InVivoMAb anti-mouse CTLA-4 (CD152)
Product Details
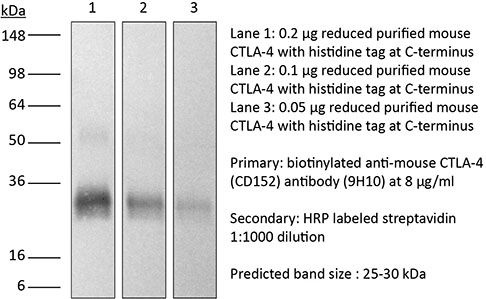
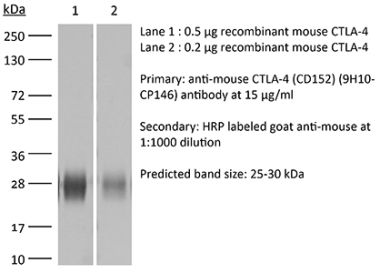
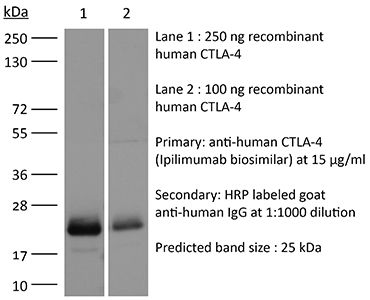
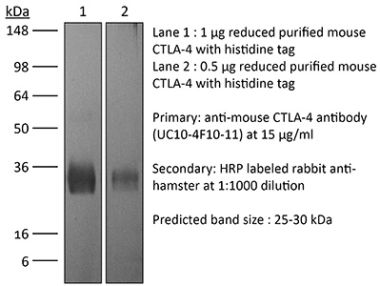
The 9H10 monoclonal antibody reacts with mouse CTLA-4 (cytotoxic T lymphocyte antigen-4) also known as CD152. CTLA-4 is a 33 kDa cell surface receptor encoded by the Ctla4 gene that belongs to the CD28 family of the Ig superfamily. CTLA-4 is expressed on activated T and B lymphocytes. CTLA-4 is structurally similar to the T-cell co-stimulatory protein, CD28, and both molecules bind to the B7 family members B7-1 (CD80) and B7-2 (CD86). Upon ligand binding, CTLA-4 negatively regulates cell-mediated immune responses. CTLA-4 plays roles in induction and/or maintenance of immunological tolerance, thymocyte development, and regulation of protective immunity. The critical role of CTLA-4 in immune down-regulation has been demonstrated in CTLA-4 deficient mice, which succumb at 3-5 weeks of age due to the development of a lymphoproliferative disease. CTLA-4 is among a group of inhibitory receptors being explored as cancer treatment targets through immune checkpoint blockade. The 9H10 antibody has been shown to promote T cell co-stimulation by blocking CTLA-4 binding to the B7 co-receptors, allowing for CD28 binding.Specifications
| Isotype | Syrian hamster IgG |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Syrian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse CTLA-4-human IgG1 fusion protein |
| Reported Applications |
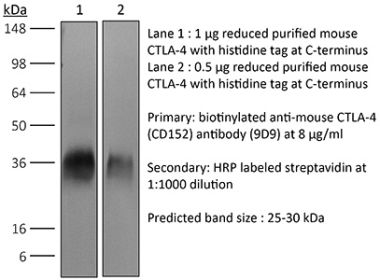
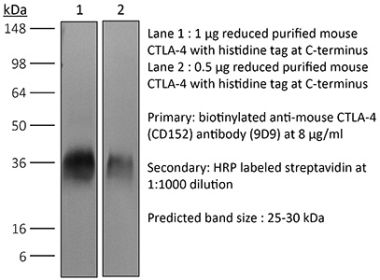
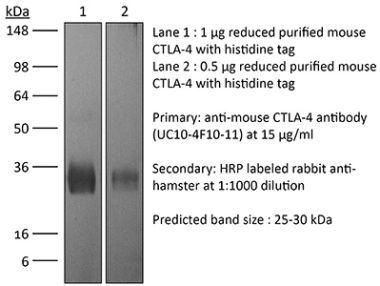
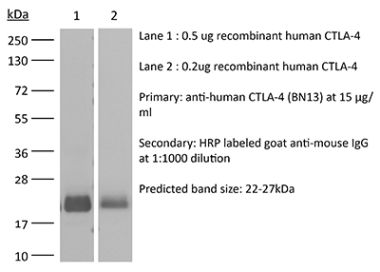
in vivo CTLA-4 neutralization in vitro CTLA-4 neutralization Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10950184 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo CTLA-4 neutralization
Ariyan, C. E., et al. (2018). "Robust Antitumor Responses Result from Local Chemotherapy and CTLA-4 Blockade" Cancer Immunol Res 6(2): 189-200. PubMed
Clinical responses to immunotherapy have been associated with augmentation of preexisting immune responses, manifested by heightened inflammation in the tumor microenvironment. However, many tumors have a noninflamed microenvironment, and response rates to immunotherapy in melanoma have been <50%. We approached this problem by utilizing immunotherapy (CTLA-4 blockade) combined with chemotherapy to induce local inflammation. In murine models of melanoma and prostate cancer, the combination of chemotherapy and CTLA-4 blockade induced a shift in the cellular composition of the tumor microenvironment, with infiltrating CD8(+) and CD4(+) T cells increasing the CD8/Foxp3 T-cell ratio. These changes were associated with improved survival of the mice. To translate these findings into a clinical setting, 26 patients with advanced melanoma were treated locally by isolated limb infusion with the nitrogen mustard alkylating agent melphalan followed by systemic administration of CTLA-4 blocking antibody (ipilimumab) in a phase II trial. This combination of local chemotherapy with systemic checkpoint blockade inhibitor resulted in a response rate of 85% at 3 months (62% complete and 23% partial response rate) and a 58% progression-free survival at 1 year. The clinical response was associated with increased T-cell infiltration, similar to that seen in the murine models. Together, our findings suggest that local chemotherapy combined with checkpoint blockade-based immunotherapy results in a durable response to cancer therapy.
in vivo CTLA-4 neutralization
Gao, J., et al. (2016). "Loss of IFN-gamma Pathway Genes in Tumor Cells as a Mechanism of Resistance to Anti-CTLA-4 Therapy" Cell 167(2): 397-404 e399. PubMed
Antibody blockade of the inhibitory CTLA-4 pathway has led to clinical benefit in a subset of patients with metastatic melanoma. Anti-CTLA-4 enhances T cell responses, including production of IFN-gamma, which is a critical cytokine for host immune responses. However, the role of IFN-gamma signaling in tumor cells in the setting of anti-CTLA-4 therapy remains unknown. Here, we demonstrate that patients identified as non-responders to anti-CTLA-4 (ipilimumab) have tumors with genomic defects in IFN-gamma pathway genes. Furthermore, mice bearing melanoma tumors with knockdown of IFN-gamma receptor 1 (IFNGR1) have impaired tumor rejection upon anti-CTLA-4 therapy. These data highlight that loss of the IFN-gamma signaling pathway is associated with primary resistance to anti-CTLA-4 therapy. Our findings demonstrate the importance of tumor genomic data, especially IFN-gamma related genes, as prognostic information for patients selected to receive treatment with immune checkpoint therapy.
in vivo CTLA-4 neutralization
Stephan, S. B., et al. (2015). "Biopolymer implants enhance the efficacy of adoptive T-cell therapy" Nat Biotechnol 33(1): 97-101. PubMed
Although adoptive T-cell therapy holds promise for the treatment of many cancers, its clinical utility has been limited by problems in delivering targeted lymphocytes to tumor sites, and the cells’ inefficient expansion in the immunosuppressive tumor microenvironment. Here we describe a bioactive polymer implant capable of delivering, expanding and dispersing tumor-reactive T cells. The approach can be used to treat inoperable or incompletely removed tumors by situating implants near them or at resection sites. Using a mouse breast cancer resection model, we show that the implants effectively support tumor-targeting T cells throughout resection beds and associated lymph nodes, and reduce tumor relapse compared to conventional delivery modalities. In a multifocal ovarian cancer model, we demonstrate that polymer-delivered T cells trigger regression, whereas injected tumor-reactive lymphocytes have little curative effect. Scaffold-based T-cell delivery may provide a viable treatment option for inoperable tumors and reduce the rate of metastatic relapse after surgery.
in vivo CTLA-4 neutralization
Spranger, S., et al. (2015). "Melanoma-intrinsic beta-catenin signalling prevents anti-tumour immunity" Nature 523(7559): 231-235. PubMed
Melanoma treatment is being revolutionized by the development of effective immunotherapeutic approaches. These strategies include blockade of immune-inhibitory receptors on activated T cells; for example, using monoclonal antibodies against CTLA-4, PD-1, and PD-L1 (refs 3-5). However, only a subset of patients responds to these treatments, and data suggest that therapeutic benefit is preferentially achieved in patients with a pre-existing T-cell response against their tumour, as evidenced by a baseline CD8(+) T-cell infiltration within the tumour microenvironment. Understanding the molecular mechanisms that underlie the presence or absence of a spontaneous anti-tumour T-cell response in subsets of cases, therefore, should enable the development of therapeutic solutions for patients lacking a T-cell infiltrate. Here we identify a melanoma-cell-intrinsic oncogenic pathway that contributes to a lack of T-cell infiltration in melanoma. Molecular analysis of human metastatic melanoma samples revealed a correlation between activation of the WNT/beta-catenin signalling pathway and absence of a T-cell gene expression signature. Using autochthonous mouse melanoma models we identified the mechanism by which tumour-intrinsic active beta-catenin signalling results in T-cell exclusion and resistance to anti-PD-L1/anti-CTLA-4 monoclonal antibody therapy. Specific oncogenic signals, therefore, can mediate cancer immune evasion and resistance to immunotherapies, pointing to new candidate targets for immune potentiation.
in vivo CTLA-4 neutralization
Twyman-Saint Victor, C., et al. (2015). "Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer" Nature 520(7547): 373-377. PubMed
Immune checkpoint inhibitors result in impressive clinical responses, but optimal results will require combination with each other and other therapies. This raises fundamental questions about mechanisms of non-redundancy and resistance. Here we report major tumour regressions in a subset of patients with metastatic melanoma treated with an anti-CTLA4 antibody (anti-CTLA4) and radiation, and reproduced this effect in mouse models. Although combined treatment improved responses in irradiated and unirradiated tumours, resistance was common. Unbiased analyses of mice revealed that resistance was due to upregulation of PD-L1 on melanoma cells and associated with T-cell exhaustion. Accordingly, optimal response in melanoma and other cancer types requires radiation, anti-CTLA4 and anti-PD-L1/PD-1. Anti-CTLA4 predominantly inhibits T-regulatory cells (Treg cells), thereby increasing the CD8 T-cell to Treg (CD8/Treg) ratio. Radiation enhances the diversity of the T-cell receptor (TCR) repertoire of intratumoral T cells. Together, anti-CTLA4 promotes expansion of T cells, while radiation shapes the TCR repertoire of the expanded peripheral clones. Addition of PD-L1 blockade reverses T-cell exhaustion to mitigate depression in the CD8/Treg ratio and further encourages oligoclonal T-cell expansion. Similarly to results from mice, patients on our clinical trial with melanoma showing high PD-L1 did not respond to radiation plus anti-CTLA4, demonstrated persistent T-cell exhaustion, and rapidly progressed. Thus, PD-L1 on melanoma cells allows tumours to escape anti-CTLA4-based therapy, and the combination of radiation, anti-CTLA4 and anti-PD-L1 promotes response and immunity through distinct mechanisms.
in vivo CTLA-4 neutralization
Bartkowiak, T., et al. (2015). "Unique potential of 4-1BB agonist antibody to promote durable regression of HPV+ tumors when combined with an E6/E7 peptide vaccine" Proc Natl Acad Sci U S A 112(38): E5290-5299. PubMed
Antibody modulation of T-cell coinhibitory (e.g., CTLA-4) or costimulatory (e.g., 4-1BB) receptors promotes clinical responses to a variety of cancers. Therapeutic cancer vaccination, in contrast, has produced limited clinical benefit and no curative therapies. The E6 and E7 oncoproteins of human papilloma virus (HPV) drive the majority of genital cancers, and many oropharyngeal tumors. We discovered 15-19 amino acid peptides from HPV-16 E6/E7 for which induction of T-cell immunity correlates with disease-free survival in patients treated for high-grade cervical neoplasia. We report here that intranasal vaccination with these peptides and the adjuvant alpha-galactosylceramide elicits systemic and mucosal T-cell responses leading to reduced HPV(+) TC-1 tumor growth and prolonged survival in mice. We hypothesized that the inability of these T cells to fully reject established tumors resulted from suppression in the tumor microenvironment which could be ameliorated through checkpoint modulation. Combining this E6/E7 peptide vaccine with checkpoint blockade produced only modest benefit; however, coadministration with a 4-1BB agonist antibody promoted durable regression of established genital TC-1 tumors. Relative to other therapies tested, this combination of vaccine and alpha4-1BB promoted the highest CD8(+) versus regulatory FoxP3(+) T-cell ratios, elicited 2- to 5-fold higher infiltration by E7-specific CTL, and evoked higher densities of highly cytotoxic TcEO (T cytotoxic Eomesodermin) CD8 (>70-fold) and ThEO (T helper Eomesodermin) CD4 (>17-fold) T cells. These findings have immediate clinical relevance both in terms of the direct clinical utility of the vaccine studied and in illustrating the potential of 4-1BB antibody to convert therapeutic E6/E7 vaccines already in clinical trials into curative therapies.
in vitro CTLA-4 neutralization
Krummey, S. M., et al. (2014). "Candida-elicited murine Th17 cells express high Ctla-4 compared with Th1 cells and are resistant to costimulation blockade" J Immunol 192(5): 2495-2504. PubMed
Effector and memory T cells may cross-react with allogeneic Ags to mediate graft rejection. Whereas the costimulation properties of Th1 cells are well studied, relatively little is known about the costimulation requirements of microbe-elicited Th17 cells. The costimulation blocker CTLA-4 Ig has been ineffective in the treatment of several Th17-driven autoimmune diseases and is associated with severe acute rejection following renal transplantation, leading us to investigate whether Th17 cells play a role in CD28/CTLA-4 blockade-resistant alloreactivity. We established an Ag-specific model in which Th1 and Th17 cells were elicited via Mycobacterium tuberculosis and Candida albicans immunization, respectively. C. albicans immunization elicited a higher frequency of Th17 cells and conferred resistance to costimulation blockade following transplantation. Compared with the M. tuberculosis group, C. albicans-elicited Th17 cells contained a higher frequency of IL-17(+)IFN-gamma(+) producers and a lower frequency of IL-10(+) and IL-10(+)IL-17(+) cells. Importantly, Th17 cells differentially regulated the CD28/CTLA-4 pathway, expressing similarly high CD28 but significantly greater amounts of CTLA-4 compared with Th1 cells. Ex vivo blockade experiments demonstrated that Th17 cells are more sensitive to CTLA-4 coinhibition and therefore less susceptible to CTLA-4 Ig. These novel insights into the differential regulation of CTLA-4 coinhibition on CD4(+) T cells have implications for the immunomodulation of pathologic T cell responses during transplantation and autoimmunity.
in vivo CTLA-4 neutralization
Ozdemir, B. C., et al. (2014). "Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival" Cancer Cell 25(6): 719-734. PubMed
Pancreatic ductal adenocarcinoma (PDAC) is associated with marked fibrosis and stromal myofibroblasts, but their functional contribution remains unknown. Transgenic mice with the ability to delete alphaSMA(+) myofibroblasts in pancreatic cancer were generated. Depletion starting at either noninvasive precursor (pancreatic intraepithelial neoplasia) or the PDAC stage led to invasive, undifferentiated tumors with enhanced hypoxia, epithelial-to-mesenchymal transition, and cancer stem cells, with diminished animal survival. In PDAC patients, fewer myofibroblasts in their tumors also correlated with reduced survival. Suppressed immune surveillance with increased CD4(+)Foxp3(+) Tregs was observed in myofibroblast-depleted mouse tumors. Although myofibroblast-depleted tumors did not respond to gemcitabine, anti-CTLA4 immunotherapy reversed disease acceleration and prolonged animal survival. This study underscores the need for caution in targeting carcinoma-associated fibroblasts in PDAC.
in vivo CTLA-4 neutralization
Hervieu, A., et al. (2013). "Dacarbazine-mediated upregulation of NKG2D ligands on tumor cells activates NK and CD8 T cells and restrains melanoma growth" J Invest Dermatol 133(2): 499-508. PubMed
Dacarbazine (DTIC) is a cytotoxic drug widely used for melanoma treatment. However, the putative contribution of anticancer immune responses in the efficacy of DTIC has not been evaluated. By testing how DTIC affects host immune responses to cancer in a mouse model of melanoma, we unexpectedly found that both natural killer (NK) and CD8(+) T cells were indispensable for DTIC therapeutic effect. Although DTIC did not directly affect immune cells, it triggered the upregulation of NKG2D ligands on tumor cells, leading to NK cell activation and IFNgamma secretion in mice and humans. NK cell-derived IFNgamma subsequently favored upregulation of major histocompatibility complex class I molecules on tumor cells, rendering them sensitive to cytotoxic CD8(+) T cells. Accordingly, DTIC markedly enhanced cytotoxic T lymphocyte antigen 4 inhibition efficacy in vivo in an NK-dependent manner. These results underscore the immunogenic properties of DTIC and provide a rationale to combine DTIC with immunotherapeutic agents that relieve immunosuppression in vivo.
in vivo CTLA-4 neutralization
Goding, S. R., et al. (2013). "Restoring immune function of tumor-specific CD4+ T cells during recurrence of melanoma" J Immunol 190(9): 4899-4909. PubMed
Recurrent solid malignancies are often refractory to standard therapies. Although adoptive T cell transfer may benefit select individuals, the majority of patients succumb to their disease. To address this important clinical dilemma, we developed a mouse melanoma model in which initial regression of advanced disease was followed by tumor recurrence. During recurrence, Foxp3(+) tumor-specific CD4(+) T cells became PD-1(+) and represented >60% of the tumor-specific CD4(+) T cells in the host. Concomitantly, tumor-specific CD4(+) T effector cells showed traits of chronic exhaustion, as evidenced by their high expression of the PD-1, TIM-3, 2B4, TIGIT, and LAG-3 inhibitory molecules. Although blockade of the PD-1/PD-L1 pathway with anti-PD-L1 Abs or depletion of tumor-specific regulatory T cells (Tregs) alone failed to reverse tumor recurrence, the combination of PD-L1 blockade with tumor-specific Treg depletion effectively mediated disease regression. Furthermore, blockade with a combination of anti-PD-L1 and anti-LAG-3 Abs overcame the requirement to deplete tumor-specific Tregs. In contrast, successful treatment of primary melanoma with adoptive cell therapy required only Treg depletion or Ab therapy, underscoring the differences in the characteristics of treatment between primary and relapsing cancer. These data highlight the need for preclinical development of combined immunotherapy approaches specifically targeting recurrent disease.
in vivo CTLA-4 neutralization
Waitz, R., et al. (2012). "Potent induction of tumor immunity by combining tumor cryoablation with anti-CTLA-4 therapy" Cancer Res 72(2): 430-439. PubMed
Thermal ablation to destroy tumor tissue may help activate tumor-specific T cells by elevating the presentation of tumor antigens to the immune system. However, the antitumor activity of these T cells may be restrained by their expression of the inhibitory T-cell coreceptor CTLA-4, the target of the recently U.S. Food and Drug Administration-approved antibody drug ipilumimab. By relieving this restraint, CTLA-4-blocking antibodies such as ipilumimab can promote tumor rejection, but the full scope of their most suitable applications has yet to be fully determined. In this study, we offer a preclinical proof-of-concept in the TRAMP C2 mouse model of prostate cancer that CTLA-4 blockade cooperates with cryoablation of a primary tumor to prevent the outgrowth of secondary tumors seeded by challenge at a distant site. Although growth of secondary tumors was unaffected by cryoablation alone, the combination treatment was sufficient to slow growth or trigger rejection. In addition, secondary tumors were highly infiltrated by CD4(+) T cells and CD8(+) T cells, and there was a significant increase in the ratio of intratumoral T effector cells to CD4(+)FoxP3(+) T regulatory cells, compared with monotherapy. These findings documented for the first time an effect of this immunotherapeutic intervention on the intratumoral accumulation and systemic expansion of CD8(+) T cells specific for the TRAMP C2-specific antigen SPAS-1. Although cryoablation is currently used to treat a targeted tumor nodule, our results suggest that combination therapy with CTLA-4 blockade will augment antitumor immunity and rejection of tumor metastases in this setting.
in vivo CTLA-4 neutralization
Balachandran, V. P., et al. (2011). "Imatinib potentiates antitumor T cell responses in gastrointestinal stromal tumor through the inhibition of Ido" Nat Med 17(9): 1094-1100. PubMed
Imatinib mesylate targets mutated KIT oncoproteins in gastrointestinal stromal tumor (GIST) and produces a clinical response in 80% of patients. The mechanism is believed to depend predominantly on the inhibition of KIT-driven signals for tumor-cell survival and proliferation. Using a mouse model of spontaneous GIST, we found that the immune system contributes substantially to the antitumor effects of imatinib. Imatinib therapy activated CD8(+) T cells and induced regulatory T cell (T(reg) cell) apoptosis within the tumor by reducing tumor-cell expression of the immunosuppressive enzyme indoleamine 2,3-dioxygenase (Ido). Concurrent immunotherapy augmented the efficacy of imatinib in mouse GIST. In freshly obtained human GIST specimens, the T cell profile correlated with imatinib sensitivity and IDO expression. Thus, T cells are crucial to the antitumor effects of imatinib in GIST, and concomitant immunotherapy may further improve outcomes in human cancers treated with targeted agents.
in vivo CTLA-4 neutralization
Pedicord, V. A., et al. (2011). "Single dose of anti-CTLA-4 enhances CD8+ T-cell memory formation, function, and maintenance" Proc Natl Acad Sci U S A 108(1): 266-271. PubMed
CTLA-4, an Ig superfamily molecule with homology to CD28, is one of the most potent negative regulators of T-cell responses. In vivo blockade of CTLA-4 exacerbates autoimmunity, enhances tumor-specific T-cell responses, and may inhibit the induction of T-cell anergy. Clinical trials of CTLA-4-blocking antibodies to augment T-cell responses to malignant melanoma are at an advanced stage; however, little is known about the effects of CTLA-4 blockade on memory CD8(+) T-cell responses and the formation and maintenance of long-term CD8(+) T-cell memory. In our studies, we show that during in vivo memory CD8(+) T-cell responses to Listeria monocytogenes infection, CTLA-4 blockade enhances bacterial clearance and increases memory CD8(+) T-cell expansion. This is followed by an accumulation of memory cells that are capable of producing the effector cytokines IFN-gamma and TNF-alpha. We also demonstrate that in a vaccination setting, blocking CTLA-4 during CD8(+) T-cell priming leads to increased expansion and maintenance of antigen-specific memory CD8(+) T cells without adversely affecting the overall T-cell repertoire. This leads to an increase in memory cell effector function and improved protective immunity against further bacterial challenges. These results indicate that transient blockade of CTLA-4 enhances memory CD8(+) T-cell responses and support the possible use of CTLA-4-blocking antibodies during vaccination to augment memory formation and maintenance.
in vivo CTLA-4 neutralization
Quezada, S. A., et al. (2010). "Tumor-reactive CD4(+) T cells develop cytotoxic activity and eradicate large established melanoma after transfer into lymphopenic hosts" J Exp Med 207(3): 637-650. PubMed
Adoptive transfer of large numbers of tumor-reactive CD8(+) cytotoxic T lymphocytes (CTLs) expanded and differentiated in vitro has shown promising clinical activity against cancer. However, such protocols are complicated by extensive ex vivo manipulations of tumor-reactive cells and have largely focused on CD8(+) CTLs, with much less emphasis on the role and contribution of CD4(+) T cells. Using a mouse model of advanced melanoma, we found that transfer of small numbers of naive tumor-reactive CD4(+) T cells into lymphopenic recipients induces substantial T cell expansion, differentiation, and regression of large established tumors without the need for in vitro manipulation. Surprisingly, CD4(+) T cells developed cytotoxic activity, and tumor rejection was dependent on class II-restricted recognition of tumors by tumor-reactive CD4(+) T cells. Furthermore, blockade of the coinhibitory receptor CTL-associated antigen 4 (CTLA-4) on the transferred CD4(+) T cells resulted in greater expansion of effector T cells, diminished accumulation of tumor-reactive regulatory T cells, and superior antitumor activity capable of inducing regression of spontaneous mouse melanoma. These findings suggest a novel potential therapeutic role for cytotoxic CD4(+) T cells and CTLA-4 blockade in cancer immunotherapy, and demonstrate the potential advantages of differentiating tumor-reactive CD4(+) cells in vivo over current protocols favoring in vitro expansion and differentiation.
- Mus musculus (House mouse),
- Immunology and Microbiology
Inhibition of IL-25/IL-17RA improves immune-related adverse events of checkpoint inhibitors and reveals antitumor activity.
In Journal for Immunotherapy of Cancer on 21 March 2024 by Hu, X., Bukhari, S. M., et al.
PubMed
Immune checkpoint inhibitors (ICIs) have improved outcomes and extended patient survival in several tumor types. However, ICIs often induce immune-related adverse events (irAEs) that warrant therapy cessation, thereby limiting the overall effectiveness of this class of therapeutic agents. Currently, available therapies used to treat irAEs might also blunt the antitumor activity of the ICI themselves. Therefore, there is an urgent need to identify treatments that have the potential to be administered alongside ICI to optimize their use. Using a translationally relevant murine model of anti-PD-1 and anti-CTLA-4 antibodies-induced irAEs, we compared the safety and efficacy of prednisolone, anti-IL-6, anti-TNFɑ, anti-IL-25 (IL-17E), and anti-IL-17RA (the receptor for IL-25) administration to prevent irAEs and to reduce tumor size. While all interventions were adequate to inhibit the onset of irAEs pneumonitis and hepatitis, treatment with anti-IL-25 or anti-IL-17RA antibodies also exerted additional antitumor activity. Mechanistically, IL-25/IL-17RA blockade reduced the number of organ-infiltrating lymphocytes. These findings suggest that IL-25/IL-17RA may serve as an additional target when treating ICI-responsive tumors, allowing for better tumor control while suppressing immune-related toxicities. © Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
CD4 T cell-activating neoantigens enhance personalized cancer vaccine efficacy.
In JCI Insight on 8 December 2023 by Huff, A. L., Longway, G., et al.
PubMed
Personalized cancer vaccines aim to activate and expand cytotoxic antitumor CD8+ T cells to recognize and kill tumor cells. However, the role of CD4+ T cell activation in the clinical benefit of these vaccines is not well defined. We previously established a personalized neoantigen vaccine (PancVAX) for the pancreatic cancer cell line Panc02, which activates tumor-specific CD8+ T cells but required combinatorial checkpoint modulators to achieve therapeutic efficacy. To determine the effects of neoantigen-specific CD4+ T cell activation, we generated a vaccine (PancVAX2) targeting both major histocompatibility complex class I- (MHCI-) and MHCII-specific neoantigens. Tumor-bearing mice vaccinated with PancVAX2 had significantly improved control of tumor growth and long-term survival benefit without concurrent administration of checkpoint inhibitors. PancVAX2 significantly enhanced priming and recruitment of neoantigen-specific CD8+ T cells into the tumor with lower PD-1 expression after reactivation compared with the CD8+ vaccine alone. Vaccine-induced neoantigen-specific Th1 CD4+ T cells in the tumor were associated with decreased Tregs. Consistent with this, PancVAX2 was associated with more proimmune myeloid-derived suppressor cells and M1-like macrophages in the tumor, demonstrating a less immunosuppressive tumor microenvironment. This study demonstrates the biological importance of prioritizing and including CD4+ T cell-specific neoantigens for personalized cancer vaccine modalities.
- Cancer Research
Opaganib (ABC294640) Induces Immunogenic Tumor Cell Death and Enhances Checkpoint Antibody Therapy.
In International Journal of Molecular Sciences on 29 November 2023 by Maines, L. W., Keller, S. N., et al.
PubMed
Antibody-based cancer drugs that target the checkpoint proteins CTLA-4, PD-1 and PD-L1 provide marked improvement in some patients with deadly diseases such as lung cancer and melanoma. However, most patients are either unresponsive or relapse following an initial response, underscoring the need for further improvement in immunotherapy. Certain drugs induce immunogenic cell death (ICD) in tumor cells in which the dying cells promote immunologic responses in the host that may enhance the in vivo activity of checkpoint antibodies. Sphingolipid metabolism is a key pathway in cancer biology, in which ceramides and sphingosine 1-phosphate (S1P) regulate tumor cell death, proliferation and drug resistance, as well as host inflammation and immunity. In particular, sphingosine kinases are key sites for manipulation of the ceramide/S1P balance that regulates tumor cell proliferation and sensitivity to radiation and chemotherapy. We and others have demonstrated that inhibition of sphingosine kinase-2 by the small-molecule investigational drug opaganib (formerly ABC294640) kills tumor cells and increases their sensitivities to other drugs and radiation. Because sphingolipids have been shown to regulate ICD, opaganib may induce ICD and improve the efficacy of checkpoint antibodies for cancer therapy. This was demonstrated by showing that in vitro treatment with opaganib increases the surface expression of the ICD marker calreticulin on a variety of tumor cell types. In vivo confirmation was achieved using the gold standard immunization assay in which B16 melanoma, Lewis lung carcinoma (LLC) or Neuro-2a neuroblastoma cells were treated with opaganib in vitro and then injected subcutaneously into syngeneic mice, followed by implantation of untreated tumor cells 7 days later. In all cases, immunization with opaganib-treated cells strongly suppressed the growth of subsequently injected tumor cells. Interestingly, opaganib treatment induced crossover immunity in that opaganib-treated B16 cells suppressed the growth of both untreated B16 and LLC cells and opaganib-treated LLC cells inhibited the growth of both untreated LLC and B16 cells. Next, the effects of opaganib in combination with a checkpoint antibody on tumor growth in vivo were assessed. Opaganib and anti-PD-1 antibody each slowed the growth of B16 tumors and improved mouse survival, while the combination of opaganib plus anti-PD-1 strongly suppressed tumor growth and improved survival (p < 0.0001). Individually, opaganib and anti-CTLA-4 antibody had modest effects on the growth of LLC tumors and mouse survival, whereas the combination of opaganib with anti-CTLA-4 substantially inhibited tumor growth and increased survival (p < 0.001). Finally, the survival of mice bearing B16 tumors was only marginally improved by opaganib or anti-PD-L1 antibody alone but was nearly doubled by the drugs in combination (p < 0.005). Overall, these studies demonstrate the ability of opaganib to induce ICD in tumor cells, which improves the antitumor activity of checkpoint antibodies.
- Mus musculus (House mouse),
- Immunology and Microbiology
Local and distant response to intratumoral immunotherapy assessed by immunoPET in mice.
In Journal for Immunotherapy of Cancer on 1 November 2023 by Meyblum, L., Chevaleyre, C., et al.
PubMed
Despite the promising efficacy of immune checkpoint blockers (ICB), tumor resistance and immune-related adverse events hinder their success in cancer treatment. To address these challenges, intratumoral delivery of immunotherapies has emerged as a potential solution, aiming to mitigate side effects through reduced systemic exposure while increasing effectiveness by enhancing local bioavailability. However, a comprehensive understanding of the local and systemic distribution of ICBs following intratumoral administration, as well as their impact on distant tumors, remains crucial for optimizing their therapeutic potential.To comprehensively investigate the distribution patterns following the intratumoral and intravenous administration of radiolabeled anti-cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and to assess its corresponding efficacy in both injected and non-injected tumors, we conducted an immunoPET imaging study. CT26 and MC38 syngeneic colorectal tumor cells were implanted subcutaneously on both flanks of Balb/c and C57Bl/6 mice, respectively. Hamster anti-mouse CTLA-4 antibody (9H10) labeled with zirconium-89 ([89Zr]9H10) was intratumorally or intravenously administered. Whole-body distribution of the antibody was monitored by immunoPET imaging (n=12 CT26 Balb/c mice, n=10 MC38 C57Bl/6 mice). Tumorous responses to injected doses (1-10 mg/kg) were correlated with specific uptake of [89Zr]9H10 (n=24). Impacts on the tumor microenvironment were assessed by immunofluorescence and flow cytometry. Half of the dose was cleared into the blood 1 hour after intratumoral administration. Despite this, 7 days post-injection, 6-8% of the dose remained in the intratumoral-injected tumors. CT26 tumors with prolonged ICB exposure demonstrated complete responses. Seven days post-injection, the contralateral non-injected tumor uptake of the ICB was comparable to the one achieved through intravenous administration (7.5±1.7% ID.cm-3 and 7.6±2.1% ID.cm-3, respectively) at the same dose in the CT26 model. This observation was confirmed in the MC38 model. Consistent intratumoral pharmacodynamic effects were observed in both intratumoral and intravenous treatment groups, as evidenced by a notable increase in CD8+T cells within the CT26 tumors following treatment. ImmunoPET-derived pharmacokinetics supports intratumoral injection of ICBs to decrease systemic exposure while maintaining efficacy compared with intravenous. Intratumoral-ICBs lead to high local drug exposure while maintaining significant therapeutic exposure in non-injected tumors. This immunoPET approach is applicable for clinical practice to support evidence-based drug development. © Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
A2AR eGFP reporter mouse enables elucidation of A2AR expression dynamics during anti-tumor immune responses.
In Nature Communications on 1 November 2023 by Todd, K. L., Lai, J., et al.
PubMed
There is significant clinical interest in targeting adenosine-mediated immunosuppression, with several small molecule inhibitors having been developed for targeting the A2AR receptor. Understanding of the mechanism by which A2AR is regulated has been hindered by difficulty in identifying the cell types that express A2AR due to a lack of robust antibodies for these receptors. To overcome this limitation, here an A2AR eGFP reporter mouse is developed, enabling the expression of A2AR during ongoing anti-tumor immune responses to be assessed. This reveals that A2AR is highly expressed on all tumor-infiltrating lymphocyte subsets including Natural Killer (NK) cells, NKT cells, γδ T cells, conventional CD4+ and CD8+ T lymphocytes and on a MHCIIhiCD86hi subset of type 2 conventional dendritic cells. In response to PD-L1 blockade, the emergence of PD-1+A2AR- cells correlates with successful therapeutic responses, whilst IL-18 is identified as a cytokine that potently upregulates A2AR and synergizes with A2AR deficiency to improve anti-tumor immunity. These studies provide insight into the biology of A2AR in the context of anti-tumor immunity and reveals potential combination immunotherapy approaches. © 2023. The Author(s).
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology,
- Genetics
Targeting nucleic acid sensors in tumor cells to reprogram biogenesis and RNA cargo of extracellular vesicles for T cell-mediated cancer immunotherapy.
In Cell Reports Medicine on 19 September 2023 by Heidegger, S., Stritzke, F., et al.
PubMed
Tumor-derived extracellular vesicles (EVs) have been associated with immune evasion and tumor progression. We show that the RNA-sensing receptor RIG-I within tumor cells governs biogenesis and immunomodulatory function of EVs. Cancer-intrinsic RIG-I activation releases EVs, which mediate dendritic cell maturation and T cell antitumor immunity, synergizing with immune checkpoint blockade. Intact RIG-I, autocrine interferon signaling, and the GTPase Rab27a in tumor cells are required for biogenesis of immunostimulatory EVs. Active intrinsic RIG-I signaling governs composition of the tumor EV RNA cargo including small non-coding stimulatory RNAs. High transcriptional activity of EV pathway genes and RIG-I in melanoma samples associate with prolonged patient survival and beneficial response to immunotherapy. EVs generated from human melanoma after RIG-I stimulation induce potent antigen-specific T cell responses. We thus define a molecular pathway that can be targeted in tumors to favorably alter EV immunomodulatory function. We propose "reprogramming" of tumor EVs as a personalized strategy for T cell-mediated cancer immunotherapy. Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
Development of a Patient-Derived 3D Immuno-Oncology Platform to Potentiate Immunotherapy Responses in Ascites-Derived Circulating Tumor Cells.
In Cancers on 16 August 2023 by Gerton, T. J., Green, A., et al.
PubMed
High-grade serous ovarian cancer (HGSOC) is responsible for the majority of gynecology cancer-related deaths. Patients in remission often relapse with more aggressive forms of disease within 2 years post-treatment. Alternative immuno-oncology (IO) strategies, such as immune checkpoint blockade (ICB) targeting the PD-(L)1 signaling axis, have proven inefficient so far. Our aim is to utilize epigenetic modulators to maximize the benefit of personalized IO combinations in ex vivo 3D patient-derived platforms and in vivo syngeneic models. Using patient-derived tumor ascites, we optimized an ex vivo 3D screening platform (PDOTS), which employs autologous immune cells and circulating ascites-derived tumor cells, to rapidly test personalized IO combinations. Most importantly, patient responses to platinum chemotherapy and poly-ADP ribose polymerase inhibitors in 3D platforms recapitulate clinical responses. Furthermore, similar to clinical trial results, responses to ICB in PDOTS tend to be low and positively correlated with the frequency of CD3+ immune cells and EPCAM+/PD-L1+ tumor cells. Thus, the greatest response observed with anti-PD-1/anti-PD-L1 immunotherapy alone is seen in patient-derived HGSOC ascites, which present with high levels of systemic CD3+ and PD-L1+ expression in immune and tumor cells, respectively. In addition, priming with epigenetic adjuvants greatly potentiates ICB in ex vivo 3D testing platforms and in vivo tumor models. We further find that epigenetic priming induces increased tumor secretion of several key cytokines known to augment T and NK cell activation and cytotoxicity, including IL-6, IP-10 (CXCL10), KC (CXCL1), and RANTES (CCL5). Moreover, epigenetic priming alone and in combination with ICB immunotherapy in patient-derived PDOTS induces rapid upregulation of CD69, a reliable early activation of immune markers in both CD4+ and CD8+ T cells. Consequently, this functional precision medicine approach could rapidly identify personalized therapeutic combinations able to potentiate ICB, which is a great advantage, especially given the current clinical difficulty of testing a high number of potential combinations in patients.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Membrane-localized neoantigens predict the efficacy of cancer immunotherapy.
In Cell Reports Medicine on 15 August 2023 by Goldberger, Z., Hauert, S., et al.
PubMed
Immune checkpoint immunotherapy (ICI) can re-activate immune reactions against neoantigens, leading to remarkable remission in cancer patients. Nevertheless, only a minority of patients are responsive to ICI, and approaches for prediction of responsiveness are needed to improve the success of cancer treatments. While the tumor mutational burden (TMB) correlates positively with responsiveness and survival of patients undergoing ICI, the influence of the subcellular localizations of the neoantigens remains unclear. Here, we demonstrate in both a mouse melanoma model and human clinical datasets of 1,722 ICI-treated patients that a high proportion of membrane-localized neoantigens, particularly at the plasma membrane, correlate with responsiveness to ICI therapy and improved overall survival across multiple cancer types. We further show that combining membrane localization and TMB analyses can enhance the predictability of cancer patient response to ICI. Our results may have important implications for establishing future clinical guidelines to direct the choice of treatment toward ICI. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Genetics
METTL1 promotes tumorigenesis through tRNA-derived fragment biogenesis in prostate cancer.
In Molecular Cancer on 29 July 2023 by García-Vílchez, R., Añazco-Guenkova, A. M., et al.
PubMed
Newly growing evidence highlights the essential role that epitranscriptomic marks play in the development of many cancers; however, little is known about the role and implications of altered epitranscriptome deposition in prostate cancer. Here, we show that the transfer RNA N7-methylguanosine (m7G) transferase METTL1 is highly expressed in primary and advanced prostate tumours. Mechanistically, we find that METTL1 depletion causes the loss of m7G tRNA methylation and promotes the biogenesis of a novel class of small non-coding RNAs derived from 5'tRNA fragments. 5'tRNA-derived small RNAs steer translation control to favour the synthesis of key regulators of tumour growth suppression, interferon pathway, and immune effectors. Knockdown of Mettl1 in prostate cancer preclinical models increases intratumoural infiltration of pro-inflammatory immune cells and enhances responses to immunotherapy. Collectively, our findings reveal a therapeutically actionable role of METTL1-directed m7G tRNA methylation in cancer cell translation control and tumour biology. © 2023. The Author(s).
- Cancer Research,
- Immunology and Microbiology
PD-L1 methylation restricts PD-L1/PD-1 interactions to control cancer immune surveillance.
In Science Advances on 26 May 2023 by Changsheng, H., Ren, S., et al.
PubMed
Immune checkpoint inhibitors targeting programmed cell death protein 1 (PD-1) or programmed cell death 1 ligand 1 (PD-L1) have enabled some patients with cancer to experience durable, complete treatment responses; however, reliable anti-PD-(L)1 treatment response biomarkers are lacking. Our research found that PD-L1 K162 was methylated by SETD7 and demethylated by LSD2. Furthermore, PD-L1 K162 methylation controlled the PD-1/PD-L1 interaction and obviously enhanced the suppression of T cell activity controlling cancer immune surveillance. We demonstrated that PD-L1 hypermethylation was the key mechanism for anti-PD-L1 therapy resistance, investigated that PD-L1 K162 methylation was a negative predictive marker for anti-PD-1 treatment in patients with non-small cell lung cancer, and showed that the PD-L1 K162 methylation:PD-L1 ratio was a more accurate biomarker for predicting anti-PD-(L)1 therapy sensitivity. These findings provide insights into the regulation of the PD-1/PD-L1 pathway, identify a modification of this critical immune checkpoint, and highlight a predictive biomarker of the response to PD-1/PD-L1 blockade therapy.
- Cancer Research,
- Immunology and Microbiology
Immune checkpoint B7-H3 is a therapeutic vulnerability in prostate cancer harboring PTEN and TP53 deficiencies.
In Science Translational Medicine on 10 May 2023 by Shi, W., Wang, Y., et al.
PubMed
Checkpoint immunotherapy has yielded meaningful responses across many cancers but has shown modest efficacy in advanced prostate cancer. B7 homolog 3 protein (B7-H3/CD276) is an immune checkpoint molecule and has emerged as a promising therapeutic target. However, much remains to be understood regarding B7-H3's role in cancer progression, predictive biomarkers for B7-H3-targeted therapy, and combinatorial strategies. Our multi-omics analyses identified B7-H3 as one of the most abundant immune checkpoints in prostate tumors containing PTEN and TP53 genetic inactivation. Here, we sought in vivo genetic evidence for, and mechanistic understanding of, the role of B7-H3 in PTEN/TP53-deficient prostate cancer. We found that loss of PTEN and TP53 induced B7-H3 expression by activating transcriptional factor Sp1. Prostate-specific deletion of Cd276 resulted in delayed tumor progression and reversed the suppression of tumor-infiltrating T cells and NK cells in Pten/Trp53 genetically engineered mouse models. Furthermore, we tested the efficacy of the B7-H3 inhibitor in preclinical models of castration-resistant prostate cancer (CRPC). We demonstrated that enriched regulatory T cells and elevated programmed cell death ligand 1 (PD-L1) in myeloid cells hinder the therapeutic efficacy of B7-H3 inhibition in prostate tumors. Last, we showed that B7-H3 inhibition combined with blockade of PD-L1 or cytotoxic T lymphocyte-associated protein 4 (CTLA-4) achieved durable antitumor effects and had curative potential in a PTEN/TP53-deficient CRPC model. Given that B7-H3-targeted therapies have been evaluated in early clinical trials, our studies provide insights into the potential of biomarker-driven combinatorial immunotherapy targeting B7-H3 in prostate cancer, among other malignancies.
- In Vivo,
- Mus musculus (House mouse),
- Cancer Research
Lymphocyte networks are dynamic cellular communities in the immunoregulatory landscape of lung adenocarcinoma.
In Cancer Cell on 8 May 2023 by Gaglia, G., Burger, M. L., et al.
PubMed
Lymphocytes are key for immune surveillance of tumors, but our understanding of the spatial organization and physical interactions that facilitate lymphocyte anti-cancer functions is limited. We used multiplexed imaging, quantitative spatial analysis, and machine learning to create high-definition maps of lung tumors from a Kras/Trp53-mutant mouse model and human resections. Networks of interacting lymphocytes ("lymphonets") emerged as a distinctive feature of the anti-cancer immune response. Lymphonets nucleated from small T cell clusters and incorporated B cells with increasing size. CXCR3-mediated trafficking modulated lymphonet size and number, but T cell antigen expression directed intratumoral localization. Lymphonets preferentially harbored TCF1+ PD-1+ progenitor CD8+ T cells involved in responses to immune checkpoint blockade (ICB) therapy. Upon treatment of mice with ICB or an antigen-targeted vaccine, lymphonets retained progenitor and gained cytotoxic CD8+ T cell populations, likely via progenitor differentiation. These data show that lymphonets create a spatial environment supportive of CD8+ T cell anti-tumor responses. Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology
Dendritic cell therapy augments antitumor immunity triggered by CDK4/6 inhibition and immune checkpoint blockade by unleashing systemic CD4 T-cell responses.
In Journal for Immunotherapy of Cancer on 1 May 2023 by Kumar, A., Ramani, V., et al.
PubMed
Cyclin-dependent kinase 4/6 inhibitors (CDK4/6i) combined with endocrine therapy are a mainstay treatment for hormone receptor-positive breast cancer. While their principal mechanism is inhibition of cancer cell proliferation, preclinical and clinical evidence suggests that CDK4/6i can also promote antitumor T-cell responses. However, this pro-immunogenic property is yet to be successfully harnessed in the clinic, as combining CDK4/6i with immune checkpoint blockade (ICB) has not shown a definitive benefit in patients. We performed an in-depth analysis of the changes in the tumor immune microenvironment and systemic immune modulation associated with CDK4/6i treatment in muring breast cancer models and in patients with breast cancer using high dimensional flow cytometry and RNA sequencing. Gain and loss of function in vivo experiments employing cell transfer and depletion antibody were performed to uncover immune cell populations critical for CDK4/6i-mediated stimulation of antitumor immunity. We found that loss of dendritic cells (DCs) within the tumor microenvironment resulting from CDK4/6 inhibition in bone marrow progenitors is a major factor limiting antitumor immunity after CDK4/6i and ICB. Consequently, restoration of DC compartment by adoptively transferring ex vivo differentiated DCs to mice treated with CDK4/6i and ICB therapy enabled robust tumor inhibition. Mechanistically, the addition of DCs promoted the induction of tumor-localized and systemic CD4 T-cell responses in mice receiving CDK4/6i-ICB-DC combination therapy, as characterized by enrichment of programmed cell death protein-1-negative T helper (Th)1 and Th2 cells with an activated phenotype. CD4 T-cell depletion abrogated the antitumor benefit of CDK4/6i-ICB-DC combination, with outgrowing tumors displaying an increased proportion of terminally exhausted CD8 T cells. Our findings suggest that CDK4/6i-mediated DC suppression limits CD4 T-cell responses essential for the sustained activity of CD8 T cells and tumor inhibition. Furthermore, they imply that restoring DC-CD4 T-cell crosstalk via DC transfer enables effective breast cancer immunity in response to CDK4/6i and ICB treatment. © Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Mus musculus (House mouse),
- Biochemistry and Molecular biology,
- Cancer Research,
- Immunology and Microbiology
Mechanism of inert inflammation in an immune checkpoint blockade-resistant tumor subtype bearing transcription elongation defects.
In Cell Reports on 25 April 2023 by Modur, V., Muhammad, B., et al.
PubMed
The clinical response to immune checkpoint blockade (ICB) correlates with tumor-infiltrating cytolytic T lymphocytes (CTLs) prior to treatment. However, many of these inflamed tumors resist ICB through unknown mechanisms. We show that tumors with transcription elongation deficiencies (TEdef+), which we previously reported as being resistant to ICB in mouse models and the clinic, have high baseline CTLs. We show that high baseline CTLs in TEdef+ tumors result from aberrant activation of the nucleic acid sensing-TBK1-CCL5/CXCL9 signaling cascade, which results in an immunosuppressive microenvironment with elevated regulatory T cells and exhausted CTLs. ICB therapy of TEdef+ tumors fail to increase CTL infiltration and suppress tumor growth in both experimental and clinical settings, suggesting that TEdef+, along with surrogate markers of tumor immunogenicity such as tumor mutational burden and CTLs, should be considered in the decision process for patient immunotherapy indication. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cancer Research
Neutrophil Conversion to a Tumor-Killing Phenotype Underpins Effective Microbial Therapy.
In Cancer Research on 14 April 2023 by Yam, A. O., Bailey, J., et al.
PubMed
The inflammatory microenvironment of solid tumors creates a protumorigenic milieu that resembles chronic inflammation akin to a subverted wound healing response. Here, we investigated the effect of converting the tumor microenvironment from a chronically inflamed state to one of acute microbial inflammation by injecting microbial bioparticles directly into tumors. Intratumoral microbial bioparticle injection led to rapid and dramatic changes in the tumor immune composition, the most striking of which was a substantial increase in the presence of activated neutrophils. In situ photoconversion and intravital microscopy indicated that tumor neutrophils transiently switched from sessile producers of VEGF to highly motile neutrophils that clustered to make neutrophil-rich domains in the tumor. The neutrophil clusters remodeled tumor tissue and repressed tumor growth. Single-cell transcriptional analysis of microbe-stimulated neutrophils showed a profound shift in gene expression towards heightened activation and antimicrobial effector function. Microbe-activated neutrophils also upregulated chemokines known to regulate neutrophil and CD8+ T-cell recruitment. Microbial therapy also boosted CD8+ T-cell function and enhanced the therapeutic benefit of checkpoint inhibitor therapy in tumor-bearing mice and provided protection in a model of tumor recurrence. These data indicate that one of the major effector mechanisms of microbial therapy is the conversion of tumor neutrophils from a wound healing to an acutely activated cytotoxic phenotype, highlighting a rationale for broader deployment of microbial therapy in the treatment of solid cancers. Intratumoral injection of microbial bioparticles stimulates neutrophil antitumor functions, suggesting pathways for optimizing efficacy of microbial therapies and paving the way for their broader utilization in the clinic. ©2023 The Authors; Published by the American Association for Cancer Research.
- Cancer Research,
- Immunology and Microbiology,
- Neuroscience
Anti-tumor memory CD4 and CD8 T-cells quantified by bulk T-cell receptor (TCR) clonal analysis.
In Frontiers in Immunology on 11 April 2023 by Gao, Y. & Bergman, I.
PubMed
Simple, reliable methods to detect anti-tumor memory T-cells are necessary to develop a clinical tumor vaccination program. A mouse model of curative viral onco-immunotherapy found that peritoneal tumor challenge following cure identified an oligoclonal anti-tumor memory CD4 and CD8 T-cell response. Clonotypes differed among the challenged animals but were congruent in blood, spleen and peritoneal cells (PC) of the same animal. Adoptive transfer demonstrated that the high-frequency responding T-cells were tumor specific. Tetramer analysis confirmed that clonotype frequency determined by T-cell receptor (TCR)- chain (TRB) analysis closely approximated cell clone frequency. The mean frequency of resting anti-tumor memory CD4 T-cells in unchallenged spleen was 0.028% and of memory CD8 T-cells was 0.11% which was not high enough to distinguish them from background. Stimulation produced a mean ~10-fold increase in splenic and 100-fold increase in peritoneal anti-tumor memory T-cell clonotypes. This methodology can be developed to use blood and tissue sampling to rapidly quantify the effectiveness of a tumor vaccine or any vaccine generating therapeutic T-cells. Copyright © 2023 Gao and Bergman.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Antigen-presenting type-I conventional dendritic cells facilitate curative checkpoint blockade immunotherapy in pancreatic cancer
Preprint on BioRxiv : the Preprint Server for Biology on 6 March 2023 by Mahadevan, K. K., Dyevoich, A. M., et al.
PubMed
Inflammation and tissue damage associated with pancreatitis can precede or occur concurrently with pancreatic ductal adenocarcinoma (PDAC). We demonstrate that in PDAC coupled with pancreatitis (ptPDAC), antigen-presenting type-I conventional dendritic cells (cDC1s) are specifically activated. Immune checkpoint blockade therapy (iCBT) leads to cytotoxic CD8 + T cell activation and eradication of ptPDAC with restoration of lifespan even upon PDAC re-challenge. Such eradication of ptPDAC was reversed following specific depletion of dendritic cells. Employing PDAC antigen-loaded cDC1s as a vaccine, immunotherapy-resistant PDAC was rendered sensitive to iCBT with a curative outcome. Analysis of the T-cell receptor (TCR) sequences in the tumor infiltrating CD8 + T cells following cDC1 vaccination coupled with iCBT identified unique CDR3 sequences with potential therapeutic significance. Our findings identify a fundamental difference in the immune microenvironment and adaptive immune response in PDAC concurrent with, or without pancreatitis, and provides a rationale for combining cDC1 vaccination with iCBT as a potential treatment option.
- Cancer Research,
- Immunology and Microbiology
Tumor-Suppressive and Immune-Stimulating Roles of Cholesterol 25-hydroxylase in Pancreatic Cancer Cells.
In Molecular Cancer Research on 1 March 2023 by McBrearty, N., Cho, C., et al.
PubMed
Cholesterol dependence is an essential characteristic of pancreatic ductal adenocarcinoma (PDAC). Cholesterol 25-hydroxylase (CH25H) catalyzes monooxygenation of cholesterol into 25-hydroxycholesterol, which is implicated in inhibiting cholesterol biosynthesis and in cholesterol depletion. Here, we show that, within PDAC cells, accumulation of cholesterol was facilitated by the loss of CH25H. Methylation of the CH25H gene and decreased levels of CH25H expression occurred in human pancreatic cancers and was associated with poor prognosis. Knockout of Ch25h in mice accelerated progression of Kras-driven pancreatic intraepithelial neoplasia. Conversely, restoration of CH25H expression in human and mouse PDAC cells decreased their viability under conditions of cholesterol deficit, and decelerated tumor growth in immune competent hosts. Mechanistically, the loss of CH25H promoted autophagy resulting in downregulation of MHC-I and decreased CD8+ T-cell tumor infiltration. Re-expression of CH25H in PDAC cells combined with immune checkpoint inhibitors notably inhibited tumor growth. We discuss additional benefits that PDAC cells might gain from inactivation of CH25H and the potential translational importance of these findings for therapeutic approaches to PDAC. Loss of CH25H by pancreatic cancer cells may stimulate tumor progression and interfere with immunotherapies. ©2022 American Association for Cancer Research.
- Cancer Research
Oncolytic BHV-1 Is Sufficient to Induce Immunogenic Cell Death and Synergizes with Low-Dose Chemotherapy to Dampen Immunosuppressive T Regulatory Cells.
In Cancers on 17 February 2023 by Dávola, M. E., Cormier, O., et al.
PubMed
Immunogenic cell death (ICD) can switch immunologically "cold" tumors "hot", making them sensitive to immune checkpoint inhibitor (ICI) therapy. Many therapeutic platforms combine multiple modalities such as oncolytic viruses (OVs) and low-dose chemotherapy to induce ICD and improve prognostic outcomes. We previously detailed many unique properties of oncolytic bovine herpesvirus type 1 (oBHV) that suggest widespread clinical utility. Here, we show for the first time, the ability of oBHV monotherapy to induce bona fide ICD and tumor-specific activation of circulating CD8+ T cells in a syngeneic murine model of melanoma. The addition of low-dose mitomycin C (MMC) was necessary to fully synergize with ICI through early recruitment of CD8+ T cells and reduced infiltration of highly suppressive PD-1+ Tregs. Cytokine and gene expression analyses within treated tumors suggest that the addition of MMC to oBHV therapy shifts the immune response from predominantly anti-viral, as evidenced by a high level of interferon-stimulated genes, to one that stimulates myeloid cells, antigen presentation and adaptive processes. Collectively, these data provide mechanistic insights into how oBHV-mediated therapy modalities overcome immune suppressive tumor microenvironments to enable the efficacy of ICI therapy.
- Immunology and Microbiology
Small-molecule toosendanin reverses macrophage-mediated immunosuppression to overcome glioblastoma resistance to immunotherapy.
In Science Translational Medicine on 15 February 2023 by Yang, F., Zhang, D., et al.
PubMed
T cell-based immunotherapy holds promise for treating solid tumors, but its therapeutic efficacy is limited by intratumoral immune suppression. This immune suppressive tumor microenvironment is largely driven by tumor-associated myeloid cells, including macrophages. Here, we report that toosendanin (TSN), a small-molecule compound, reprograms macrophages to enforce antitumor immunity in glioblastoma (GBM) in mouse models. Our functional screen of genetically probed macrophages with a chemical library identifies that TSN reverses macrophage-mediated tumor immunosuppression, leading to enhanced T cell infiltration, activation, and reduced exhaustion. Chemoproteomic and structural analyses revealed that TSN interacts with Hck and Lyn to abrogate suppressive macrophage immunity. In addition, a combination of immune checkpoint blockade and TSN therapy induced regression of syngeneic GBM tumors in mice. Furthermore, TSN treatment sensitized GBM to Egfrviii chimeric antigen receptor (CAR) T cell therapy. These findings suggest that TSN may serve as a therapeutic compound that blocks tumor immunosuppression and circumvents tumor resistance to T cell-based immunotherapy in GBM and other solid tumors that warrants further investigation.