InVivoMAb anti-mouse CD3ε
Product Details
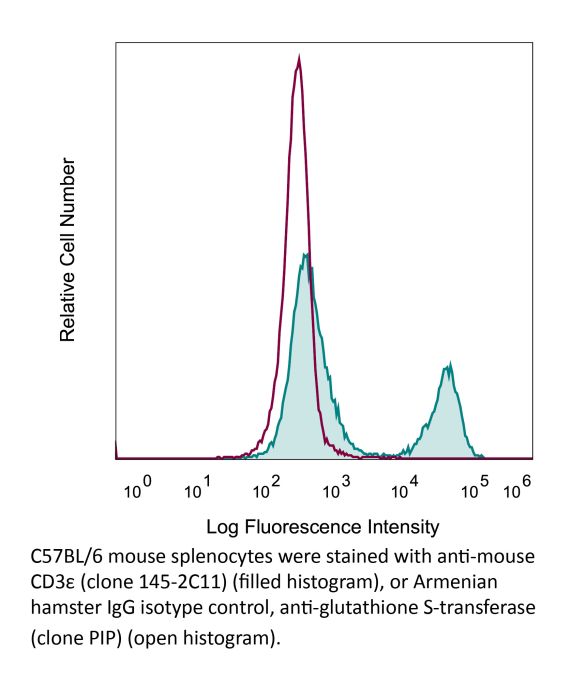
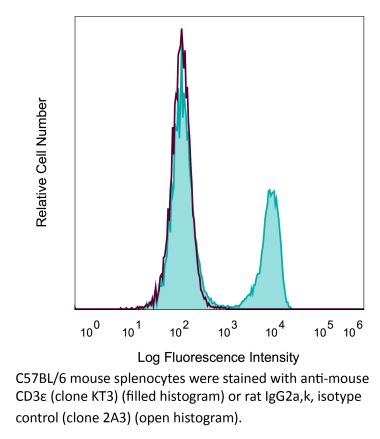
The 145-2C11 monoclonal antibody reacts with mouse CD3ε, a 20 kDa transmembrane cell-surface protein that belongs to the immunoglobulin superfamily. CD3ε is one of five polypeptide chains that combine to form the TCR complex. CD3ε is expressed on T lymphocytes, NK-T cells, and to varying degrees on developing thymocytes. CD3 plays roles in TCR signaling, T lymphocyte activation, and antigen recognition. The 145-2C11 antibody has been shown to induce T lymphocyte activation, proliferation, and apoptosis via binding and stimulating the TCR. Additionally, the 145-2C11 antibody has been reported to block the binding of the 17A2 antibody to CD3ε+ T lymphocytes.Specifications
| Isotype | Armenian Hamster IgG1 |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse BM10-37 cytotoxic T cells |
| Reported Applications |
in vivo T cell depletion in vitro T cell stimulation/activation Immunofluorescence Flow cytometry Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein A |
| RRID | AB_1107634 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo T cell depletion
Glasner, A., et al. (2018). "NKp46 Receptor-Mediated Interferon-gamma Production by Natural Killer Cells Increases Fibronectin 1 to Alter Tumor Architecture and Control Metastasis" Immunity 48(1): 107-119 e104. PubMed
Natural killer (NK) cells are innate lymphoid cells, and their presence within human tumors correlates with better prognosis. However, the mechanisms by which NK cells control tumors in vivo are unclear. Here, we used reflectance confocal microscopy (RCM) imaging in humans and in mice to visualize tumor architecture in vivo. We demonstrated that signaling via the NK cell receptor NKp46 (human) and Ncr1 (mouse) induced interferon-gamma (IFN-gamma) secretion from intratumoral NK cells. NKp46- and Ncr1-mediated IFN-gamma production led to the increased expression of the extracellular matrix protein fibronectin 1 (FN1) in the tumors, which altered primary tumor architecture and resulted in decreased metastases formation. Injection of IFN-gamma into tumor-bearing mice or transgenic overexpression of Ncr1 in NK cells in mice resulted in decreased metastasis formation. Thus, we have defined a mechanism of NK cell-mediated control of metastases in vivo that may help develop NK cell-dependent cancer therapies.
in vitro T cell stimulation/activation
Wendland, K., et al. (2018). "Retinoic Acid Signaling in Thymic Epithelial Cells Regulates Thymopoiesis" J Immunol 201(2): 524-532. PubMed
Despite the essential role of thymic epithelial cells (TEC) in T cell development, the signals regulating TEC differentiation and homeostasis remain incompletely understood. In this study, we show a key in vivo role for the vitamin A metabolite, retinoic acid (RA), in TEC homeostasis. In the absence of RA signaling in TEC, cortical TEC (cTEC) and CD80(lo)MHC class II(lo) medullary TEC displayed subset-specific alterations in gene expression, which in cTEC included genes involved in epithelial proliferation, development, and differentiation. Mice whose TEC were unable to respond to RA showed increased cTEC proliferation, an accumulation of stem cell Ag-1(hi) cTEC, and, in early life, a decrease in medullary TEC numbers. These alterations resulted in reduced thymic cellularity in early life, a reduction in CD4 single-positive and CD8 single-positive numbers in both young and adult mice, and enhanced peripheral CD8(+) T cell survival upon TCR stimulation. Collectively, our results identify RA as a regulator of TEC homeostasis that is essential for TEC function and normal thymopoiesis.
in vitro T cell stimulation/activation
Lacher, S. M., et al. (2018). "NF-kappaB inducing kinase (NIK) is an essential post-transcriptional regulator of T-cell activation affecting F-actin dynamics and TCR signaling" J Autoimmun 94: 110-121. PubMed
NF-kappaB inducing kinase (NIK) is the key protein of the non-canonical NF-kappaB pathway and is important for the development of lymph nodes and other secondary immune organs. We elucidated the specific role of NIK in T cells using T-cell specific NIK-deficient (NIK(DeltaT)) mice. Despite showing normal development of lymphoid organs, NIK(DeltaT) mice were resistant to induction of CNS autoimmunity. T cells from NIK(DeltaT) mice were deficient in late priming, failed to up-regulate T-bet and to transmigrate into the CNS. Proteomic analysis of activated NIK(-/-) T cells showed de-regulated expression of proteins involved in the formation of the immunological synapse: in particular, proteins involved in cytoskeleton dynamics. In line with this we found that NIK-deficient T cells were hampered in phosphorylation of Zap70, LAT, AKT, ERK1/2 and PLCgamma upon TCR engagement. Hence, our data disclose a hitherto unknown function of NIK in T-cell priming and differentiation.
in vitro T cell stimulation/activation
Ron-Harel, N., et al. (2016). "Mitochondrial Biogenesis and Proteome Remodeling Promote One-Carbon Metabolism for T Cell Activation" Cell Metab 24(1): 104-117. PubMed
Naive T cell stimulation activates anabolic metabolism to fuel the transition from quiescence to growth and proliferation. Here we show that naive CD4(+) T cell activation induces a unique program of mitochondrial biogenesis and remodeling. Using mass spectrometry, we quantified protein dynamics during T cell activation. We identified substantial remodeling of the mitochondrial proteome over the first 24 hr of T cell activation to generate mitochondria with a distinct metabolic signature, with one-carbon metabolism as the most induced pathway. Salvage pathways and mitochondrial one-carbon metabolism, fed by serine, contribute to purine and thymidine synthesis to enable T cell proliferation and survival. Genetic inhibition of the mitochondrial serine catabolic enzyme SHMT2 impaired T cell survival in culture and antigen-specific T cell abundance in vivo. Thus, during T cell activation, mitochondrial proteome remodeling generates specialized mitochondria with enhanced one-carbon metabolism that is critical for T cell activation and survival.
in vitro T cell stimulation/activation
Liu, H., et al. (2015). "The Immune Adaptor SLP-76 Binds to SUMO-RANGAP1 at Nuclear Pore Complex Filaments to Regulate Nuclear Import of Transcription Factors in T Cells" Mol Cell 59(5): 840-849. PubMed
While immune cell adaptors regulate proximal T cell signaling, direct regulation of the nuclear pore complex (NPC) has not been reported. NPC has cytoplasmic filaments composed of RanGAP1 and RanBP2 with the potential to interact with cytoplasmic mediators. Here, we show that the immune cell adaptor SLP-76 binds directly to SUMO-RanGAP1 of cytoplasmic fibrils of the NPC, and that this interaction is needed for optimal NFATc1 and NF-kappaB p65 nuclear entry in T cells. Transmission electron microscopy showed anti-SLP-76 cytoplasmic labeling of the majority of NPCs in anti-CD3 activated T cells. Further, SUMO-RanGAP1 bound to the N-terminal lysine 56 of SLP-76 where the interaction was needed for optimal RanGAP1-NPC localization and GAP exchange activity. While the SLP-76-RanGAP1 (K56E) mutant had no effect on proximal signaling, it impaired NF-ATc1 and p65/RelA nuclear entry and in vivo responses to OVA peptide. Overall, we have identified SLP-76 as a direct regulator of nuclear pore function in T cells.
in vitro T cell stimulation/activation
Xu, H., et al. (2015). "Regulation of bifurcating B cell trajectories by mutual antagonism between transcription factors IRF4 and IRF8" Nat Immunol . PubMed
Upon recognition of antigen, B cells undertake a bifurcated response in which some cells rapidly differentiate into plasmablasts while others undergo affinity maturation in germinal centers (GCs). Here we identified a double-negative feedback loop between the transcription factors IRF4 and IRF8 that regulated the initial developmental bifurcation of activated B cells as well as the GC response. IRF8 dampened signaling via the B cell antigen receptor (BCR), facilitated antigen-specific interaction with helper T cells, and promoted antibody affinity maturation while antagonizing IRF4-driven differentiation of plasmablasts. Genomic analysis revealed concentration-dependent actions of IRF4 and IRF8 in regulating distinct gene-expression programs. Stochastic modeling suggested that the double-negative feedback was sufficient to initiate bifurcation of the B cell developmental trajectories.
in vitro T cell stimulation/activation, Immunofluorescence
Kim, Y. U., et al. (2015). "Regulation of autoimmune germinal center reactions in lupus-prone BXD2 mice by follicular helper T cells" PLoS One 10(3): e0120294. PubMed
BXD2 mice spontaneously develop autoantibodies and subsequent glomerulonephritis, offering a useful animal model to study autoimmune lupus. Although initial studies showed a critical contribution of IL-17 and Th17 cells in mediating autoimmune B cell responses in BXD2 mice, the role of follicular helper T (Tfh) cells remains incompletely understood. We found that both the frequency of Th17 cells and the levels of IL-17 in circulation in BXD2 mice were comparable to those of wild-type. By contrast, the frequency of PD-1+ CXCR5+ Tfh cells was significantly increased in BXD2 mice compared with wild-type mice, while the frequency of PD-1+ CXCR5+ Foxp3+ follicular regulatory T (Tfr) cells was reduced in the former group. The frequency of Tfh cells rather than that of Th17 cells was positively correlated with the frequency of germinal center B cells as well as the levels of autoantibodies to dsDNA. More importantly, CXCR5+ CD4+ T cells isolated from BXD2 mice induced the production of IgG from naive B cells in an IL-21-dependent manner, while CCR6+ CD4+ T cells failed to do so. These results together demonstrate that Tfh cells rather than Th17 cells contribute to the autoimmune germinal center reactions in BXD2 mice.
in vitro T cell stimulation/activation
Awe, O., et al. (2015). "PU.1 Expression in T Follicular Helper Cells Limits CD40L-Dependent Germinal Center B Cell Development" J Immunol . PubMed
PU.1 is an ETS family transcription factor that is important for the development of multiple hematopoietic cell lineages. Previous work demonstrated a critical role for PU.1 in promoting Th9 development and in limiting Th2 cytokine production. Whether PU.1 has functions in other Th lineages is not clear. In this study, we examined the effects of ectopic expression of PU.1 in CD4+ T cells and observed decreased expression of genes involved with the function of T follicular helper (Tfh) cells, including Il21 and Tnfsf5 (encoding CD40L). T cells from conditional mutant mice that lack expression of PU.1 in T cells (Sfpi1lck-/-) demonstrated increased production of CD40L and IL-21 in vitro. Following adjuvant-dependent or adjuvant-independent immunization, we observed that Sfpi1lck-/- mice had increased numbers of Tfh cells, increased germinal center B cells (GCB cells), and increased Ab production in vivo. This correlated with increased expression of IL-21 and CD40L in Tfh cells from Sfpi1lck-/- mice compared with control mice. Finally, although blockade of IL-21 did not affect GCB cells in Sfpi1lck-/- mice, anti-CD40L treatment of immunized Sfpi1lck-/- mice decreased GCB cell numbers and Ag-specific Ig concentrations. Together, these data indicate an inhibitory role for PU.1 in the function of Tfh cells, germinal centers, and Tfh-dependent humoral immunity.
in vitro T cell stimulation/activation
Huang, Y., et al. (2015). "CRK proteins selectively regulate T cell migration into inflamed tissues" J Clin Invest 125(3): 1019-1032. PubMed
Effector T cell migration into inflamed sites greatly exacerbates tissue destruction and disease severity in inflammatory diseases, including graft-versus-host disease (GVHD). T cell migration into such sites depends heavily on regulated adhesion and migration, but the signaling pathways that coordinate these functions downstream of chemokine receptors are largely unknown. Using conditional knockout mice, we found that T cells lacking the adaptor proteins CRK and CRK-like (CRKL) exhibit reduced integrin-dependent adhesion, chemotaxis, and diapedesis. Moreover, these two closely related proteins exhibited substantial functional redundancy, as ectopic expression of either protein rescued defects in T cells lacking both CRK and CRKL. We determined that CRK proteins coordinate with the RAP guanine nucleotide exchange factor C3G and the adhesion docking molecule CASL to activate the integrin regulatory GTPase RAP1. CRK proteins were required for effector T cell trafficking into sites of inflammation, but not for migration to lymphoid organs. In a murine bone marrow transplantation model, the differential migration of CRK/CRKL-deficient T cells resulted in efficient graft-versus-leukemia responses with minimal GVHD. Together, the results from our studies show that CRK family proteins selectively regulate T cell adhesion and migration at effector sites and suggest that these proteins have potential as therapeutic targets for preventing GVHD.
in vitro T cell stimulation/activation
Gu, A. D., et al. (2015). "A critical role for transcription factor Smad4 in T cell function that is independent of transforming growth factor beta receptor signaling" Immunity 42(1): 68-79. PubMed
Transforming growth factor-beta (TGF-beta) suppresses T cell function to maintain self-tolerance and to promote tumor immune evasion. Yet how Smad4, a transcription factor component of TGF-beta signaling, regulates T cell function remains unclear. Here we have demonstrated an essential role for Smad4 in promoting T cell function during autoimmunity and anti-tumor immunity. Smad4 deletion rescued the lethal autoimmunity resulting from transforming growth factor-beta receptor (TGF-betaR) deletion and compromised T-cell-mediated tumor rejection. Although Smad4 was dispensable for T cell generation, homeostasis, and effector function, it was essential for T cell proliferation after activation in vitro and in vivo. The transcription factor Myc was identified to mediate Smad4-controlled T cell proliferation. This study thus reveals a requirement of Smad4 for T-cell-mediated autoimmunity and tumor rejection, which is beyond the current paradigm. It highlights a TGF-betaR-independent role for Smad4 in promoting T cell function, autoimmunity, and anti-tumor immunity.
in vitro T cell stimulation/activation
Rabenstein, H., et al. (2014). "Differential kinetics of antigen dependency of CD4+ and CD8+ T cells" J Immunol 192(8): 3507-3517. PubMed
Ag recognition via the TCR is necessary for the expansion of specific T cells that then contribute to adaptive immunity as effector and memory cells. Because CD4+ and CD8+ T cells differ in terms of their priming APCs and MHC ligands we compared their requirements of Ag persistence during their expansion phase side by side. Proliferation and effector differentiation of TCR transgenic and polyclonal mouse T cells were thus analyzed after transient and continuous TCR signals. Following equally strong stimulation, CD4+ T cell proliferation depended on prolonged Ag presence, whereas CD8+ T cells were able to divide and differentiate into effector cells despite discontinued Ag presentation. CD4+ T cell proliferation was neither affected by Th lineage or memory differentiation nor blocked by coinhibitory signals or missing inflammatory stimuli. Continued CD8+ T cell proliferation was truly independent of self-peptide/MHC-derived signals. The subset divergence was also illustrated by surprisingly broad transcriptional differences supporting a stronger propensity of CD8+ T cells to programmed expansion. These T cell data indicate an intrinsic difference between CD4+ and CD8+ T cells regarding the processing of TCR signals for proliferation. We also found that the presentation of a MHC class II-restricted peptide is more efficiently prolonged by dendritic cell activation in vivo than a class I bound one. In summary, our data demonstrate that CD4+ T cells require continuous stimulation for clonal expansion, whereas CD8+ T cells can divide following a much shorter TCR signal.
in vitro T cell stimulation/activation
Bertin, S., et al. (2014). "The ion channel TRPV1 regulates the activation and proinflammatory properties of CD4(+) T cells" Nat Immunol 15(11): 1055-1063. PubMed
TRPV1 is a Ca(2+)-permeable channel studied mostly as a pain receptor in sensory neurons. However, its role in other cell types is poorly understood. Here we found that TRPV1 was functionally expressed in CD4(+) T cells, where it acted as a non-store-operated Ca(2+) channel and contributed to T cell antigen receptor (TCR)-induced Ca(2+) influx, TCR signaling and T cell activation. In models of T cell-mediated colitis, TRPV1 promoted colitogenic T cell responses and intestinal inflammation. Furthermore, genetic and pharmacological inhibition of TRPV1 in human CD4(+) T cells recapitulated the phenotype of mouse Trpv1(-/-) CD4(+) T cells. Our findings suggest that inhibition of TRPV1 could represent a new therapeutic strategy for restraining proinflammatory T cell responses.
in vitro T cell stimulation/activation, Flow Cytometry
Tang, W., et al. (2014). "The oncoprotein and transcriptional regulator Bcl-3 governs plasticity and pathogenicity of autoimmune T cells" Immunity 41(4): 555-566. PubMed
Bcl-3 is an atypical member of the IkappaB family that modulates transcription in the nucleus via association with p50 (NF-kappaB1) or p52 (NF-kappaB2) homodimers. Despite evidence attesting to the overall physiologic importance of Bcl-3, little is known about its cell-specific functions or mechanisms. Here we demonstrate a T-cell-intrinsic function of Bcl-3 in autoimmunity. Bcl-3-deficient T cells failed to induce disease in T cell transfer-induced colitis and experimental autoimmune encephalomyelitis. The protection against disease correlated with a decrease in Th1 cells that produced the cytokines IFN-gamma and GM-CSF and an increase in Th17 cells. Although differentiation into Th1 cells was not impaired in the absence of Bcl-3, differentiated Th1 cells converted to less-pathogenic Th17-like cells, in part via mechanisms involving expression of the RORgammat transcription factor. Thus, Bcl-3 constrained Th1 cell plasticity and promoted pathogenicity by blocking conversion to Th17-like cells, revealing a unique type of regulation that shapes adaptive immunity.
in vitro T cell stimulation/activation
Vegran, F., et al. (2014). "The transcription factor IRF1 dictates the IL-21-dependent anticancer functions of TH9 cells" Nat Immunol 15(8): 758-766. PubMed
The TH9 subset of helper T cells was initially shown to contribute to the induction of autoimmune and allergic diseases, but subsequent evidence has suggested that these cells also exert antitumor activities. However, the molecular events that account for their effector properties are elusive. Here we found that the transcription factor IRF1 enhanced the effector function of TH9 cells and dictated their anticancer properties. Under TH9-skewing conditions, interleukin 1beta (IL-1beta) induced phosphorylation of the transcription factor STAT1 and subsequent expression of IRF1, which bound to the promoters of Il9 and Il21 and enhanced secretion of the cytokines IL-9 and IL-21 from TH9 cells. Furthermore, IL-1beta-induced TH9 cells exerted potent anticancer functions in an IRF1- and IL-21-dependent manner. Our findings thus identify IRF1 as a target for controlling the function of TH9 cells.
in vitro T cell stimulation/activation
Berger, H., et al. (2013). "SOCS3 transactivation by PPARgamma prevents IL-17-driven cancer growth" Cancer Res 73(12): 3578-3590. PubMed
Activation of the transcription factor PPARgamma by the n-3 fatty acid docosahexaenoic acid (DHA) is implicated in controlling proinflammatory cytokine secretion, but the intracellular signaling pathways engaged by PPARgamma are incompletely characterized. Here, we identify the adapter-encoding gene SOCS3 as a critical transcriptional target of PPARgamma. SOCS3 promoter binding and gene transactivation by PPARgamma was associated with a repression in differentiation of proinflammatory T-helper (TH)17 cells. Accordingly, TH17 cells induced in vitro displayed increased SOCS3 expression and diminished capacity to produce interleukin (IL)-17 following activation of PPARgamma by DHA. Furthermore, naive CD4 T cells derived from mice fed a DHA-enriched diet displayed less capability to differentiate into TH17 cells. In two different mouse models of cancer, DHA prevented tumor outgrowth and angiogenesis in an IL-17-dependent manner. Altogether, our results uncover a novel molecular pathway by which PPARgamma-induced SOCS3 expression prevents IL-17-mediated cancer growth.
in vitro T cell stimulation/activation
Sledzinska, A., et al. (2013). "TGF-beta signalling is required for CD4(+) T cell homeostasis but dispensable for regulatory T cell function" PLoS Biol 11(10): e1001674. PubMed
TGF-beta is widely held to be critical for the maintenance and function of regulatory T (T(reg)) cells and thus peripheral tolerance. This is highlighted by constitutive ablation of TGF-beta receptor (TR) during thymic development in mice, which leads to a lethal autoimmune syndrome. Here we describe that TGF-beta-driven peripheral tolerance is not regulated by TGF-beta signalling on mature CD4(+) T cells. Inducible TR2 ablation specifically on CD4(+) T cells did not result in a lethal autoinflammation. Transfer of these TR2-deficient CD4(+) T cells to lymphopenic recipients resulted in colitis, but not overt autoimmunity. In contrast, thymic ablation of TR2 in combination with lymphopenia led to lethal multi-organ inflammation. Interestingly, deletion of TR2 on mature CD4(+) T cells does not result in the collapse of the T(reg) cell population as observed in constitutive models. Instead, a pronounced enlargement of both regulatory and effector memory T cell pools was observed. This expansion is cell-intrinsic and seems to be caused by increased T cell receptor sensitivity independently of common gamma chain-dependent cytokine signals. The expression of Foxp3 and other regulatory T cells markers was not dependent on TGF-beta signalling and the TR2-deficient T(reg) cells retained their suppressive function both in vitro and in vivo. In summary, absence of TGF-beta signalling on mature CD4(+) T cells is not responsible for breakdown of peripheral tolerance, but rather controls homeostasis of mature T cells in adult mice.
in vitro T cell stimulation/activation
Goswami, R., et al. (2012). "STAT6-dependent regulation of Th9 development" J Immunol 188(3): 968-975. PubMed
Th cell effector subsets develop in response to specific cytokine environments. The development of a particular cytokine-secreting pattern requires an integration of signals that may promote the development of opposing pathways. A recent example of this paradigm is the IL-9-secreting Th9 cell that develops in response to TGF-beta and IL-4, cytokines that, in isolation, promote the development of inducible regulatory T cells and Th2 cells, respectively. To determine how the balance of these factors results in priming for IL-9 secretion, we examined the effects of each pathway on transcription factors that regulate Th cell differentiation. We demonstrated that TGF-beta induces the PU.1-encoding Sfpi1 locus and that this is independent of IL-4-induced STAT6 activation. IL-4-activated STAT6 is required for repressing the expression of T-bet and Foxp3 in Th9 cells, transcription factors that inhibit IL-9 production, and STAT6 is required for the induction of IRF4, which promotes Th9 development. These data established a transcription factor network that regulates IL-9 and demonstrated how combinations of cytokine signals generate cytokine-secreting potential by altering the expression of a panel of transcription factors.
in vivo T cell depletion
Peng, B., et al. (2009). "Anti-CD3 antibodies modulate anti-factor VIII immune responses in hemophilia A mice after factor VIII plasmid-mediated gene therapy" Blood 114(20): 4373-4382. PubMed
One major obstacle in gene therapy is the generation of immune responses directed against transgene product. Five consecutive anti-CD3 treatments concomitant with factor VIII (FVIII) plasmid injection prevented the formation of inhibitory antibodies against FVIII and achieved persistent, therapeutic levels of FVIII gene expression in treated hemophilia A mice. Repeated plasmid gene transfer is applicable in tolerized mice without eliciting immune responses. Anti-CD3 treatment significantly depleted both CD4+ and CD8+ T cells, whereas increased transforming growth factor-beta levels in plasma and the frequency of both CD4+CD25+FoxP3+ and CD4+CD25-Foxp3+ regulatory T cells in the initial few weeks after treatment. Although prior depletion of CD4+CD25+ cells did not abrogate tolerance induction, adoptive transfer of CD4+ cells from tolerized mice at 6 weeks after treatment protected recipient mice from anti-FVIII immune responses. Anti-CD3-treated mice mounted immune responses against both T-dependent and T-independent neo-antigens, indicating that anti-CD3 did not hamper the immune systems in the long term. Concomitant FVIII plasmid + anti-CD3 treatment induced long-term tolerance specific to FVIII via a mechanism involving the increase in transforming growth factor-beta levels and the generation of adaptive FVIII-specific CD4+Foxp3+ regulatory T cells at the periphery. Furthermore, anti-CD3 can reduce the titers of preexisting anti-FVIII inhibitory antibodies in hemophilia A mice.
in vitro T cell stimulation/activation
Dardalhon, V., et al. (2008). "IL-4 inhibits TGF-beta-induced Foxp3+ T cells and, together with TGF-beta, generates IL-9+ IL-10+ Foxp3(-) effector T cells" Nat Immunol 9(12): 1347-1355. PubMed
Transcription factor Foxp3 is critical for generating regulatory T cells (T(reg) cells). Transforming growth factor-beta (TGF-beta) induces Foxp3 and suppressive T(reg) cells from naive T cells, whereas interleukin 6 (IL-6) inhibits the generation of inducible T(reg) cells. Here we show that IL-4 blocked the generation of TGF-beta-induced Foxp3(+) T(reg) cells and instead induced a population of T helper cells that produced IL-9 and IL-10. The IL-9(+)IL-10(+) T cells demonstrated no regulatory properties despite producing abundant IL-10. Adoptive transfer of IL-9(+)IL-10(+) T cells into recombination-activating gene 1-deficient mice induced colitis and peripheral neuritis, the severity of which was aggravated if the IL-9(+)IL-10(+) T cells were transferred with CD45RB(hi) CD4(+) effector T cells. Thus IL-9(+)IL-10(+) T cells lack suppressive function and constitute a distinct population of helper-effector T cells that promote tissue inflammation.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
CPT-11 mitigates autoimmune diseases by suppressing effector T cells without affecting long-term anti-tumor immunity.
In Cell Death Discovery on 4 May 2024 by Liang, H., Fan, X., et al.
PubMed
The incidence of autoimmune diseases has significantly increased over the past 20 years. Excessive host immunoreactions and disordered immunoregulation are at the core of the pathogenesis of autoimmune diseases. The traditional anti-tumor chemotherapy drug CPT-11 is associated with leukopenia. Considering that CPT-11 induces leukopenia, we believe that it is a promising drug for the control of autoimmune diseases. Here, we show that CPT-11 suppresses T cell proliferation and pro-inflammatory cytokine production in healthy C57BL/6 mice and in complete Freund's adjuvant-challenged mice. We found that CPT-11 effectively inhibited T cell proliferation and Th1 and Th17 cell differentiation by inhibiting glycolysis in T cells. We also assessed CPT-11 efficacy in treating autoimmune diseases in models of experimental autoimmune encephalomyelitis and psoriasis. Finally, we proved that treatment of autoimmune diseases with CPT-11 did not suppress long-term immune surveillance for cancer. Taken together, these results show that CPT-11 is a promising immunosuppressive drug for autoimmune disease treatment. © 2024. The Author(s).
- Immunology and Microbiology,
- Cancer Research
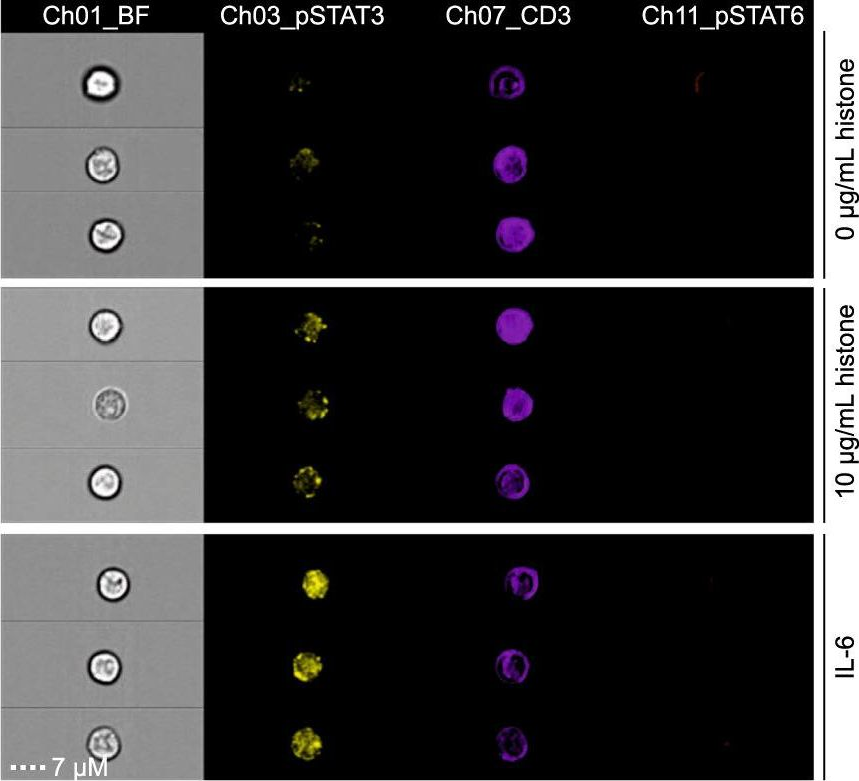
Integrating multiplexed imaging and multiscale modeling identifies tumor phenotype conversion as a critical component of therapeutic T cell efficacy.
In Cell Systems on 17 April 2024 by Hickey, J. W., Agmon, E., et al.
PubMed
Cancer progression is a complex process involving interactions that unfold across molecular, cellular, and tissue scales. These multiscale interactions have been difficult to measure and to simulate. Here, we integrated CODEX multiplexed tissue imaging with multiscale modeling software to model key action points that influence the outcome of T cell therapies with cancer. The initial phenotype of therapeutic T cells influences the ability of T cells to convert tumor cells to an inflammatory, anti-proliferative phenotype. This T cell phenotype could be preserved by structural reprogramming to facilitate continual tumor phenotype conversion and killing. One takeaway is that controlling the rate of cancer phenotype conversion is critical for control of tumor growth. The results suggest new design criteria and patient selection metrics for T cell therapies, call for a rethinking of T cell therapeutic implementation, and provide a foundation for synergistically integrating multiplexed imaging data with multiscale modeling of the cancer-immune interface. A record of this paper's transparent peer review process is included in the supplemental information. Copyright © 2024 The Author(s). Published by Elsevier Inc. All rights reserved.
- Immunology and Microbiology
HIF1α-glycolysis engages activation-induced cell death to drive IFN-γ induction in hypoxic T cells
Preprint on Research Square on 12 January 2024 by Shi, L., Shen, H., et al.
PubMed
The role of HIF1α-glycolysis in regulating IFN-γ induction in hypoxic T cells is unknown. Given that hypoxia is a common feature in a wide array of pathophysiological contexts such as tumor and that IFN-γ is instrumental for protective immunity, it is of great significance to gain a clear idea on this. Combining pharmacological and genetic gain-of-function and loss-of-function approaches, we find that HIF1α-glycolysis controls IFN-γ induction in both human and mouse T cells activated under hypoxia. Specific deletion of HIF1α in T cells (HIF1α –/– ) and glycolytic inhibition significantly abrogate IFN-γ induction. Conversely, HIF1α stabilization in T cells by hypoxia and VHL deletion (VHL –/– ) promotes IFN-γ production. Mechanistically, reduced IFN-γ production in hypoxic HIF1α –/– T cells is due to attenuated activation-induced cell death but not proliferative defect. We further show that depletion of intracellular acetyl-CoA is a key metabolic underlying mechanism. Hypoxic HIF1α –/– T cells are less able to kill tumor cells, and HIF1α –/– tumor-bearing mice are not responsive to immune checkpoint blockade (ICB) therapy, indicating loss of HIF1α in T cells is a major mechanism of therapeutic resistance to ICBs. Importantly, acetate supplementation restores IFN-γ production in hypoxic HIF1α –/– T cells and re-sensitizes HIF1α –/– tumor-bearing mice to ICBs, providing an effective strategy to overcome ICB resistance. Taken together, our results highlight T cell HIF1α-anaerobic glycolysis as a principal mediator of IFN-γ induction and anti-tumor immunity. Considering that acetate supplementation (i.e., glycerol triacetate (GTA)) is approved to treat infants with Canavan disease, we envision a rapid translation of our findings, justifying further testing of GTA as a repurposed medicine for ICB resistance, a pressing unmet medical need.
- Mus musculus (House mouse),
- Immunology and Microbiology
TRAM deletion attenuates monocyte exhaustion and alleviates sepsis severity.
In Frontiers in Immunology on 2 January 2024 by Wang, J., Wu, Y., et al.
PubMed
Monocyte exhaustion characterized by immune-suppressive features can develop during sepsis and contribute to adverse patient outcomes. However, molecular mechanisms responsible for the establishment of immune-suppressive monocytes with reduced expression of immune-enhancing mediators such as CD86 during sepsis are not well understood. In this study, we identified that the TLR4 intracellular adaptor TRAM plays a key role in mediating the sustained reduction of CD86 expression on exhausted monocytes and generating an immune-suppressive monocyte state. TRAM contributes to the prolonged suppression of CD86 through inducing TAX1BP1 as well as SARM1, collectively inhibiting Akt and NFκB. TRAM deficient mice are protected from cecal slurry-induced experimental sepsis and retain immune-competent monocytes with CD86 expression. Our data reveal a key molecular circuitry responsible for monocyte exhaustion and provide a viable target for rejuvenating functional monocytes and treating sepsis. Copyright © 2023 Wang, Wu, Lin, Zhang and Li.
- Mus musculus (House mouse),
- Immunology and Microbiology
p53 suppresses MHC class II presentation by intestinal epithelium to protect against radiation-induced gastrointestinal syndrome.
In Nature Communications on 2 January 2024 by Wang, J., Chang, C. Y., et al.
PubMed
Radiation-induced gastrointestinal syndrome is a major complication and limiting factor for radiotherapy. Tumor suppressor p53 has a protective role in radiation-induced gastrointestinal toxicity. However, its underlying mechanism remains unclear. Here we report that regulating the IL12-p40/MHC class II signaling pathway is a critical mechanism by which p53 protects against radiation-induced gastrointestinal syndrome. p53 inhibits the expression of inflammatory cytokine IL12-p40, which in turn suppresses the expression of MHC class II on intestinal epithelial cells to suppress T cell activation and inflammation post-irradiation that causes intestinal stem cell damage. Anti-IL12-p40 neutralizing antibody inhibits inflammation and rescues the defects in intestinal epithelial regeneration post-irradiation in p53-deficient mice and prolongs mouse survival. These results uncover that the IL12-p40/MHC class II signaling mediates the essential role of p53 in ensuring intestinal stem cell function and proper immune reaction in response to radiation to protect mucosal epithelium, and suggest a potential therapeutic strategy to protect against radiation-induced gastrointestinal syndrome. © 2024. The Author(s).
- Mus musculus (House mouse),
- Cancer Research
Leukemia-intrinsic determinants of CAR-T response revealed by iterative in vivo genome-wide CRISPR screening.
In Nature Communications on 5 December 2023 by Ramos, A., Koch, C. E., et al.
PubMed
CAR-T therapy is a promising, novel treatment modality for B-cell malignancies and yet many patients relapse through a variety of means, including loss of CAR-T cells and antigen escape. To investigate leukemia-intrinsic CAR-T resistance mechanisms, we performed genome-wide CRISPR-Cas9 loss-of-function screens in an immunocompetent murine model of B-cell acute lymphoblastic leukemia (B-ALL) utilizing a modular guide RNA library. We identified IFNγR/JAK/STAT signaling and components of antigen processing and presentation pathway as key mediators of resistance to CAR-T therapy in vivo; intriguingly, loss of this pathway yielded the opposite effect in vitro (sensitized leukemia to CAR-T cells). Transcriptional characterization of this model demonstrated upregulation of these pathways in tumors relapsed after CAR-T treatment, and functional studies showed a surprising role for natural killer (NK) cells in engaging this resistance program. Finally, examination of data from B-ALL patients treated with CAR-T revealed an association between poor outcomes and increased expression of JAK/STAT and MHC-I in leukemia cells. Overall, our data identify an unexpected mechanism of resistance to CAR-T therapy in which tumor cell interaction with the in vivo tumor microenvironment, including NK cells, induces expression of an adaptive, therapy-induced, T-cell resistance program in tumor cells. © 2023. The Author(s).
- Mus musculus (House mouse),
- Cancer Research
Microsomal glutathione transferase 1 controls metastasis and therapeutic response in melanoma.
In Pharmacological Research : the Official Journal of the Italian Pharmacological Society on 1 October 2023 by Zhang, J., Ye, Z. W., et al.
PubMed
While recent targeted and immunotherapies in malignant melanoma are encouraging, most patients acquire resistance, implicating a need to identify additional drug targets to improve outcomes. Recently, attention has been given to pathways that regulate redox homeostasis, especially the lipid peroxidase pathway that protects cells against ferroptosis. Here we identify microsomal glutathione S-transferase 1 (MGST1), a non-selenium-dependent glutathione peroxidase, as highly expressed in malignant and drug resistant melanomas and as a specific determinant of metastatic spread and therapeutic sensitivity. Loss of MGST1 in mouse and human melanoma enhanced cellular oxidative stress, and diminished glycolysis, oxidative phosphorylation, and pentose phosphate pathway. Gp100 activated pmel-1 T cells killed more Mgst1 KD than control melanoma cells and KD cells were more sensitive to cytotoxic anticancer drugs and ferroptotic cell death. When compared to control, mice bearing Mgst1 KD B16 tumors had more CD8+ T cell infiltration with reduced expression of inhibitory receptors and increased cytokine response, large reduction of lung metastases and enhanced survival. Targeting MGST1 alters the redox balance and limits metastases in melanoma, enhancing the therapeutic index for chemo- and immunotherapies. Copyright © 2023 The Authors. Published by Elsevier Ltd.. All rights reserved.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Pathology
Loss of CD4+ T cell-intrinsic arginase 1 accelerates Th1 response kinetics and reduces lung pathology during influenza infection.
In Immunity on 12 September 2023 by West, E. E., Merle, N. S., et al.
PubMed
Arginase 1 (Arg1), the enzyme catalyzing the conversion of arginine to ornithine, is a hallmark of IL-10-producing immunoregulatory M2 macrophages. However, its expression in T cells is disputed. Here, we demonstrate that induction of Arg1 expression is a key feature of lung CD4+ T cells during mouse in vivo influenza infection. Conditional ablation of Arg1 in CD4+ T cells accelerated both virus-specific T helper 1 (Th1) effector responses and its resolution, resulting in efficient viral clearance and reduced lung pathology. Using unbiased transcriptomics and metabolomics, we found that Arg1-deficiency was distinct from Arg2-deficiency and caused altered glutamine metabolism. Rebalancing this perturbed glutamine flux normalized the cellular Th1 response. CD4+ T cells from rare ARG1-deficient patients or CRISPR-Cas9-mediated ARG1-deletion in healthy donor cells phenocopied the murine cellular phenotype. Collectively, CD4+ T cell-intrinsic Arg1 functions as an unexpected rheostat regulating the kinetics of the mammalian Th1 lifecycle with implications for Th1-associated tissue pathologies. Published by Elsevier Inc.
- Cancer Research,
- Immunology and Microbiology,
- Mus musculus (House mouse)
Universal redirection of CAR T cells against solid tumours via membrane-inserted ligands for the CAR.
In Nature Biomedical Engineering on 1 September 2023 by Zhang, A. Q., Hostetler, A., et al.
PubMed
The effectiveness of chimaeric antigen receptor (CAR) T cell therapies for solid tumours is hindered by difficulties in the selection of an effective target antigen, owing to the heterogeneous expression of tumour antigens and to target antigen expression in healthy tissues. Here we show that T cells with a CAR specific for fluorescein isothiocyanate (FITC) can be directed against solid tumours via the intratumoural administration of a FITC-conjugated lipid-poly(ethylene)-glycol amphiphile that inserts itself into cell membranes. In syngeneic and human tumour xenografts in mice, 'amphiphile tagging' of tumour cells drove tumour regression via the proliferation and accumulation of FITC-specific CAR T cells in the tumours. In syngeneic tumours, the therapy induced the infiltration of host T cells, elicited endogenous tumour-specific T cell priming and led to activity against distal untreated tumours and to protection against tumour rechallenge. Membrane-inserting ligands for specific CARs may facilitate the development of adoptive cell therapies that work independently of antigen expression and of tissue of origin. © 2023. The Author(s).
- Cancer Research,
- Immunology and Microbiology,
- Mus musculus (House mouse)
SLC38A2 and glutamine signalling in cDC1s dictate anti-tumour immunity.
In Nature on 1 August 2023 by Guo, C., You, Z., et al.
PubMed
Cancer cells evade T cell-mediated killing through tumour-immune interactions whose mechanisms are not well understood1,2. Dendritic cells (DCs), especially type-1 conventional DCs (cDC1s), mediate T cell priming and therapeutic efficacy against tumours3. DC functions are orchestrated by pattern recognition receptors3-5, although other signals involved remain incompletely defined. Nutrients are emerging mediators of adaptive immunity6-8, but whether nutrients affect DC function or communication between innate and adaptive immune cells is largely unresolved. Here we establish glutamine as an intercellular metabolic checkpoint that dictates tumour-cDC1 crosstalk and licenses cDC1 function in activating cytotoxic T cells. Intratumoral glutamine supplementation inhibits tumour growth by augmenting cDC1-mediated CD8+ T cell immunity, and overcomes therapeutic resistance to checkpoint blockade and T cell-mediated immunotherapies. Mechanistically, tumour cells and cDC1s compete for glutamine uptake via the transporter SLC38A2 to tune anti-tumour immunity. Nutrient screening and integrative analyses show that glutamine is the dominant amino acid in promoting cDC1 function. Further, glutamine signalling via FLCN impinges on TFEB function. Loss of FLCN in DCs selectively impairs cDC1 function in vivo in a TFEB-dependent manner and phenocopies SLC38A2 deficiency by eliminating the anti-tumour therapeutic effect of glutamine supplementation. Our findings establish glutamine-mediated intercellular metabolic crosstalk between tumour cells and cDC1s that underpins tumour immune evasion, and reveal glutamine acquisition and signalling in cDC1s as limiting events for DC activation and putative targets for cancer treatment. © 2023. The Author(s).
- Mus musculus (House mouse)
Resolving neutrophils due to TRAM deletion renders protection against experimental sepsis.
In Inflammation Research : Official Journal of the European Histamine Research Society ... [et Al.] on 1 August 2023 by Lin, R., Wang, J., et al.
PubMed
Proper inflammation resolution is crucial to prevent runaway inflammation during sepsis and reduce sepsis-related mortality/morbidity. Previous studies suggest that deleting TRAM, a key TLR4 signaling adaptor, can reprogram the first inflammatory responder cell-neutrophil from an inflammatory state to a resolving state. In this study, we aim to examine the therapeutic potential of TRAM-deficient neutrophils in vivo with recipient mice undergoing experimental sepsis. Wild-type or Tram-/- mice were intraperitoneally injected with cecal slurry to induce either severe or mild sepsis. Phenotypic examinations of sepsis and neutrophil characteristics were examined in vivo and ex vivo. The propagations of resolution from donor neutrophils to recipient cells such as monocytes, T cells, and endothelial cells were examined through co-culture assays in vitro. The efficacies of Tram-/- neutrophils in reducing inflammation were studied by transfusing either wild-type or Tram-/- neutrophils into septic recipient mice. Tram-/- septic mice had improved survival and attenuated injuries within the lung and kidney tissues as compared to wild-type septic mice. Wild-type septic mice transfused with Tram-/- resolving neutrophils exhibited reduced multi-organ damages and improved cellular homeostasis. In vitro co-culture studies revealed that donor Tram-/- neutrophils can effectively propagate cellular homeostasis to co-cultured neighboring monocytes, neutrophils, T cells as well as endothelial cells. Neutrophils with TRAM deletion render effective reprogramming into a resolving state beneficial for ameliorating experimental sepsis, with therapeutic potential in propagating cellular and tissue homeostasis as well as treating sepsis. © 2023. The Author(s), under exclusive licence to Springer Nature Switzerland AG.
- Immunology and Microbiology,
- Cancer Research,
- Mus musculus (House mouse)
Vaccine-boosted CAR T crosstalk with host immunity to reject tumors with antigen heterogeneity.
In Cell on 20 July 2023 by Ma, L., Hostetler, A., et al.
PubMed
Chimeric antigen receptor (CAR) T cell therapy effectively treats human cancer, but the loss of the antigen recognized by the CAR poses a major obstacle. We found that in vivo vaccine boosting of CAR T cells triggers the engagement of the endogenous immune system to circumvent antigen-negative tumor escape. Vaccine-boosted CAR T promoted dendritic cell (DC) recruitment to tumors, increased tumor antigen uptake by DCs, and elicited the priming of endogenous anti-tumor T cells. This process was accompanied by shifts in CAR T metabolism toward oxidative phosphorylation (OXPHOS) and was critically dependent on CAR-T-derived IFN-γ. Antigen spreading (AS) induced by vaccine-boosted CAR T enabled a proportion of complete responses even when the initial tumor was 50% CAR antigen negative, and heterogeneous tumor control was further enhanced by the genetic amplification of CAR T IFN-γ expression. Thus, CAR-T-cell-derived IFN-γ plays a critical role in promoting AS, and vaccine boosting provides a clinically translatable strategy to drive such responses against solid tumors. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cell Biology,
- Genetics
Endoplasmic reticulum stress in the intestinal epithelium initiates purine metabolite synthesis and promotes Th17 cell differentiation in the gut.
In Immunity on 9 May 2023 by Duan, J., Matute, J. D., et al.
PubMed
Intestinal IL-17-producing T helper (Th17) cells are dependent on adherent microbes in the gut for their development. However, how microbial adherence to intestinal epithelial cells (IECs) promotes Th17 cell differentiation remains enigmatic. Here, we found that Th17 cell-inducing gut bacteria generated an unfolded protein response (UPR) in IECs. Furthermore, subtilase cytotoxin expression or genetic removal of X-box binding protein 1 (Xbp1) in IECs caused a UPR and increased Th17 cells, even in antibiotic-treated or germ-free conditions. Mechanistically, UPR activation in IECs enhanced their production of both reactive oxygen species (ROS) and purine metabolites. Treating mice with N-acetyl-cysteine or allopurinol to reduce ROS production and xanthine, respectively, decreased Th17 cells that were associated with an elevated UPR. Th17-related genes also correlated with ER stress and the UPR in humans with inflammatory bowel disease. Overall, we identify a mechanism of intestinal Th17 cell differentiation that emerges from an IEC-associated UPR. Copyright © 2023 Elsevier Inc. All rights reserved.
Restraint of IFN-γ expression through a distal silencer CNS-28 for tissue homeostasis.
In Immunity on 9 May 2023 by Cui, K., Chen, Z., et al.
PubMed
Interferon-γ (IFN-γ) is a key cytokine in response to viral or intracellular bacterial infection in mammals. While a number of enhancers are described to promote IFN-γ responses, to the best of our knowledge, no silencers for the Ifng gene have been identified. By examining H3K4me1 histone modification in naive CD4+ T cells within Ifng locus, we identified a silencer (CNS-28) that restrains Ifng expression. Mechanistically, CNS-28 maintains Ifng silence by diminishing enhancer-promoter interactions within Ifng locus in a GATA3-dependent but T-bet-independent manner. Functionally, CNS-28 restrains Ifng transcription in NK cells, CD4+ cells, and CD8+ T cells during both innate and adaptive immune responses. Moreover, CNS-28 deficiency resulted in repressed type 2 responses due to elevated IFN-γ expression, shifting Th1 and Th2 paradigm. Thus, CNS-28 activity ensures immune cell quiescence by cooperating with other regulatory cis elements within the Ifng gene locus to minimize autoimmunity. Published by Elsevier Inc.
- Genetics,
- Immunology and Microbiology
Immune profiling of adeno-associated virus response identifies B cell-specific targets that enable vector re-administration in mice.
In Gene Therapy on 1 May 2023 by Chen, M., Kim, B., et al.
PubMed
Adeno-associated virus (AAV) vector-based gene therapies can be applied to a wide range of diseases. AAV expression can last for months to years, but vector re-administration may be necessary to achieve life-long treatment. Unfortunately, immune responses against these vectors are potentiated after the first administration, preventing the clinical use of repeated administration of AAVs. Reducing the immune response against AAVs while minimizing broad immunosuppression would improve gene delivery efficiency and long-term safety. In this study, we quantified the contributions of multiple immune system components of the anti-AAV response in mice. We identified B-cell-mediated immunity as a critical component preventing vector re-administration. Additionally, we found that IgG depletion alone was insufficient to enable re-administration, suggesting IgM antibodies play an important role in the immune response against AAV. Further, we found that AAV-mediated transduction is improved in µMT mice that lack functional IgM heavy chains and cannot form mature B-cells relative to wild-type mice. Combined, our results suggest that B-cells, including non-class switched B-cells, are a potential target for therapeutics enabling AAV re-administration. Our results also suggest that the µMT mice are a potentially useful experimental model for gene delivery studies since they allow repeated dosing for more efficient gene delivery from AAVs. © 2022. The Author(s), under exclusive licence to Springer Nature Limited.
- Immunology and Microbiology,
- FC/FACS,
- Mus musculus (House mouse)
Goliath induces inflammation in obese mice by linking fatty acid β-oxidation to glycolysis.
In EMBO Reports on 5 April 2023 by Hao, S., Zhang, S., et al.
PubMed
Obesity is associated with metabolic disorders and chronic inflammation. However, the obesity-associated metabolic contribution to inflammatory induction remains elusive. Here, we show that, compared with lean mice, CD4+ T cells from obese mice exhibit elevated basal levels of fatty acid β-oxidation (FAO), which promote T cell glycolysis and thus hyperactivation, leading to enhanced induction of inflammation. Mechanistically, the FAO rate-limiting enzyme carnitine palmitoyltransferase 1a (Cpt1a) stabilizes the mitochondrial E3 ubiquitin ligase Goliath, which mediates deubiquitination of calcineurin and thus enhances activation of NF-AT signaling, thereby promoting glycolysis and hyperactivation of CD4+ T cells in obesity. We also report the specific GOLIATH inhibitor DC-Gonib32, which blocks this FAO-glycolysis metabolic axis in CD4+ T cells of obese mice and reduces the induction of inflammation. Overall, these findings establish a role of a Goliath-bridged FAO-glycolysis axis in mediating CD4+ T cell hyperactivation and thus inflammation in obese mice. © 2023 The Authors.
- FC/FACS,
- Mus musculus (House mouse),
- Immunology and Microbiology
PD-1 and CTLA-4 exert additive control of effector regulatory T cells at homeostasis.
In Frontiers in Immunology on 25 March 2023 by Pereira, J. A., Lanzar, Z., et al.
PubMed
At homeostasis, a substantial proportion of Foxp3+ T regulatory cells (Tregs) have an activated phenotype associated with enhanced TCR signals and these effector Treg cells (eTregs) co-express elevated levels of PD-1 and CTLA-4. Short term in vivo blockade of the PD-1 or CTLA-4 pathways results in increased eTreg populations, while combination blockade of both pathways had an additive effect. Mechanistically, combination blockade resulted in a reduction of suppressive phospho-SHP2 Y580 in eTreg cells which was associated with increased proliferation, enhanced production of IL-10, and reduced dendritic cell and macrophage expression of CD80 and MHC-II. Thus, at homeostasis, PD-1 and CTLA-4 function additively to regulate eTreg function and the ability to target these pathways in Treg cells may be useful to modulate inflammation. Copyright © 2023 Pereira, Lanzar, Clark, Hart, Douglas, Shallberg, O’Dea, Christian and Hunter.
- Mus musculus (House mouse)
Structural Basis for Self-Discrimination by Neoantigen-Specific TCRs
Preprint on Research Square on 31 January 2023 by Finnigan, J., Newman, J., et al.
PubMed
Physical interactions between T cell receptors (TCRs) and mutation-derived tumour neoantigens (neoAg) presented by major histocompatibility class-I (MHC-I) enable sensitive and specific cytolysis of tumour cells. Adoptive transfer of neoAg-reactive T cells in patients is correlated with response to immunotherapy; however, the structural and cellular mechanisms of neoAg recognition remain poorly understood. We have identified multiple cognate neoAg:TCRs from B16F10, a common murine implantable tumour model of melanoma. We identified a high affinity TCR targeting H2-D b -restricted Hsf2 K72N that conferred specific recognition of B16F10 in vitro and in vivo . Structural characterization of the peptide-MHC (pMHC) binary and pMHC:TCR ternary complexes yielded highresolution crystal structures, revealing the formation of a solvent-exposed hydrophobic arch in H2-Db that enables multiple intermolecular contacts between pMHC and the TCR. These features of structural stability strikingly mimic that of a previously published influenza peptide-H2-D b complex and its corresponding TCR, suggesting that there are shared structural motifs between neoantigens and viral peptides that explain their shared immunogenicity.
- Cancer Research,
- Mus musculus (House mouse)
CD73 Inhibits cGAS-STING and Cooperates with CD39 to Promote Pancreatic Cancer.
In Cancer Immunology Research on 3 January 2023 by Jacoberger-Foissac, C., Cousineau, I., et al.
PubMed
The ectonucleotidases CD39 and CD73 catalyze extracellular ATP to immunosuppressive adenosine, and as such, represent potential cancer targets. We investigated biological impacts of CD39 and CD73 in pancreatic ductal adenocarcinoma (PDAC) by studying clinical samples and experimental mouse tumors. Stromal CD39 and tumoral CD73 expression significantly associated with worse survival in human PDAC samples and abolished the favorable prognostic impact associated with the presence of tumor-infiltrating CD8+ T cells. In mouse transplanted KPC tumors, both CD39 and CD73 on myeloid cells, as well as CD73 on tumor cells, promoted polarization of infiltrating myeloid cells towards an M2-like phenotype, which enhanced tumor growth. CD39 on tumor-specific CD8+ T cells and pancreatic stellate cells also suppressed IFNγ production by T cells. Although therapeutic inhibition of CD39 or CD73 alone significantly delayed tumor growth in vivo, targeting of both ectonucleotidases exhibited markedly superior antitumor activity. CD73 expression on human and mouse PDAC tumor cells also protected against DNA damage induced by gemcitabine and irradiation. Accordingly, large-scale pharmacogenomic analyses of human PDAC cell lines revealed significant associations between CD73 expression and gemcitabine chemoresistance. Strikingly, increased DNA damage in CD73-deficient tumor cells associated with activation of the cGAS-STING pathway. Moreover, cGAS expression in mouse KPC tumor cells was required for antitumor activity of the CD73 inhibitor AB680 in vivo. Our study, thus, illuminates molecular mechanisms whereby CD73 and CD39 seemingly cooperate to promote PDAC progression. ©2022 American Association for Cancer Research.
- Immunology and Microbiology,
- Mus musculus (House mouse)
T cell-intrinsic protein kinase D3 is dispensable for the cells' activation.
In Frontiers in Immunology on 6 December 2022 by Koutník, J., Leitges, M., et al.
PubMed
Protein kinases D (PKDs) are implicated in T cell receptor (TCR) signaling. Of the two T cell-expressed isoforms PKD2 and PKD3, however, only the former one is rather well understood in this immune cell type. Recently, we have observed a putative hyper-phenotype of T cells from conventional PKD3-knockout mice, which we explained as a secondary effect due to a skewed T cell compartment from naïve towards effector/memory T cells already under steady state conditions. Nonetheless, to this end it is not clear whether these aberrations are mediated by a T cell-intrinsic or -extrinsic function of PKD3. To address this question, we have investigated mice lacking PKD3 specifically in the T cell compartment. We could show that T cells from CD4-Cre-driven conditional knockout mice did not phenocopy the ones from conventional PKD3-knockout mice. In brief, no skewing in the T cell compartment of peripheral lymphoid organs, no hyper-activation upon stimulation in vitro or in vivo as well as no aberrations in follicular helper T cells (TFH) upon immunization were observed. Hence, although PKD3 is strongly regulated upon TCR stimulation, in T cells this kinase seems to be dispensable for their activation. The described skewing in the T cell compartment of conventional PKD3-deficient mice seems to be mediated by T cell-extrinsic mechanisms, thus once more emphasizing the importance of cell type-specific mouse models. Copyright © 2022 Koutník, Leitges and Siegmund.