all human cancers, including ovarian cancer. Approximately half of ovarian clear cell carcinomas (OCCC) carry mutations in the SWI/SNF subunit ARID1A, while small cell carcinoma of the ovary hypercalcemic type (SCCOHT) presents with inactivating mutations of the SWI/SNF ATPase SMARCA4 alongside epigenetic silencing of the ATPase SMARCA2. Loss of these ATPases disrupts SWI/SNF chromatin remodeling activity and may also interfere with the function of other histone-modifying enzymes that associate with or are dependent on SWI/SNF activity. One such enzyme is lysine-specific histone demethylase 1 (LSD1/KDM1A), which regulates the chromatin landscape and gene expression by demethylating proteins such as histone H3. Cross-cancer analysis of the TCGA database shows that LSD1 is highly expressed in SWI/SNF-mutated tumors. SCCOHT and OCCC cell lines have shown sensitivity to the reversible LSD1 inhibitor SP-2577 (Seclidemstat), suggesting that SWI/SNF-deficient ovarian cancers are dependent on LSD1 activity. Moreover, it has been shown that inhibition of LSD1 stimulates interferon (IFN)-dependent anti-tumor immunity through induction of endogenous retroviral elements and may thereby overcome resistance to checkpoint blockade. In this study, we investigated the ability of SP-2577 to promote anti-tumor immunity and T-cell infiltration in SCCOHT and OCCC cell lines. We found that SP-2577 stimulated IFN-dependent anti-tumor immunity in SCCOHT and promoted the expression of PD-L1 in both SCCOHT and OCCC. Together, these findings suggest that the combination therapy of SP-2577 with checkpoint inhibitors may induce or augment immunogenic responses of SWI/SNF-mutated ovarian cancers and warrants further investigation.
High CTLA-4 expression on Th17 cells results in increased sensitivity to CTLA-4 coinhibition and resistance to belatacept.
In American Journal of Transplantation : Official Journal of the American Society of Transplantation and the American Society of Transplant Surgeons on 1 March 2014 by Krummey, S. M., Cheeseman, J. A., et al.
PubMed
The CD28/cytotoxic T-lymphocyte antigen 4 (CTLA-4)blocker belatacept selectively inhibits alloreactive T cell responses but is associated with a high incidence of acute rejection following renal transplantation,which led us to investigate the etiology of belatacept–resistant graft rejection. T cells can differentiate into functionally distinct subsets of memory T cellsthat collectively enable protection against diverse classes of pathogens and can cross-react with allogeneicantigen and mediate graft rejection. T helper 17(Th17) cells are a pro-inflammatory CD4+ lineage that provides immunity to pathogens and are pathogenic in autoimmune disease. We found that T helper 1 (Th1)and Th17 memory compartments contained a similar frequency of divided cells following allogeneic stimulation.Compared to Th1 cells, Th17 memory cells expressed significantly higher levels of the coinhibitory molecule CTLA-4. Stimulation in the presence of belatacept inhibited Th1 responses but augmented Th17 cells due to greater sensitivity to coinhibition by CTLA-4. Th17 cells from renal transplant recipients were resistant to ex vivo CD28/CTLA-4 blockade with belatacept, and an elevated frequency of Th17 memory cells was associated with acute rejection during belatacept therapy. These data highlight important differences in costimulatory and coinhibitory requirements of CD4+ memory subsets, and demonstrate that the heterogeneity of pathogen-derived memory has implications for immunomodulation strategies.