InVivoMAb anti-mouse CD40L (CD154)
Product Details
The MR-1 monoclonal antibody reacts with mouse CD154 also known as CD40 ligand. CD154 exists as a 39 kDa accessory molecule and belongs to the TNF superfamily of cytokines. CD154 is primarily expressed on the surface of activated CD4+ T lymphocytes but can also be expressed by platelets, mast cells, macrophages, basophils, NK cells, B lymphocytes, CD8+ T lymphocytes as well as non-hematopoietic cells including smooth muscle cells, endothelial cells, and epithelial cells. CD154 signals through CD40 and is thought to play a key role in T and B lymphocyte costimulation. The MR-1 monoclonal antibody has been reported to inhibit in vitro activation of B lymphocytes by blocking the binding of CD154 with CD40 on T helper cells as well as inhibit the formation of germinal centers and disrupt antigen-specific T cell responses. Additionally, the MR-1 antibody blocks interactions of T cells and antigen-presenting cells in vitro and blocks the development of experimental autoimmune disease in vivo.Specifications
| Isotype | Armenian hamster IgG |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Activated mouse Th1 clone D1.6 |
| Reported Applications |
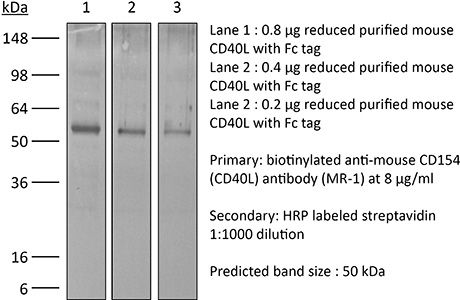
in vivo blocking of CD40/CD40L signaling in vitro blocking of CD40/CD40L signaling Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein A |
| RRID | AB_1107601 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo blocking of CD40/CD40L signaling
Pasqual, G., et al. (2018). "Monitoring T cell-dendritic cell interactions in vivo by intercellular enzymatic labelling" Nature 553(7689): 496-500. PubMed
Interactions between different cell types are essential for multiple biological processes, including immunity, embryonic development and neuronal signalling. Although the dynamics of cell-cell interactions can be monitored in vivo by intravital microscopy, this approach does not provide any information on the receptors and ligands involved or enable the isolation of interacting cells for downstream analysis. Here we describe a complementary approach that uses bacterial sortase A-mediated cell labelling across synapses of immune cells to identify receptor-ligand interactions between cells in living mice, by generating a signal that can subsequently be detected ex vivo by flow cytometry. We call this approach for the labelling of ‘kiss-and-run’ interactions between immune cells ‘Labelling Immune Partnerships by SorTagging Intercellular Contacts’ (LIPSTIC). Using LIPSTIC, we show that interactions between dendritic cells and CD4(+) T cells during T-cell priming in vivo occur in two distinct modalities: an early, cognate stage, during which CD40-CD40L interactions occur specifically between T cells and antigen-loaded dendritic cells; and a later, non-cognate stage during which these interactions no longer require prior engagement of the T-cell receptor. Therefore, LIPSTIC enables the direct measurement of dynamic cell-cell interactions both in vitro and in vivo. Given its flexibility for use with different receptor-ligand pairs and a range of detectable labels, we expect that this approach will be of use to any field of biology requiring quantification of intercellular communication.
in vivo blocking of CD40/CD40L signaling
Brasseit, J., et al. (2015). "CD4 T cells are required for both development and maintenance of disease in a new mouse model of reversible colitis" Mucosal Immunol. doi : 10.1038/mi.2015.93. PubMed
Current therapies to treat inflammatory bowel diseases have limited efficacy, significant side effects, and often wane over time. Little is known about the cellular and molecular mechanisms operative in the process of mucosal healing from colitis. To study such events, we developed a new model of reversible colitis in which adoptive transfer of CD4+CD45RBhi T cells into Helicobacter typhlonius-colonized lymphopenic mice resulted in a rapid onset of colonic inflammation that was reversible through depletion of colitogenic T cells. Remission was associated with an improved clinical and histopathological score, reduced immune cell infiltration to the intestinal mucosa, altered intestinal gene expression profiles, regeneration of the colonic mucus layer, and the restoration of epithelial barrier integrity. Notably, colitogenic T cells were not only critical for induction of colitis but also for maintenance of disease. Depletion of colitogenic T cells resulted in a rapid drop in tumor necrosis factor alpha (TNFalpha) levels associated with reduced infiltration of inflammatory immune cells to sites of inflammation. Although neutralization of TNFalpha prevented the onset of colitis, anti-TNFalpha treatment of mice with established disease failed to resolve colonic inflammation. Collectively, this new model of reversible colitis provides an important research tool to study the dynamics of mucosal healing in chronic intestinal remitting-relapsing disorders.
in vivo blocking of CD40/CD40L signaling
Conde, P., et al. (2015). "DC-SIGN(+) Macrophages Control the Induction of Transplantation Tolerance" Immunity 42(6): 1143-1158. PubMed
Tissue effector cells of the monocyte lineage can differentiate into different cell types with specific cell function depending on their environment. The phenotype, developmental requirements, and functional mechanisms of immune protective macrophages that mediate the induction of transplantation tolerance remain elusive. Here, we demonstrate that costimulatory blockade favored accumulation of DC-SIGN-expressing macrophages that inhibited CD8(+) T cell immunity and promoted CD4(+)Foxp3(+) Treg cell expansion in numbers. Mechanistically, that simultaneous DC-SIGN engagement by fucosylated ligands and TLR4 signaling was required for production of immunoregulatory IL-10 associated with prolonged allograft survival. Deletion of DC-SIGN-expressing macrophages in vivo, interfering with their CSF1-dependent development, or preventing the DC-SIGN signaling pathway abrogated tolerance. Together, the results provide new insights into the tolerogenic effects of costimulatory blockade and identify DC-SIGN(+) suppressive macrophages as crucial mediators of immunological tolerance with the concomitant therapeutic implications in the clinic.
in vivo blocking of CD40/CD40L signaling
Awe, O., et al. (2015). "PU.1 Expression in T Follicular Helper Cells Limits CD40L-Dependent Germinal Center B Cell Development" J Immunol . PubMed
PU.1 is an ETS family transcription factor that is important for the development of multiple hematopoietic cell lineages. Previous work demonstrated a critical role for PU.1 in promoting Th9 development and in limiting Th2 cytokine production. Whether PU.1 has functions in other Th lineages is not clear. In this study, we examined the effects of ectopic expression of PU.1 in CD4+ T cells and observed decreased expression of genes involved with the function of T follicular helper (Tfh) cells, including Il21 and Tnfsf5 (encoding CD40L). T cells from conditional mutant mice that lack expression of PU.1 in T cells (Sfpi1lck-/-) demonstrated increased production of CD40L and IL-21 in vitro. Following adjuvant-dependent or adjuvant-independent immunization, we observed that Sfpi1lck-/- mice had increased numbers of Tfh cells, increased germinal center B cells (GCB cells), and increased Ab production in vivo. This correlated with increased expression of IL-21 and CD40L in Tfh cells from Sfpi1lck-/- mice compared with control mice. Finally, although blockade of IL-21 did not affect GCB cells in Sfpi1lck-/- mice, anti-CD40L treatment of immunized Sfpi1lck-/- mice decreased GCB cell numbers and Ag-specific Ig concentrations. Together, these data indicate an inhibitory role for PU.1 in the function of Tfh cells, germinal centers, and Tfh-dependent humoral immunity.
in vivo blocking of CD40/CD40L signaling
Miller, M. L., et al. (2015). "Spontaneous restoration of transplantation tolerance after acute rejection" Nat Commun 6: 7566. PubMed
Transplantation is a cure for end-stage organ failure but, in the absence of pharmacological immunosuppression, allogeneic organs are acutely rejected. Such rejection invariably results in allosensitization and accelerated rejection of secondary donor-matched grafts. Transplantation tolerance can be induced in animals and a subset of humans, and enables long-term acceptance of allografts without maintenance immunosuppression. However, graft rejection can occur long after a state of transplantation tolerance has been acquired. When such an allograft is rejected, it has been assumed that the same rules of allosensitization apply as to non-tolerant hosts and that immunological tolerance is permanently lost. Using a mouse model of cardiac transplantation, we show that when Listeria monocytogenes infection precipitates acute rejection, thus abrogating transplantation tolerance, the donor-specific tolerant state re-emerges, allowing spontaneous acceptance of a donor-matched second transplant. These data demonstrate a setting in which the memory of allograft tolerance dominates over the memory of transplant rejection.
in vivo blocking of CD40/CD40L signaling, in vitro blocking of CD40/CD40L signaling
Krummey, S. M., et al. (2014). "Candida-elicited murine Th17 cells express high Ctla-4 compared with Th1 cells and are resistant to costimulation blockade" J Immunol 192(5): 2495-2504. PubMed
Effector and memory T cells may cross-react with allogeneic Ags to mediate graft rejection. Whereas the costimulation properties of Th1 cells are well studied, relatively little is known about the costimulation requirements of microbe-elicited Th17 cells. The costimulation blocker CTLA-4 Ig has been ineffective in the treatment of several Th17-driven autoimmune diseases and is associated with severe acute rejection following renal transplantation, leading us to investigate whether Th17 cells play a role in CD28/CTLA-4 blockade-resistant alloreactivity. We established an Ag-specific model in which Th1 and Th17 cells were elicited via Mycobacterium tuberculosis and Candida albicans immunization, respectively. C. albicans immunization elicited a higher frequency of Th17 cells and conferred resistance to costimulation blockade following transplantation. Compared with the M. tuberculosis group, C. albicans-elicited Th17 cells contained a higher frequency of IL-17(+)IFN-gamma(+) producers and a lower frequency of IL-10(+) and IL-10(+)IL-17(+) cells. Importantly, Th17 cells differentially regulated the CD28/CTLA-4 pathway, expressing similarly high CD28 but significantly greater amounts of CTLA-4 compared with Th1 cells. Ex vivo blockade experiments demonstrated that Th17 cells are more sensitive to CTLA-4 coinhibition and therefore less susceptible to CTLA-4 Ig. These novel insights into the differential regulation of CTLA-4 coinhibition on CD4(+) T cells have implications for the immunomodulation of pathologic T cell responses during transplantation and autoimmunity.
in vivo blocking of CD40/CD40L signaling
Marshall, D., et al. (2014). "Differential requirement for IL-2 and IL-15 during bifurcated development of thymic regulatory T cells" J Immunol 193(11): 5525-5533. PubMed
The developmental pathways of regulatory T cells (T(reg)) generation in the thymus are not fully understood. In this study, we reconstituted thymic development of Zap70-deficient thymocytes with a tetracycline-inducible Zap70 transgene to allow temporal dissection of T(reg) development. We find that T(reg) develop with distinctive kinetics, first appearing by day 4 among CD4 single-positive (SP) thymocytes. Accepted models of CD25(+)Foxp3(+) T(reg) selection suggest development via CD25(+)Foxp3(-) CD4 SP precursors. In contrast, our kinetic analysis revealed the presence of abundant CD25(-)Foxp3(+) cells that are highly efficient at maturing to CD25(+)Foxp3(+) cells in response to IL-2. CD25(-)Foxp3(+) cells more closely resembled mature T(reg) both with respect to kinetics of development and avidity for self-peptide MHC. These population also exhibited distinct requirements for cytokines during their development. CD25(-)Foxp3(+) cells were IL-15 dependent, whereas generation of CD25(+)Foxp3(+) specifically required IL-2. Finally, we found that IL-2 and IL-15 arose from distinct sources in vivo. IL-15 was of stromal origin, whereas IL-2 was of exclusively from hemopoetic cells that depended on intact CD4 lineage development but not either Ag-experienced or NKT cells.
in vivo blocking of CD40/CD40L signaling
Ballesteros-Tato, A., et al. (2014). "Epitope-specific regulation of memory programming by differential duration of antigen presentation to influenza-specific CD8(+) T cells" Immunity 41(1): 127-140. PubMed
Memory CD8(+) T cells are programmed during the primary response for robust secondary responsiveness. Here we show that CD8(+) T cells responding to different epitopes of influenza virus received qualitatively different signals during the primary response that altered their secondary responsiveness. Nucleoprotein (NP)-specific CD8(+) T cells encountered antigen on CD40-licensed, CD70-expressing, CD103(-)CD11b(hi) dendritic cells (DCs) at later times in the primary response. As a consequence, they maintained CD25 expression and responded to interleukin-2 (IL-2) and CD27, which together programmed their robust secondary proliferative capacity and interferon-gamma (IFN-gamma)-producing ability. In contrast, polymerase (PA)-specific CD8(+) T cells did not encounter antigen-bearing, CD40-activated DCs at later times in the primary response, did not receive CD27 and CD25 signals, and were not programmed to become memory CD8(+) T cells with strong proliferative and cytokine-producing ability. As a result, CD8(+) T cells responding to abundant antigens, like NP, dominated the secondary response.
in vivo blocking of CD40/CD40L signaling
Baumjohann, D., et al. (2013). "Persistent antigen and germinal center B cells sustain T follicular helper cell responses and phenotype" Immunity 38(3): 596-605. PubMed
T follicular helper (Tfh) cells provide help to B cells and are crucial for establishment of germinal center (GC) reactions, including production of high-affinity antibodies and generation of memory B cells and long-lived plasma cells. Here we report that the magnitude of the Tfh cell response was dictated by the amount of antigen and directly correlated with the magnitude of the GC B cell response. In addition, maintenance of the Tfh cell phenotype required sustained antigenic stimulation by GC B cells. In lymphopenic conditions, a strong and prolonged Tfh cell response led to bystander B cell activation, hypergammaglobulinemia, and production of poly- and self-reactive antibodies. These data demonstrate that antigen dose determines the size and duration of the Tfh cell response and GC reaction, highlight the transient nature of the Tfh cell phenotype, and suggest a link between overstimulation of Tfh cells and the development of dysregulated humoral immune responses.
in vivo blocking of CD40/CD40L signaling
Taylor, J. J., et al. (2012). "A germinal center-independent pathway generates unswitched memory B cells early in the primary response" J Exp Med 209(3): 597-606. PubMed
Memory B cells can be produced from the classical germinal center (GC) pathway or a less understood GC-independent route. We used antigen-based cell enrichment to assess the relative contributions of these pathways to the polyclonal memory B cell pool. We identified a CD38(+) GL7(+) B cell precursor population that differentiated directly into IgM(+) or isotype-switched (sw) Ig(+) memory B cells in a GC-independent fashion in response to strong CD40 stimulation. Alternatively, CD38(+) GL7(+) B cell precursors had the potential to become Bcl-6(+) GC cells that then generated primarily swIg(+) memory B cells. These results demonstrate that early IgM(+) and swIg(+) memory B cells are products of a GC-independent pathway, whereas later switched Ig(+) memory B cells are products of GC cells.
in vivo blocking of CD40/CD40L signaling
Hofstetter, A. R., et al. (2012). "MHC class Ib-restricted CD8 T cells differ in dependence on CD4 T cell help and CD28 costimulation over the course of mouse polyomavirus infection" J Immunol 188(7): 3071-3079. PubMed
We recently identified a protective MHC class Ib-restricted CD8 T cell response to infection with mouse polyomavirus. These CD8 T cells recognize a peptide from aa 139-147 of the VP2 viral capsid protein bound to the nonpolymorphic H-2Q9 molecule, a member of the Qa-2 family of beta(2)m-associated MHC class Ib molecules. Q9:VP2.139-specific CD8 T cells exhibit an unusual inflationary response characterized by a gradual expansion over 3 mo followed by a stable maintenance phase. We previously demonstrated that Q9:VP2.139-specific CD8 T cells are dependent on Ag for expansion, but not for long-term maintenance. In this study, we tested the hypothesis that the expansion and maintenance components of the Q9:VP2.139-specific T cell response are differentially dependent on CD4 T cell help and CD28 costimulation. Depletion of CD4(+) cells and CD28/CD40L blockade impaired expansion of Q9:VP2.139-specific CD8 T cells, and intrinsic CD28 signaling was sufficient for expansion. In contrast, CD4 T cell insufficiency, but not CD28/CD40L blockade, resulted in a decline in frequency of Q9:VP2.139-specific CD8 T cells during the maintenance phase. These results indicate that the Q9:VP2.139-specific CD8 T cell response to mouse polyomavirus infection depends on CD4 T cell help and CD28 costimulation for inflationary expansion, but only on CD4 T cell help for maintenance.
in vivo blocking of CD40/CD40L signaling
West, E. E., et al. (2011). "Tight regulation of memory CD8(+) T cells limits their effectiveness during sustained high viral load" Immunity 35(2): 285-298. PubMed
To design successful vaccines for chronic diseases, an understanding of memory CD8(+) T cell responses to persistent antigen restimulation is critical. However, most studies comparing memory and naive cell responses have been performed only in rapidly cleared acute infections. Herein, by comparing the responses of memory and naive CD8(+) T cells to acute and chronic lymphocytic choriomeningitis virus infection, we show that memory cells dominated over naive cells and were protective when present in sufficient numbers to quickly reduce infection. In contrast, when infection was not rapidly reduced, because of high antigen load or persistence, memory cells were quickly lost, unlike naive cells. This loss of memory cells was due to a block in sustaining cell proliferation, selective regulation by the inhibitory receptor 2B4, and increased reliance on CD4(+) T cell help. Thus, emphasizing the importance of designing vaccines that elicit effective CD4(+) T cell help and rapidly control infection.
- Mus musculus (House mouse),
- Neuroscience,
- Stem Cells and Developmental Biology
Human neural stem cells restore spatial memory in a transgenic Alzheimer's disease mouse model by an immunomodulating mechanism.
In Frontiers in Aging Neuroscience on 29 December 2023 by Chen, K. S., Noureldein, M. H., et al.
PubMed
Stem cells are a promising therapeutic in Alzheimer's disease (AD) given the complex pathophysiologic pathways involved. However, the therapeutic mechanisms of stem cells remain unclear. Here, we used spatial transcriptomics to elucidate therapeutic mechanisms of human neural stem cells (hNSCs) in an animal model of AD. hNSCs were transplanted into the fimbria fornix of the hippocampus using the 5XFAD mouse model. Spatial memory was assessed by Morris water maze. Amyloid plaque burden was quantified. Spatial transcriptomics was performed and differentially expressed genes (DEGs) identified both globally and within the hippocampus. Subsequent pathway enrichment and ligand-receptor network analysis was performed. hNSC transplantation restored learning curves of 5XFAD mice. However, there were no changes in amyloid plaque burden. Spatial transcriptomics showed 1,061 DEGs normalized in hippocampal subregions. Plaque induced genes in microglia, along with populations of stage 1 and stage 2 disease associated microglia (DAM), were normalized upon hNSC transplantation. Pathologic signaling between hippocampus and DAM was also restored. hNSCs normalized many dysregulated genes, although this was not mediated by a change in amyloid plaque levels. Rather, hNSCs appear to exert beneficial effects in part by modulating microglia-mediated neuroinflammation and signaling in AD. Copyright © 2023 Chen, Noureldein, McGinley, Hayes, Rigan, Kwentus, Mason, Mendelson, Savelieff and Feldman.
- Mus musculus (House mouse),
- Neuroscience,
- Stem Cells and Developmental Biology
Human neural stem cells restore spatial memory in a transgenic Alzheimer’s disease mouse model by an immunomodulating mechanism
Preprint on BioRxiv : the Preprint Server for Biology on 4 November 2023 by Chen, K. S., Noureldein, M. H., et al.
PubMed
ABSTRACT INTRODUCTION Stem cells are a promising therapeutic in Alzheimer’s disease (AD) given the complex pathophysiologic pathways involved. However, the therapeutic mechanisms of stem cells remain unclear. Here, we used spatial transcriptomics to elucidate therapeutic mechanisms of human neural stem cells (hNSCs) in an animal model of AD. METHODS hNSCs were transplanted into the fimbria fornix of the hippocampus using the 5XFAD mouse model. Spatial memory was assessed by Morris water maze. Amyloid plaque burden was quantified. Spatial transcriptomics was performed and differentially expressed genes (DEGs) identified both globally and within the hippocampus. Subsequent pathway enrichment and ligand-receptor network analysis was performed. RESULTS hNSC transplantation restored learning curves of 5XFAD mice. However, there were no changes in amyloid plaque burden. Spatial transcriptomics showed 1061 DEGs normalized in hippocampal subregions. Plaque induced genes in microglia, along with populations of stage 1 and stage 2 disease associated microglia (DAM), were normalized upon hNSC transplantation. Pathologic signaling between hippocampus and DAM was also restored. DISCUSSION hNSCs normalized many dysregulated genes, although this was not mediated by a change in amyloid plaque levels. Rather, hNSCs appear to exert beneficial effects in part by modulating microglia-mediated neuroinflammation and signaling in AD.
- Cancer Research,
- Immunology and Microbiology,
- Neuroscience,
- Stem Cells and Developmental Biology
Neoantigen-specific stem cell memory-like CD4+ T cells mediate CD8+ T cell-dependent immunotherapy of MHC class II-negative solid tumors.
In Nature Immunology on 1 August 2023 by Brightman, S. E., Becker, A., et al.
PubMed
CD4+ T cells play key roles in a range of immune responses, either as direct effectors or through accessory cells, including CD8+ T lymphocytes. In cancer, neoantigen (NeoAg)-specific CD8+ T cells capable of direct tumor recognition have been extensively studied, whereas the role of NeoAg-specific CD4+ T cells is less well understood. We have characterized the murine CD4+ T cell response against a validated NeoAg (CLTCH129>Q) expressed by the MHC-II-deficient squamous cell carcinoma tumor model (SCC VII) at the level of single T cell receptor (TCR) clonotypes and in the setting of adoptive immunotherapy. We find that the natural CLTCH129>Q-specific repertoire is diverse and contains TCRs with distinct avidities as measured by tetramer-binding assays and CD4 dependence. Despite these differences, CD4+ T cells expressing high or moderate avidity TCRs undergo comparable in vivo proliferation to cross-presented antigen from growing tumors and drive similar levels of therapeutic immunity that is dependent on CD8+ T cells and CD40L signaling. Adoptive cellular therapy (ACT) with NeoAg-specific CD4+ T cells is most effective when TCR-engineered cells are differentiated ex vivo with IL-7 and IL-15 rather than IL-2 and this was associated with both increased expansion as well as the acquisition and stable maintenance of a T stem cell memory (TSCM)-like phenotype in tumor-draining lymph nodes (tdLNs). ACT with TSCM-like CD4+ T cells results in lower PD-1 expression by CD8+ T cells in the tumor microenvironment and an increased frequency of PD-1+CD8+ T cells in tdLNs. These findings illuminate the role of NeoAg-specific CD4+ T cells in mediating antitumor immunity via providing help to CD8+ T cells and highlight their therapeutic potential in ACT. © 2023. The Author(s).
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Tumor-specific CD4 T cells instruct monocyte fate in pancreatic ductal adenocarcinoma.
In Cell Reports on 25 July 2023 by Patterson, M. T., Burrack, A. L., et al.
PubMed
Pancreatic ductal adenocarcinoma (PDA) orchestrates a suppressive tumor microenvironment that fosters immunotherapy resistance. Tumor-associated macrophages (TAMs) are the principal immune cell infiltrating PDA and are heterogeneous. Here, by employing macrophage fate-mapping approaches and single-cell RNA sequencing, we show that monocytes give rise to most macrophage subsets in PDA. Tumor-specific CD4, but not CD8, T cells promote monocyte differentiation into MHCIIhi anti-tumor macrophages. By conditional major histocompatibility complex (MHC) class II deletion on monocyte-derived macrophages, we show that tumor antigen presentation is required for instructing monocyte differentiation into anti-tumor macrophages, promoting Th1 cells, abrogating Treg cells, and mitigating CD8 T cell exhaustion. Non-redundant IFNγ and CD40 promote MHCIIhi anti-tumor macrophages. Intratumoral monocytes adopt a pro-tumor fate indistinguishable from that of tissue-resident macrophages following loss of macrophage MHC class II or tumor-specific CD4 T cells. Thus, tumor antigen presentation by macrophages to CD4 T cells dictates TAM fate and is a major determinant of macrophage heterogeneity in cancer. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
The Ubiquitin Ligase Itch Skews Light Zone Selection in Germinal Centers.
In The Journal of Immunology on 15 May 2023 by Renshaw, L., Kim, P., et al.
PubMed
Ig diversification occurs in peripheral lymphoid organs after establishment of central tolerance during B cell development. In germinal centers (GCs), somatic hypermutation of Ig genes occurs in dark zones, followed by selection of mutated clones in light zones (LZs). This generates high-affinity Ig receptors to pathogens but can also produce autoreactive Ig receptors, which are removed by selection mechanisms that are incompletely understood. The ubiquitin ligase Itch prevents the emergence of autoimmune disease and autoantibodies in humans and mice, and patients lacking Itch develop potentially fatal autoimmune diseases; yet, how Itch regulates GC B cells is not well understood. By studying Itch-deficient mice, we have recently shown that Itch directly limits the magnitude of GC responses. Proteomic profiling of GC B cells uncovered that Itch-deficient cells exhibit high mTORC1 and Myc activity, hallmarks of positive selection. Bone marrow chimera and adoptive transfer experiments revealed that B cell Itch restricts noncycling LZ cells. These results support, to our knowledge, a novel role for Itch in skewing selection of GC B cells to restrict LZ accumulation and shape GC-derived humoral immunity. Determining how B cells integrate cues within GCs to navigate through LZs and dark zones will aid in understanding how autoreactive clones emerge from GCs in people with autoimmune disease. Copyright © 2023 by The American Association of Immunologists, Inc.
- Genetics,
- Immunology and Microbiology
Immune profiling of adeno-associated virus response identifies B cell-specific targets that enable vector re-administration in mice.
In Gene Therapy on 1 May 2023 by Chen, M., Kim, B., et al.
PubMed
Adeno-associated virus (AAV) vector-based gene therapies can be applied to a wide range of diseases. AAV expression can last for months to years, but vector re-administration may be necessary to achieve life-long treatment. Unfortunately, immune responses against these vectors are potentiated after the first administration, preventing the clinical use of repeated administration of AAVs. Reducing the immune response against AAVs while minimizing broad immunosuppression would improve gene delivery efficiency and long-term safety. In this study, we quantified the contributions of multiple immune system components of the anti-AAV response in mice. We identified B-cell-mediated immunity as a critical component preventing vector re-administration. Additionally, we found that IgG depletion alone was insufficient to enable re-administration, suggesting IgM antibodies play an important role in the immune response against AAV. Further, we found that AAV-mediated transduction is improved in µMT mice that lack functional IgM heavy chains and cannot form mature B-cells relative to wild-type mice. Combined, our results suggest that B-cells, including non-class switched B-cells, are a potential target for therapeutics enabling AAV re-administration. Our results also suggest that the µMT mice are a potentially useful experimental model for gene delivery studies since they allow repeated dosing for more efficient gene delivery from AAVs. © 2022. The Author(s), under exclusive licence to Springer Nature Limited.
- FC/FACS,
- Mus musculus (House mouse),
- Immunology and Microbiology
Expansion of circulating stem-like CD8+ T cells by adding CD122-directed IL-2 complexes to radiation and anti-PD1 therapies in mice.
In Nature Communications on 12 April 2023 by Onyshchenko, K., Luo, R., et al.
PubMed
Combination of radiation therapy (RT) with immune checkpoint blockade can enhance systemic anti-tumor T cell responses. Here, using two mouse tumor models, we demonstrate that adding long-acting CD122-directed IL-2 complexes (IL-2c) to RT/anti-PD1 further increases tumor-specific CD8+ T cell numbers. The highest increase (>50-fold) is found in the blood circulation. Compartmental analysis of exhausted T cell subsets shows that primarily undifferentiated, stem-like, tumor-specific CD8+ T cells expand in the blood; these cells express the chemokine receptor CXCR3, which is required for migration into tumors. In tumor tissue, effector-like but not terminally differentiated exhausted CD8+ T cells increase. Consistent with the surge in tumor-specific CD8+ T cells in blood that are migration and proliferation competent, we observe a CD8-dependent and CXCR3-dependent enhancement of the abscopal effect against distant/non-irradiated tumors and find that CD8+ T cells isolated from blood after RT/anti-PD1/IL-2c triple treatment can be a rich source of tumor-specific T cells for adoptive transfers. © 2023. The Author(s).
- Mus musculus (House mouse)
Thymus antibody-secreting cells possess an interferon gene signature and are preferentially expanded in young female mice.
In IScience on 17 March 2023 by Pioli, K. T., Lau, K. H., et al.
PubMed
Antibody-secreting cells (ASCs) are key contributors to humoral immunity through immunoglobulin production and the potential to be long-lived. ASC persistence has been recognized in the autoimmune thymus (THY); however, only recently has this population been appreciated in healthy THY tissue. We showed that the young female THY was skewed toward higher production of ASCs relative to males. However, these differences disappeared with age. In both sexes, THY ASCs included Ki-67+ plasmablasts which required CD154(CD40L) signals for their propagation. Single cell RNA-sequencing revealed that THY ASCs were enriched for an interferon responsive transcriptional signature relative to those from bone marrow and spleen. Flow cytometry confirmed that THY ASCs had increased levels of Toll-like receptor 7 as well as CD69 and major histocompatibility complex class II. Overall, we identified fundamental aspects of THY ASC biology which may be leveraged for future in depth studies of this population in both health and disease. © 2023 The Author(s).
- Mus musculus (House mouse)
Progressive differentiation toward the long-lived plasma cell compartment in the bone marrow.
In The Journal of Experimental Medicine on 6 February 2023 by Koike, T., Fujii, K., et al.
PubMed
The longevity of plasma cells is dependent on their ability to access and reside in so-called niches that are predominantly located in the bone marrow. Here, by employing a traceable method to label recently generated plasma cells, we showed that homeostatic plasma cells in the bone marrow and spleen were continuously replenished by newly generated B220hiMHC-IIhi populations that progressively differentiated into B220loMHC-IIlo long-lived plasma cell (LLPC) populations. We also found that, in the bone marrow, germinal center (GC)-independent and GC-dependent plasma cells decayed similarly upon NP-CGG engagement, and both entered the B220loMHC-IIlo LLPC pool. Compared with NP+B220hiMHC-IIhi plasma cells, NP+B220loMHC-IIlo cells were more immobilized in the bone marrow niches and showed better survival potential. Thus, our results suggest that the adhesion status of bone marrow plasma cells is dynamically altered during their differentiation and is associated with provision of survival signals. © 2022 Koike et al.
- Mus musculus (House mouse),
- Immunology and Microbiology
Mucosal plasma cells are required to protect the upper airway and brain from infection.
In Immunity on 8 November 2022 by Wellford, S. A., Moseman, A. P., et al.
PubMed
While blood antibodies mediate protective immunity in most organs, whether they protect nasal surfaces in the upper airway is unclear. Using multiple viral infection models in mice, we found that blood-borne antibodies could not defend the olfactory epithelium. Despite high serum antibody titers, pathogens infected nasal turbinates, and neurotropic microbes invaded the brain. Using passive antibody transfers and parabiosis, we identified a restrictive blood-endothelial barrier that excluded circulating antibodies from the olfactory mucosa. Plasma cell depletions demonstrated that plasma cells must reside within olfactory tissue to achieve sterilizing immunity. Antibody blockade and genetically deficient models revealed that this local immunity required CD4+ T cells and CXCR3. Many vaccine adjuvants failed to generate olfactory plasma cells, but mucosal immunizations established humoral protection of the olfactory surface. Our identification of a blood-olfactory barrier and the requirement for tissue-derived antibody has implications for vaccinology, respiratory and CNS pathogen transmission, and B cell fate decisions. Copyright © 2022 Elsevier Inc. All rights reserved.
- Cancer Research
Platelets control liver tumor growth through P2Y12-dependent CD40L release in NAFLD.
In Cancer Cell on 12 September 2022 by Ma, C., Fu, Q., et al.
PubMed
Platelets, the often-overlooked component of the immune system, have been shown to promote tumor growth. Non-alcoholic fatty liver disease (NAFLD) is a common disease in the Western world and rising risk for hepatocellular carcinoma (HCC). Unexpectedly, we observed that platelets can inhibit the growth of established HCC in NAFLD mice. Through pharmacological inhibition and genetic depletion of P2Y12 as well as in vivo transfusion of wild-type (WT) or CD40L-/- platelets, we demonstrate that the anti-tumor function of platelets is mediated through P2Y12-dependent CD40L release, which leads to CD8+ T cell activation by the CD40 receptor. Unlike P2Y12 inhibition, blocking platelets with aspirin does not prevent platelet CD40L release nor accelerate HCC in NAFLD mice. Similar findings were observed in liver metastasis models. All together, our study reveals a complex role of platelets in tumor regulation. Anti-platelet treatment without inhibiting CD40L release could be considered for liver cancer patients with NAFLD. Published by Elsevier Inc.
- Cardiovascular biology
Low-dose IL-2 prevents murine chronic cardiac allograft rejection: Role for IL-2-induced T regulatory cells and exosomes with PD-L1 and CD73.
In American Journal of Transplantation : Official Journal of the American Society of Transplantation and the American Society of Transplant Surgeons on 1 September 2022 by Ravichandran, R., Itabashi, Y., et al.
PubMed
To determine the effects and immunological mechanisms of low-dose interleukin-2 (IL-2) in a murine model of chronic cardiac allograft rejection (BALB/c to C57BL/6) after costimulatory blockade consisting of MR1 (250 μg/ip day 0) and CTLA4-Ig (200 μg/ip day 2), we administered low-dose IL-2 (2000 IU/day) starting on posttransplant day 14 for 3 weeks. T regulatory (Treg) cell infiltration of the grafts was determined by immunohistochemistry; circulating exosomes by western blot and aldehyde bead flow cytometry; antibodies to donor MHC by immunofluorescent staining of donor cells; and antibodies to cardiac self-antigens (myosin, vimentin) by ELISA. We demonstrated that costimulation blockade after allogeneic heart transplantation induced circulating exosomes containing cardiac self-antigens and antibodies to both donor MHC and self-antigens, leading to chronic rejection by day 45. Treatment with low-dose IL-2 prolonged allograft survival (>100 days), prevented chronic rejection, and induced splenic and graft-infiltrating CD4+ CD25+ Foxp3 Treg cells by day 45 and circulating exosomes (Foxp3+) with PD-L1 and CD73. MicroRNA 142, associated with the TGFβ pathway, was significantly downregulated in exosomes from IL-2-treated mice. In conclusion, low-dose IL-2 delays rejection in a murine model of chronic cardiac allograft rejection and also induces graft-infiltrating Tregs and circulating exosomes with immunoregulatory molecules. © 2022 The American Society of Transplantation and the American Society of Transplant Surgeons.
- Immunology and Microbiology,
- Neuroscience,
- In Vivo,
- Mus musculus (House mouse)
Viral infection engenders bona fide and bystander subsets of lung-resident memory B cells through a permissive mechanism.
In Immunity on 12 July 2022 by Grégoire, C., Spinelli, L., et al.
PubMed
Lung-resident memory B cells (MBCs) provide localized protection against reinfection in respiratory airways. Currently, the biology of these cells remains largely unexplored. Here, we combined influenza and SARS-CoV-2 infection with fluorescent-reporter mice to identify MBCs regardless of antigen specificity. We found that two main transcriptionally distinct subsets of MBCs colonized the lung peribronchial niche after infection. These subsets arose from different progenitors and were both class switched, somatically mutated, and intrinsically biased in their differentiation fate toward plasma cells. Combined analysis of antigen specificity and B cell receptor repertoire segregated these subsets into "bona fide" virus-specific MBCs and "bystander" MBCs with no apparent specificity for eliciting viruses generated through an alternative permissive process. Thus, diverse transcriptional programs in MBCs are not linked to specific effector fates but rather to divergent strategies of the immune system to simultaneously provide rapid protection from reinfection while diversifying the initial B cell repertoire. Copyright © 2022 Elsevier Inc. All rights reserved.
- Mus musculus (House mouse)
Germinal center expansion but not plasmablast differentiation is proportional to peptide-MHCII density via CD40-CD40L signaling strength.
In Cell Reports on 3 May 2022 by Jing, Z., McCarron, M. J., et al.
PubMed
T follicular helper (TFH) cells promote expansion of germinal center (GC) B cells and plasma cell differentiation. Whether cognate peptide-MHCII (pMHCII) density instructs selection and cell fate decisions in a quantitative manner remains unclear. Using αDEC205-OVA to differentially deliver OVA peptides to GC B cells on the basis of DEC205 allelic copy number, we find DEC205+/+ B cells take up 2-fold more antigen than DEC205+/- cells, leading to proportional TFH cell help and B cell expansion. To validate these results, we establish a caged OVA peptide, which is readily detected by OVA-specific TFH cells after photo-uncaging. In situ uncaging of peptides leads to multiple serial B-T contacts and cell activation. Differential CD40 signaling, is both necessary and sufficient to mediate 2-fold differences in B cell expansion. While plasmablast numbers are increased, pMHCII density does not directly control the output or quality of plasma cells. Thus, we distinguish the roles TFH cells play in expansion versus differentiation. Copyright © 2022 The Author(s). Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Neuroscience
Secondary influenza challenge triggers resident memory B cell migration and rapid relocation to boost antibody secretion at infected sites.
In Immunity on 12 April 2022 by MacLean, A. J., Richmond, N., et al.
PubMed
Resident memory B (BRM) cells develop and persist in the lungs of influenza-infected mice and humans; however, their contribution to recall responses has not been defined. Here, we used two-photon microscopy to visualize BRM cells within the lungs of influenza -virus immune and reinfected mice. Prior to re-exposure, BRM cells were sparsely scattered throughout the tissue, displaying limited motility. Within 24 h of rechallenge, these cells increased their migratory capacity, localized to infected sites, and subsequently differentiated into plasma cells. Alveolar macrophages mediated this process, in part by inducing expression of chemokines CXCL9 and CXCL10 from infiltrating inflammatory cells. This led to the recruitment of chemokine receptor CXCR3-expressing BRM cells to infected regions and increased local antibody concentrations. Our study uncovers spatiotemporal mechanisms that regulate lung BRM cell reactivation and demonstrates their capacity to rapidly deliver antibodies in a highly localized manner to sites of viral replication.Copyright © 2022 The Author(s). Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology
Tfh-cell-derived interleukin 21 sustains effector CD8+ T cell responses during chronic viral infection.
In Immunity on 8 March 2022 by Zander, R., Kasmani, M. Y., et al.
PubMed
CD4+ T cell-derived interleukin 21 (IL-21) sustains CD8+ T cell responses during chronic viral infection, but the helper subset that confers this protection remains unclear. Here, we applied scRNA and ATAC-seq approaches to determine the heterogeneity of IL-21+CD4+ T cells during LCMV clone 13 infection. CD4+ T cells were comprised of three transcriptionally and epigenetically distinct populations: Cxcr6+ Th1 cells, Cxcr5+ Tfh cells, and a previously unrecognized Slamf6+ memory-like (Tml) subset. T cell differentiation was specifically redirected toward the Tml subset during chronic, but not acute, LCMV infection. Although this subset displayed an enhanced capacity to accumulate and some developmental plasticity, it remained largely quiescent, which may hinder its helper potential. Conversely, mixed bone marrow chimera experiments revealed that Tfh cell-derived IL-21 was critical to sustain CD8+ T cell responses and viral control. Thus, strategies that bolster IL-21+Tfh cell responses may prove effective in enhancing CD8+ T cell-mediated immunity. Copyright © 2022 Elsevier Inc. All rights reserved.
Targeted immunosuppression enhances repeated gene delivery
Preprint on Research Square on 1 March 2022 by Chen, M., Kim, B., et al.
PubMed
Adeno-associated virus (AAV) vector-based gene therapies can be applied to a wide range of diseases. AAV expression can last for months to years, but vector re-administration may be necessary to achieve life-long treatment. Unfortunately, immune system response against these vectors is potentiated after the first administration, which prevents the clinical use of repeated administration of AAVs. Reducing immune response against AAVs while minimizing immunosuppression would improve gene delivery efficiency and long-term safety. In this study, we quantified the contributions of multiple immune system components towards AAV response in mice. We identified B-cell-mediated immunity as a critical component preventing vector re-administration. Specifically, we found that IgG depletion was insufficient to enhance re-administration, suggesting the key role of B-cell mediated IgM antibodies in the immune response against AAV. Further, we also found that AAV-mediated transduction is improved compared to wild-type mice in µMT mice that lack functional IgM heavy chains and cannot form mature B-cells. Combined, our results suggest that IgM production in B cells is a potential target for therapeutics enabling AAV re-administration. Our results also suggest that the µMT mice are a potentially useful experimental model for gene delivery studies since they allow for up to 15-fold more efficient gene delivery.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
B cells imprint adoptively transferred CD8+ T cells with enhanced tumor immunity.
In Journal for Immunotherapy of Cancer on 1 January 2022 by Smith, A. S., Knochelmann, H. M., et al.
PubMed
Adoptive T cell transfer (ACT) therapy improves outcomes in patients with advanced malignancies, yet many individuals relapse due to the infusion of T cells with poor function or persistence. Toll-like receptor (TLR) agonists can invigorate antitumor T cell responses when administered directly to patients, but these responses often coincide with toxicities. We posited that TLR agonists could be repurposed ex vivo to condition T cells with remarkable potency in vivo, circumventing TLR-related toxicity. In this study we investigated how tumor-specific murine CD8+ T cells and human tumor infiltrating lymphocytes (TILs) are impacted when expanded ex vivo with the TLR9 agonist CpG. Herein we reveal a new way to reverse the tolerant state of adoptively transferred CD8+ T cells against tumors using TLR-activated B cells. We repurposed the TLR9 agonist, CpG, commonly used in the clinic, to bolster T cell-B cell interactions during expansion for ACT. T cells expanded ex vivo from a CpG-treated culture demonstrated potent antitumor efficacy and prolonged persistence in vivo. This antitumor efficacy was accomplished without in vivo administration of TLR agonists or other adjuvants of high-dose interleukin (IL)-2 or vaccination, which are classically required for effective ACT therapy. CpG-conditioned CD8+ T cells acquired a unique proteomic signature hallmarked by an IL-2RαhighICOShighCD39low phenotype and an altered metabolic profile, all reliant on B cells transiently present in the culture. Likewise, human TILs benefitted from expansion with CpG ex vivo, as they also possessed the IL-2RαhighICOShighCD39low phenotype. CpG fostered the expansion of potent CD8+ T cells with the signature phenotype and antitumor ability via empowering a direct B-T cell interaction. Isolated B cells also imparted T cells with the CpG-associated phenotype and improved tumor immunity without the aid of additional antigen-presenting cells or other immune cells in the culture. Our results demonstrate a novel way to use TLR agonists to improve immunotherapy and reveal a vital role for B cells in the generation of potent CD8+ T cell-based therapies. Our findings have immediate implications in the clinical treatment of advanced solid tumors. © Author(s) (or their employer(s)) 2022. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Immunology and Microbiology
Antigen presentation by lung epithelial cells directs CD4+ TRM cell function and regulates barrier immunity.
In Nature Communications on 5 October 2021 by Shenoy, A. T., Lyon de Ana, C., et al.
PubMed
Barrier tissues are populated by functionally plastic CD4+ resident memory T (TRM) cells. Whether the barrier epithelium regulates CD4+ TRM cell locations, plasticity and activities remains unclear. Here we report that lung epithelial cells, including distinct surfactant protein C (SPC)lowMHChigh epithelial cells, function as anatomically-segregated and temporally-dynamic antigen presenting cells. In vivo ablation of lung epithelial MHC-II results in altered localization of CD4+ TRM cells. Recurrent encounters with cognate antigen in the absence of epithelial MHC-II leads CD4+ TRM cells to co-express several classically antagonistic lineage-defining transcription factors, changes their cytokine profiles, and results in dysregulated barrier immunity. In addition, lung epithelial MHC-II is needed for surface expression of PD-L1, which engages its ligand PD-1 to constrain lung CD4+ TRM cell phenotypes. Thus, we establish epithelial antigen presentation as a critical regulator of CD4+ TRM cell function and identify epithelial-CD4+ TRM cell immune interactions as core elements of barrier immunity. © 2021. The Author(s).
- Immunology and Microbiology,
- Neuroscience
Germinal center-dependent and -independent memory B cells produced throughout the immune response.
In The Journal of Experimental Medicine on 2 August 2021 by Viant, C., Wirthmiller, T., et al.
PubMed
Memory B cells comprise a heterogenous group of cells that differ in origin and phenotype. During the early phases of the immune response, activated B cells can differentiate into IgM-expressing memory cells, short-lived plasma cells, or seed germinal centers (GCs). The memory compartment is subsequently enriched by B cells that have been through several rounds of division and selection in the GC. Here, we report on the use of an unbiased lineage-tracking approach to explore the origins and properties of memory B cell subsets in mice with an intact immune system. We find that activated B cells continue to differentiate into memory B cells throughout the immune response. When defined on the basis of their origins, the memory B cells originating from activated B cells or GCs differ in isotype and overall gene expression, somatic hypermutation, and their affinity for antigen. © 2021 Viant et al.