InVivoMAb anti-mouse CXCL9 (MIG)
Product Description
Specifications
| Isotype | Armenian Hamster IgG, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Reported Applications |
in vivo CXCL9 neutralization Immunofluorescence |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein A |
| RRID | AB_2736989 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo CXCL9 neutralization
Moreno-Fernandez, M. E., et al (2021). "PKM2-dependent metabolic skewing of hepatic Th17 cells regulates pathogenesis of non-alcoholic fatty liver disease" Cell Metab 33(6): 1187-1204 e1189.
PubMed
Emerging evidence suggests a key contribution to non-alcoholic fatty liver disease (NAFLD) pathogenesis by Th17 cells. The pathogenic characteristics and mechanisms of hepatic Th17 cells, however, remain unknown. Here, we uncover and characterize a distinct population of inflammatory hepatic CXCR3(+)Th17 (ihTh17) cells sufficient to exacerbate NAFLD pathogenesis. Hepatic ihTh17 cell accrual was dependent on the liver microenvironment and CXCR3 axis activation. Mechanistically, the pathogenic potential of ihTh17 cells correlated with increased chromatin accessibility, glycolytic output, and concomitant production of IL-17A, IFNgamma, and TNFalpha. Modulation of glycolysis using 2-DG or cell-specific PKM2 deletion was sufficient to reverse ihTh17-centric inflammatory vigor and NAFLD severity. Importantly, ihTh17 cell characteristics, CXCR3 axis activation, and hepatic expression of glycolytic genes were conserved in human NAFLD. Together, our data show that the steatotic liver microenvironment regulates Th17 cell accrual, metabolism, and competence toward an ihTh17 fate. Modulation of these pathways holds potential for development of novel therapeutic strategies for NAFLD.
in vivo CXCL9 neutralization
Wang, C., et al (2021). "Reprogramming NK cells and macrophages via combined antibody and cytokine therapy primes tumors for elimination by checkpoint blockade" Cell Rep 37(8): 110021.
PubMed
Treatments aiming to augment immune checkpoint blockade (ICB) in cancer often focus on T cell immunity, but innate immune cells may have important roles to play. Here, we demonstrate a single-dose combination treatment (termed AIP) using a pan-tumor-targeting antibody surrogate, half-life-extended interleukin-2 (IL-2), and anti-programmed cell death 1 (PD-1), which primes tumors to respond to subsequent ICB and promotes rejection of large established tumors in mice. Natural killer (NK) cells and macrophages activated by AIP treatment underwent transcriptional reprogramming; rapidly killed cancer cells; governed the recruitment of cross-presenting dendritic cells (DCs) and other leukocytes; and induced normalization of the tumor vasculature, facilitating further immune infiltration. Thus, innate cell-activating therapies can initiate critical steps leading to a self-sustaining cycle of T cell priming driven by ICB.
in vivo CXCL9 neutralization
Qu, Y., et al (2020). "Baseline Frequency of Inflammatory Cxcl9-Expressing Tumor-Associated Macrophages Predicts Response to Avelumab Treatment" Cell Rep 32(1): 107873.
PubMed
The tumor microenvironment is rich with immune-suppressive macrophages that are associated with cancer progression and resistance to immune checkpoint therapy. Using pre-treatment tumor biopsies complemented with single-cell RNA sequencing (RNA-seq), we characterize intratumoral immune heterogeneity to unveil potential mechanisms of resistance to avelumab (anti-PD-L1). We identify a proinflammatory F480(+)MHCII(+)Ly6C(lo) macrophage population that is associated with response rather than resistance to avelumab. These macrophages are the primary source of the interferon-inducible chemokine Cxcl9, which facilitates the recruitment of protective Cxcr3(+) T cells. Consequently, the efficacy of avelumab in mouse tumor models is dependent on Cxcr3 and Cxcl9, and baseline levels of Cxcl9 in patients treated with avelumab are associated with clinical response and overall survival. These data suggest that, within the broadly immune-suppressive macrophage compartment, a pro-inflammatory population exists that promotes responsiveness to PD-L1 blockade.
in vivo CXCL9 neutralization
Dangaj, D., et al (2019). "Cooperation between Constitutive and Inducible Chemokines Enables T Cell Engraftment and Immune Attack in Solid Tumors" Cancer Cell 35(6): 885-900 e810.
PubMed
We investigated the role of chemokines in regulating T cell accumulation in solid tumors. CCL5 and CXCL9 overexpression was associated with CD8(+) T cell infiltration in solid tumors. T cell infiltration required tumor cell-derived CCL5 and was amplified by IFN-gamma-inducible, myeloid cell-secreted CXCL9. CCL5 and CXCL9 coexpression revealed immunoreactive tumors with prolonged survival and response to checkpoint blockade. Loss of CCL5 expression in human tumors was associated with epigenetic silencing through DNA methylation. Reduction of CCL5 expression caused tumor-infiltrating lymphocyte (TIL) desertification, whereas forced CCL5 expression prevented Cxcl9 expression and TILs loss, and attenuated tumor growth in mice through IFN-gamma. The cooperation between tumor-derived CCL5 and IFN-gamma-inducible CXCR3 ligands secreted by myeloid cells is key for orchestrating T cell infiltration in immunoreactive and immunoresponsive tumors.
Immunofluorescence
Xiong, Y., et al (2016). "T-bet Regulates Natural Regulatory T Cell Afferent Lymphatic Migration and Suppressive Function" J Immunol 196(6): 2526-2540.
PubMed
T-bet is essential for natural regulatory T cells (nTreg) to regulate Th1 inflammation, but whether T-bet controls other Treg functions after entering the inflammatory site is unknown. In an islet allograft model, T-bet(-/-) nTreg, but not induced Treg, failed to prolong graft survival as effectively as wild-type Treg. T-bet(-/-) nTreg had no functional deficiency in vitro but failed to home from the graft to draining lymph nodes (dLN) as efficiently as wild type. T-bet regulated expression of adhesion- and migration-related molecules, influencing nTreg distribution in tissues, so that T-bet(-/-) nTreg remained in the grafts rather than migrating to lymphatics and dLN. In contrast, both wild-type and T-bet(-/-) CD4(+) conventional T cells and induced Treg migrated normally toward afferent lymphatics. T-bet(-/-) nTreg displayed instability in the graft, failing to suppress Ag-specific CD4(+) T cells and prevent their infiltration into the graft and dLN. Thus, T-bet regulates nTreg migration into afferent lymphatics and dLN and consequently their suppressive stability in vivo.
Immunofluorescence
Jin, J. O., et al (2013). "Innate immune signaling induces interleukin-7 production from salivary gland cells and accelerates the development of primary Sjogren’s syndrome in a mouse model" PLoS One 8(10): e77605.
PubMed
Elevated IL-7 in the target tissues is closely associated with multiple autoimmune disorders, including Sjogren’s syndrome (SS). We recently found that IL-7 plays an essential role in the development and onset of primary SS (pSS) in C57BL/6.NOD-Aec1Aec2 mice, a well-defined mouse model of primary SS. However, environmental signals that cause excessive IL-7 production are not well-characterized. Innate immune signaling plays a critical role in shaping the adaptive immune responses including autoimmune responses. We and others have previously shown that innate immune signaling can induce IL-7 expression in lungs and intestines of C57BL/6 mice. In this study, we characterized the effects of poly I:C, a double-stranded RNA analog and toll-like receptor 3 agonist, on the induction of IL-7 expression in salivary glands and on pSS development. We showed that poly I:C administration to C57BL/6 mice rapidly induced IL-7 expression in the salivary glands in a type 1 IFN- and IFN-gamma-dependent manner. Moreover, poly I:C-induced IL-7 contributed to the optimal up-regulation of CXCL9 in the salivary glands, which may subsequently promote recruitment of more IFN-gamma-producing T cells. Repeated administration of poly I:C to C57BL/6.NOD-Aec1Aec2 mice accelerated the development of SS-like exocrinopathy, and this effect was abolished by the blockade of IL-7 receptor signaling with a neutralizing antibody. Finally, poly I:C or a combination of IFN-alpha and IFN-gamma induced IL-7 gene expression and protein production in a human salivary gland epithelial cell line. Hence, we demonstrate that IL-7 expression in the salivary gland cells can be induced by poly I:C and delineate a crucial mechanism by which innate immune signals facilitate the development of pSS, which is through induction of IL-7 in the target tissues.
Immunofluorescence
Sung, J. H., et al (2012). "Chemokine guidance of central memory T cells is critical for antiviral recall responses in lymph nodes" Cell 150(6): 1249-1263.
PubMed
A defining feature of vertebrate immunity is the acquisition of immunological memory, which confers enhanced protection against pathogens by mechanisms that are incompletely understood. Here, we compared responses by virus-specific naive T cells (T(N)) and central memory T cells (T(CM)) to viral antigen challenge in lymph nodes (LNs). In steady-state LNs, both T cell subsets localized in the deep T cell area and interacted similarly with antigen-presenting dendritic cells. However, upon entry of lymph-borne virus, only T(CM) relocalized rapidly and efficiently toward the outermost LN regions in the medullary, interfollicular, and subcapsular areas where viral infection was initially confined. This rapid peripheralization was coordinated by a cascade of cytokines and chemokines, particularly ligands for T(CM)-expressed CXCR3. Consequently, in vivo recall responses to viral infection by CXCR3-deficient T(CM) were markedly compromised, indicating that early antigen detection afforded by intranodal chemokine guidance of T(CM) is essential for efficient antiviral memory.
Product Citations
-
Cxcl9high macrophages recruit circulating Cxcr3+ plasmablasts into kidneys to promote pathogenesis of lupus nephritis mice.
In Commun Biol on 9 October 2025 by Zhao, J., Bai, X., et al.
PubMed
Systemic lupus erythematosus (SLE) is an autoimmune disease driven by autoantibody production. Lupus nephritis (LN), a severe SLE complication, is primarily caused by renal autoantibodies. Long-lived plasma cells (LLPCs), the main producers of these autoantibodies, are especially elevated in the kidney of LN patients, particularly in refractory or recurrent cases. However, the cause of increased LLPCs in LN kidneys remains unknown. This study uses an LN mouse model and combines single-cell RNA sequencing with spatial transcriptomics, finding that kidney-resident Cxcl9high macrophages and their secreted chemokine Cxcl9 significantly rise with disease progression. This increase in Cxcl9 attracts Cxcr3+ plasmablasts in peripheral blood into the kidneys, where they differentiate into LLPCs and produce autoantibodies. Based on these findings, this study suggests that Cxcl9high macrophages are the inducing factor causing the increase of LLPCs in LN kidneys and may be a potential therapeutic target for LN.
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
Immune mechanisms shape the clonal landscape during early progression of prostate cancer.
In Dev Cell on 19 June 2023 by Tshering, L. F., Luo, F., et al.
PubMed
Understanding the role of the immune microenvironment in modulating intratumor heterogeneity is essential for effective cancer therapies. Using multicolor lineage tracing in genetically engineered mouse models and single-cell transcriptomics, we show that slowly progressing tumors contain a multiclonal landscape of relatively homogeneous subpopulations within a well-organized tumor microenvironment. In more advanced and aggressive tumors, however, the multiclonal landscape develops into competing dominant and minor clones accompanied by a disordered microenvironment. We demonstrate that this dominant/minor landscape is associated with differential immunoediting, in which minor clones are marked by an increased expression of IFNγ-response genes and the T cell-activating chemokines Cxcl9 and Cxcl11. Furthermore, immunomodulation of the IFNγ pathway can rescue minor clones from elimination. Notably, the immune-specific gene signature of minor clones exhibits a prognostic value for biochemical recurrence-free survival in human prostate cancer. These findings suggest new immunotherapy approaches for modulating clonal fitness and tumor progression in prostate cancer.
-
-
-
Cancer Research
Nanosecond Pulsed Electric Field Induces an Antitumor Effect in Triple-Negative Breast Cancer via CXCL9 Axis Dependence in Mice.
In Cancers (Basel) on 30 March 2023 by Xu, Z., Pan, C., et al.
PubMed
Triple-negative breast cancer (TNBC) is a refractory tumor, and therapeutic options are very limited. Local ablation has been applied recently. Chemokines play a critical role in the recruitment of immune cells into ablative tumors. Nanosecond pulsed electric field (nsPEF) shows potential anti-tumor efficacy, but the mechanism for maintaining the immune effect is not very clear. Here, we applied nsPEF for treating 4T1 breast cancer cells in vitro. RNA sequencing (RNA-seq) was applied. Anti-CXCL9 was used alone or combined with nsPEF to treat triple-negative breast cancer in mice. We demonstrated that nsPEF effectively induced cell apoptosis and inhibited the growth and metastasis of triple-negative breast cancer. An immune effect, especially chemotaxis, was activated by nsPEF. The number of infiltrated CD8+ T cells was increased significantly. We found that the inhibition of residual breast cancer growth by nsPEF was dependent on the CXCL9 axis. In conclusion, our work demonstrated that nsPEF effectively ablated the tumor, aroused an immune response, and inhibited residual breast cancer growth via CXCL9 axis dependence in mice.
-
-
-
Immunology and Microbiology
-
Neuroscience
-
Mus musculus (Mouse)
Infection induces tissue-resident memory NK cells that safeguard tissue health.
In Immunity on 14 March 2023 by Schuster, I. S., Sng, X. Y. X., et al.
PubMed
Tissue health is dictated by the capacity to respond to perturbations and then return to homeostasis. Mechanisms that initiate, maintain, and regulate immune responses in tissues are therefore essential. Adaptive immunity plays a key role in these responses, with memory and tissue residency being cardinal features. A corresponding role for innate cells is unknown. Here, we have identified a population of innate lymphocytes that we term tissue-resident memory-like natural killer (NKRM) cells. In response to murine cytomegalovirus infection, we show that circulating NK cells were recruited in a CX3CR1-dependent manner to the salivary glands where they formed NKRM cells, a long-lived, tissue-resident population that prevented autoimmunity via TRAIL-dependent elimination of CD4+ T cells. Thus, NK cells develop adaptive-like features, including long-term residency in non-lymphoid tissues, to modulate inflammation, restore immune equilibrium, and preserve tissue health. Modulating the functions of NKRM cells may provide additional strategies to treat inflammatory and autoimmune diseases.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
Tumor PD-L1 engages myeloid PD-1 to suppress type I interferon to impair cytotoxic T lymphocyte recruitment.
In Cancer Cell on 13 March 2023 by Klement, J. D., Redd, P. S., et al.
PubMed
The cellular and molecular mechanisms underlying tumor cell PD-L1 (tPD-L1) function in tumor immune evasion are incompletely understood. We report here that tPD-L1 does not suppress cytotoxic T lymphocyte (CTL) activity in co-cultures of tumor cells and tumor-specific CTLs and exhibits no effect on primary tumor growth. However, deleting tPD-L1 decreases lung metastasis in a CTL-dependent manner in tumor-bearing mice. Depletion of myeloid cells or knocking out PD-1 in myeloid cells (mPD-1) impairs tPD-L1 promotion of tumor lung metastasis in mice. Single-cell RNA sequencing (scRNA-seq) reveals that tPD-L1 engages mPD-1 to activate SHP2 to antagonize the type I interferon (IFN-I) and STAT1 pathway to repress Cxcl9 and impair CTL recruitment to lung metastases. Human cancer patient response to PD-1 blockade immunotherapy correlates with IFN-I response in myeloid cells. Our findings determine that tPD-L1 engages mPD-1 to activate SHP2 to suppress the IFN-I-STAT1-CXCL9 pathway to impair CTL tumor recruitment in lung metastasis.
-
-
-
Immunology and Microbiology
XCR1+ DCs are critical for T cell-mediated immunotherapy of chronic viral infections.
In Cell Rep on 28 February 2023 by Domenjo-Vila, E., Casella, V., et al.
PubMed
The contribution of cross-presenting XCR1+ dendritic cells (DCs) and SIRPα+ DCs in maintaining T cell function during exhaustion and immunotherapeutic interventions of chronic infections remains poorly characterized. Using the mouse model of chronic LCMV infection, we found that XCR1+ DCs are more resistant to infection and highly activated compared with SIRPα+ DCs. Exploiting XCR1+ DCs via Flt3L-mediated expansion or XCR1-targeted vaccination notably reinvigorates CD8+ T cells and improves virus control. Upon PD-L1 blockade, XCR1+ DCs are not required for the proliferative burst of progenitor exhausted CD8+ T (TPEX) cells but are indispensable to sustain the functionality of exhausted CD8+ T (TEX) cells. Combining anti-PD-L1 therapy with increased frequency of XCR1+ DCs improves functionality of TPEX and TEX subsets, while increase of SIRPα+ DCs dampened their proliferation. Together, this demonstrates that XCR1+ DCs are crucial for the success of checkpoint inhibitor-based therapies through differential activation of exhausted CD8+ T cell subsets.
-
-
-
Cancer Research
Anti-PD-L1 antibody enhances curative effect of cryoablation via antibody-dependent cell-mediated cytotoxicity mediating PD-L1highCD11b+ cells elimination in hepatocellular carcinoma.
In Acta Pharm Sin B on 1 February 2023 by Tan, J., Liu, T., et al.
PubMed
Cryoablation (CRA) and microwave ablation (MWA) are two main local treatments for hepatocellular carcinoma (HCC). However, which one is more curative and suitable for combining with immunotherapy is still controversial. Herein, CRA induced higher tumoral PD-L1 expression and more T cells infiltration, but less PD-L1highCD11b+ myeloid cells infiltration than MWA in HCC. Furthermore, CRA had better curative effect than MWA for anti-PD-L1 combination therapy in mouse models. Mechanistically, anti-PD-L1 antibody facilitated infiltration of CD8+ T cells by enhancing the secretion of CXCL9 from cDC1 cells after CRA therapy. On the other hand, anti-PD-L1 antibody promoted the infiltration of NK cells to eliminate PD-L1highCD11b+ myeloid cells by antibody-dependent cell-mediated cytotoxicity (ADCC) effect after CRA therapy. Both aspects relieved the immunosuppressive microenvironment after CRA therapy. Notably, the wild-type PD-L1 Avelumab (Bavencio), compared to the mutant PD-L1 atezolizumab (Tecentriq), was better at inducing the ADCC effect to target PD-L1highCD11b+ myeloid cells. Collectively, our study uncovered the novel insights that CRA showed superior curative effect than MWA in combining with anti-PD-L1 antibody by strengthening CTL/NK cell immune responses, which provided a strong rationale for combining CRA and PD-L1 blockade in the clinical treatment for HCC.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cardiovascular biology
-
Genetics
-
Immunology and Microbiology
-
In vivo experiments
Single-Cell RNA sequencing reveals immune cell dynamics and local intercellular communication in acute murine cardiac allograft rejection.
In Theranostics on 29 September 2022 by Chen, Z., Xu, H., et al.
PubMed
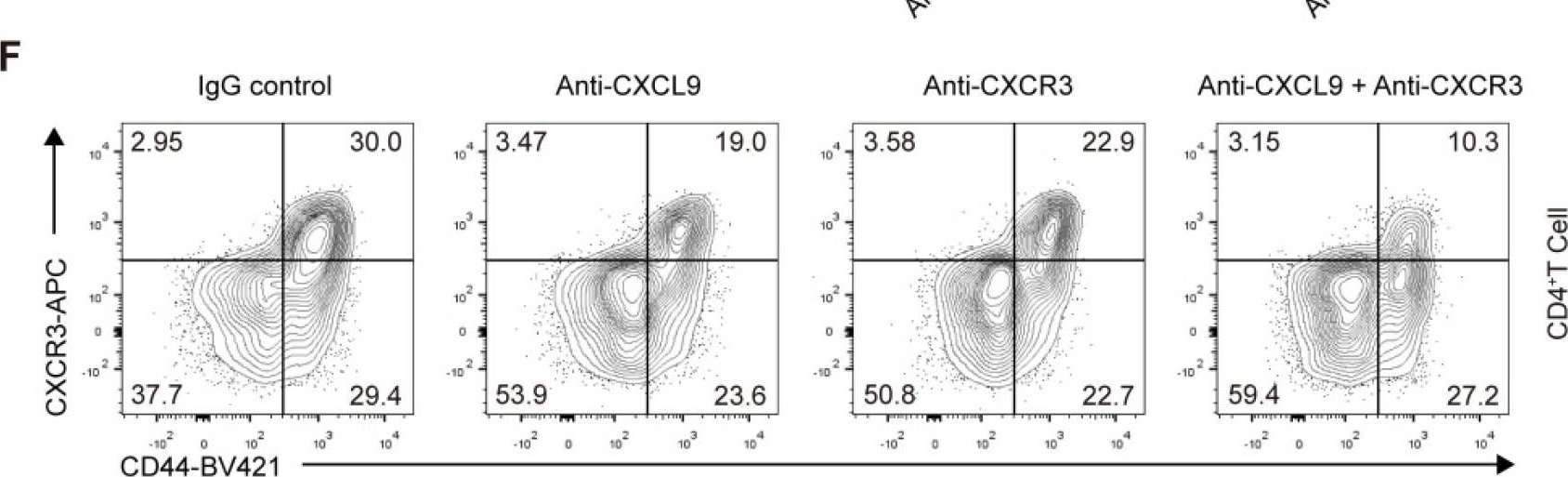
Rationale: Transplant rejection is a major impediment to long-term allograft survival, in which the actions of immune cells are of fundamental importance. However, the immune cell dynamics and local intercellular communication of acute cardiac allograft rejection are not completely clear. Methods: Here we performed single-cell RNA sequencing on CD45+ immune cells isolated from cardiac grafts and spleens in a model of murine heterotopic heart transplantation. Moreover, we applied unsupervised clustering, functional enrichment analysis, cell trajectory construction and intercellular communication analysis to explore the immune cell dynamics and local intercellular communication of acute cardiac allograft rejection at single-cell level. The effect of CXCR3 antagonist and neutralizing antibody against its ligand on allograft rejection and T cell function was evaluated in murine heart transplantation model. Results: We presented the immune cell landscape of acute murine cardiac allograft rejection at single-cell resolution, and uncovered the functional characteristics and differentiation trajectory of several alloreactive cell subpopulations, including Mki67hi CTLs, Ccl5hi CTLs, activated Tregs and alloreactive B cells. We demonstrated local intercellular communication and revealed the upregulation of CXCR3 and its ligands in cardiac allografts. Finally, CXCR3 blockade significantly suppressed acute cardiac allograft rejection and inhibited the alloreactive T cell function. Conclusions: These results provide a new insight into the immune cell dynamics and local intercellular communication of acute cardiac allograft rejection, and suggest CXCR3 pathway may serve as a potential therapeutic target for transplant rejection.
-
-
-
Immunohistochemistry
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
STAT1 is regulated by TRIM24 and promotes immunosuppression in head and neck squamous carcinoma cells, but enhances T cell antitumour immunity in the tumour microenvironment.
In Br J Cancer on 1 September 2022 by Anderson, K., Ryan, N., et al.
PubMed
Head and neck squamous cell carcinoma (HNSCC) is a significant problem and is frequently resistant to current treatments. STAT1 is important in anti-tumour immune responses against HNSCC. However, the role of STAT1 expression by tumour cells and its regulation during HNSCC is unclear.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
The microbiome restrains melanoma bone growth by promoting intestinal NK and Th1 cell homing to bone.
In J Clin Invest on 15 June 2022 by Pal, S., Perrien, D. S., et al.
PubMed
Bone metastases are frequent complications of malignant melanoma leading to reduced quality of life and significant morbidity. Regulation of immune cells by the gut microbiome influences cancer progression, but the role of the microbiome in tumor growth in bone is unknown. Using intracardiac or intratibial injections of B16-F10 melanoma cells into mice, we showed that gut microbiome depletion by broad-spectrum antibiotics accelerated intraosseous tumor growth and osteolysis. Microbiome depletion blunted melanoma-induced expansion of intestinal NK cells and Th1 cells and their migration from the gut to tumor-bearing bones. Demonstrating the functional relevance of immune cell trafficking from the gut to the bone marrow (BM) in bone metastasis, blockade of S1P-mediated intestinal egress of NK and Th1 cells, or inhibition of their CXCR3/CXCL9-mediated influx into the BM, prevented the expansion of BM NK and Th1 cells and accelerated tumor growth and osteolysis. Using a mouse model, this study revealed mechanisms of microbiota-mediated gut-bone crosstalk that are relevant to the immunological restraint of melanoma metastasis and tumor growth in bone. Microbiome modifications induced by antibiotics might have negative clinical consequences in patients with melanoma.
-
-
-
In vitro experiments
-
Mus musculus (Mouse)
-
Immunology and Microbiology
CXCR3 regulates stem and proliferative CD8+ T cells during chronic infection by promoting interactions with DCs in splenic bridging channels.
In Cell Rep on 18 January 2022 by Bangs, D. J., Tsitsiklis, A., et al.
PubMed
Production of effector CD8+ T cells during persistent infection requires a stable pool of stem-like cells that can give rise to effector cells via a proliferative intermediate population. In infection models marked by T cell exhaustion, this process can be transiently induced by checkpoint blockade but occurs spontaneously in mice chronically infected with the protozoan intracellular parasite Toxoplasma gondii. We observe distinct locations for parasite-specific T cell subsets, implying a link between differentiation and anatomical niches in the spleen. Loss of the chemokine receptor CXCR3 on T cells does not prevent white pulp-to-red pulp migration but reduces interactions with CXCR3 ligand-producing dendritic cells (DCs) and impairs memory-to-intermediate transition, leading to a buildup of memory T cells in the red pulp. Thus, CXCR3 increases T cell exposure to differentiation-inducing signals during red pulp migration, providing a dynamic mechanism for modulating effector differentiation in response to environmental signals.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
Reprogramming NK cells and macrophages via combined antibody and cytokine therapy primes tumors for elimination by checkpoint blockade.
In Cell Rep on 23 November 2021 by Wang, C., Cui, A., et al.
PubMed
Treatments aiming to augment immune checkpoint blockade (ICB) in cancer often focus on T cell immunity, but innate immune cells may have important roles to play. Here, we demonstrate a single-dose combination treatment (termed AIP) using a pan-tumor-targeting antibody surrogate, half-life-extended interleukin-2 (IL-2), and anti-programmed cell death 1 (PD-1), which primes tumors to respond to subsequent ICB and promotes rejection of large established tumors in mice. Natural killer (NK) cells and macrophages activated by AIP treatment underwent transcriptional reprogramming; rapidly killed cancer cells; governed the recruitment of cross-presenting dendritic cells (DCs) and other leukocytes; and induced normalization of the tumor vasculature, facilitating further immune infiltration. Thus, innate cell-activating therapies can initiate critical steps leading to a self-sustaining cycle of T cell priming driven by ICB.
-
-
-
Immunodepletion
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
BIRC2 Expression Impairs Anti-Cancer Immunity and Immunotherapy Efficacy.
In Cell Rep on 25 August 2020 by Samanta, D., Huang, T. Y., et al.
PubMed
Immune checkpoint blockade (ICB) has led to therapeutic responses in some cancer patients for whom no effective treatment previously existed. ICB acts on T lymphocytes and other immune cells that are inactivated due to checkpoint signals that inhibit their infiltration and function within tumors. But for more than 80% of patients, immunotherapy has not been effective. Here, we demonstrate a cancer-cell-intrinsic mechanism of immune evasion and resistance to ICB mediated by baculoviral IAP repeat-containing 2 (BIRC2). Knockdown of BIRC2 expression in mouse melanoma or breast cancer cells increases expression of the chemokine CXCL9 and impairs tumor growth by increasing the number of intratumoral activated CD8+ T cells and natural killer cells. Administration of anti-CXCL9 neutralizing antibody inhibits the recruitment of CD8+ T cells and natural killer cells to BIRC2-deficient tumors. Most importantly, BIRC2 deficiency dramatically increases the sensitivity of mouse melanoma and breast tumors to anti-CTLA4 and/or anti-PD1 ICB.
-
-
-
In vivo experiments
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Cooperation between Constitutive and Inducible Chemokines Enables T Cell Engraftment and Immune Attack in Solid Tumors.
In Cancer Cell on 10 June 2019 by Dangaj, D., Bruand, M., et al.
PubMed
We investigated the role of chemokines in regulating T cell accumulation in solid tumors. CCL5 and CXCL9 overexpression was associated with CD8+ T cell infiltration in solid tumors. T cell infiltration required tumor cell-derived CCL5 and was amplified by IFN-γ-inducible, myeloid cell-secreted CXCL9. CCL5 and CXCL9 coexpression revealed immunoreactive tumors with prolonged survival and response to checkpoint blockade. Loss of CCL5 expression in human tumors was associated with epigenetic silencing through DNA methylation. Reduction of CCL5 expression caused tumor-infiltrating lymphocyte (TIL) desertification, whereas forced CCL5 expression prevented Cxcl9 expression and TILs loss, and attenuated tumor growth in mice through IFN-γ. The cooperation between tumor-derived CCL5 and IFN-γ-inducible CXCR3 ligands secreted by myeloid cells is key for orchestrating T cell infiltration in immunoreactive and immunoresponsive tumors.
-