InVivoMAb anti-mouse CD40
Product Description
Specifications
| Isotype | Rat IgG2a |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse CD40 fusion protein |
| Reported Applications |
in vivo CD40 activation in vitro B cell stimulation/activation |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107601 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo CD40 activation
Bauche, D., et al (2018). "LAG3(+) Regulatory T Cells Restrain Interleukin-23-Producing CX3CR1(+) Gut-Resident Macrophages during Group 3 Innate Lymphoid Cell-Driven Colitis" Immunity 49(2): 342-352 e345.
PubMed
Interleukin-22 (IL-22)-producing group 3 innate lymphoid cells (ILC3) maintains gut homeostasis but can also promote inflammatory bowel disease (IBD). The regulation of ILC3-dependent colitis remains to be elucidated. Here we show that Foxp3(+) regulatory T cells (Treg cells) prevented ILC3-mediated colitis in an IL-10-independent manner. Treg cells inhibited IL-23 and IL-1beta production from intestinal-resident CX3CR1(+) macrophages but not CD103(+) dendritic cells. Moreover, Treg cells restrained ILC3 production of IL-22 through suppression of CX3CR1(+) macrophage production of IL-23 and IL-1beta. This suppression was contact dependent and was mediated by latent activation gene-3 (LAG-3)-an immune checkpoint receptor-expressed on Treg cells. Engagement of LAG-3 on MHC class II drove profound immunosuppression of CX3CR1(+) tissue-resident macrophages. Our study reveals that the health of the intestinal mucosa is maintained by an axis driven by Treg cells communication with resident macrophages that withhold inflammatory stimuli required for ILC3 function.
in vivo CD40 activation
Bartkowiak, T., et al (2015). "Unique potential of 4-1BB agonist antibody to promote durable regression of HPV+ tumors when combined with an E6/E7 peptide vaccine" Proc Natl Acad Sci U S A 112(38): E5290-5299.
PubMed
Antibody modulation of T-cell coinhibitory (e.g., CTLA-4) or costimulatory (e.g., 4-1BB) receptors promotes clinical responses to a variety of cancers. Therapeutic cancer vaccination, in contrast, has produced limited clinical benefit and no curative therapies. The E6 and E7 oncoproteins of human papilloma virus (HPV) drive the majority of genital cancers, and many oropharyngeal tumors. We discovered 15-19 amino acid peptides from HPV-16 E6/E7 for which induction of T-cell immunity correlates with disease-free survival in patients treated for high-grade cervical neoplasia. We report here that intranasal vaccination with these peptides and the adjuvant alpha-galactosylceramide elicits systemic and mucosal T-cell responses leading to reduced HPV(+) TC-1 tumor growth and prolonged survival in mice. We hypothesized that the inability of these T cells to fully reject established tumors resulted from suppression in the tumor microenvironment which could be ameliorated through checkpoint modulation. Combining this E6/E7 peptide vaccine with checkpoint blockade produced only modest benefit; however, coadministration with a 4-1BB agonist antibody promoted durable regression of established genital TC-1 tumors. Relative to other therapies tested, this combination of vaccine and alpha4-1BB promoted the highest CD8(+) versus regulatory FoxP3(+) T-cell ratios, elicited 2- to 5-fold higher infiltration by E7-specific CTL, and evoked higher densities of highly cytotoxic TcEO (T cytotoxic Eomesodermin) CD8 (>70-fold) and ThEO (T helper Eomesodermin) CD4 (>17-fold) T cells. These findings have immediate clinical relevance both in terms of the direct clinical utility of the vaccine studied and in illustrating the potential of 4-1BB antibody to convert therapeutic E6/E7 vaccines already in clinical trials into curative therapies.
in vivo CD40 activation
Conde, P., et al (2015). "DC-SIGN(+) Macrophages Control the Induction of Transplantation Tolerance" Immunity 42(6): 1143-1158.
PubMed
Tissue effector cells of the monocyte lineage can differentiate into different cell types with specific cell function depending on their environment. The phenotype, developmental requirements, and functional mechanisms of immune protective macrophages that mediate the induction of transplantation tolerance remain elusive. Here, we demonstrate that costimulatory blockade favored accumulation of DC-SIGN-expressing macrophages that inhibited CD8(+) T cell immunity and promoted CD4(+)Foxp3(+) Treg cell expansion in numbers. Mechanistically, that simultaneous DC-SIGN engagement by fucosylated ligands and TLR4 signaling was required for production of immunoregulatory IL-10 associated with prolonged allograft survival. Deletion of DC-SIGN-expressing macrophages in vivo, interfering with their CSF1-dependent development, or preventing the DC-SIGN signaling pathway abrogated tolerance. Together, the results provide new insights into the tolerogenic effects of costimulatory blockade and identify DC-SIGN(+) suppressive macrophages as crucial mediators of immunological tolerance with the concomitant therapeutic implications in the clinic.
in vivo CD40 activation
Carmi, Y., et al (2015). "Allogeneic IgG combined with dendritic cell stimuli induce antitumour T-cell immunity" Nature 521(7550): 99-104.
PubMed
Whereas cancers grow within host tissues and evade host immunity through immune-editing and immunosuppression, tumours are rarely transmissible between individuals. Much like transplanted allogeneic organs, allogeneic tumours are reliably rejected by host T cells, even when the tumour and host share the same major histocompatibility complex alleles, the most potent determinants of transplant rejection. How such tumour-eradicating immunity is initiated remains unknown, although elucidating this process could provide the basis for inducing similar responses against naturally arising tumours. Here we find that allogeneic tumour rejection is initiated in mice by naturally occurring tumour-binding IgG antibodies, which enable dendritic cells (DCs) to internalize tumour antigens and subsequently activate tumour-reactive T cells. We exploited this mechanism to treat autologous and autochthonous tumours successfully. Either systemic administration of DCs loaded with allogeneic-IgG-coated tumour cells or intratumoral injection of allogeneic IgG in combination with DC stimuli induced potent T-cell-mediated antitumour immune responses, resulting in tumour eradication in mouse models of melanoma, pancreas, lung and breast cancer. Moreover, this strategy led to eradication of distant tumours and metastases, as well as the injected primary tumours. To assess the clinical relevance of these findings, we studied antibodies and cells from patients with lung cancer. T cells from these patients responded vigorously to autologous tumour antigens after culture with allogeneic-IgG-loaded DCs, recapitulating our findings in mice. These results reveal that tumour-binding allogeneic IgG can induce powerful antitumour immunity that can be exploited for cancer immunotherapy.
in vitro B cell stimulation/activation
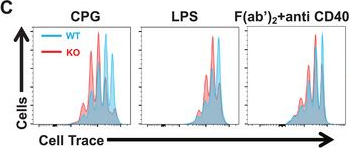
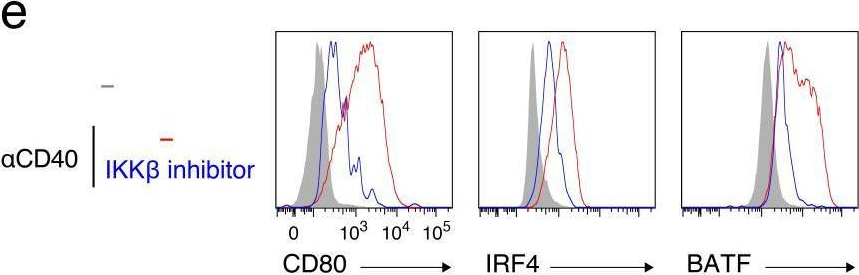
Xu, H., et al (2015). "Regulation of bifurcating B cell trajectories by mutual antagonism between transcription factors IRF4 and IRF8" Nat Immunol .
PubMed
Upon recognition of antigen, B cells undertake a bifurcated response in which some cells rapidly differentiate into plasmablasts while others undergo affinity maturation in germinal centers (GCs). Here we identified a double-negative feedback loop between the transcription factors IRF4 and IRF8 that regulated the initial developmental bifurcation of activated B cells as well as the GC response. IRF8 dampened signaling via the B cell antigen receptor (BCR), facilitated antigen-specific interaction with helper T cells, and promoted antibody affinity maturation while antagonizing IRF4-driven differentiation of plasmablasts. Genomic analysis revealed concentration-dependent actions of IRF4 and IRF8 in regulating distinct gene-expression programs. Stochastic modeling suggested that the double-negative feedback was sufficient to initiate bifurcation of the B cell developmental trajectories.
in vitro B cell stimulation/activation
Muppidi, J. R., et al (2014). "Loss of signalling via Galpha13 in germinal centre B-cell-derived lymphoma" Nature 516(7530): 254-258.
PubMed
Germinal centre B-cell-like diffuse large B-cell lymphoma (GCB-DLBCL) is a common malignancy, yet the signalling pathways that are deregulated and the factors leading to its systemic dissemination are poorly defined. Work in mice showed that sphingosine-1-phosphate receptor-2 (S1PR2), a Galpha12 and Galpha13 coupled receptor, promotes growth regulation and local confinement of germinal centre B cells. Recent deep sequencing studies of GCB-DLBCL have revealed mutations in many genes in this cancer, including in GNA13 (encoding Galpha13) and S1PR2 (refs 5,6, 7). Here we show, using in vitro and in vivo assays, that GCB-DLBCL-associated mutations occurring in S1PR2 frequently disrupt the receptor’s Akt and migration inhibitory functions. Galpha13-deficient mouse germinal centre B cells and human GCB-DLBCL cells were unable to suppress pAkt and migration in response to S1P, and Galpha13-deficient mice developed germinal centre B-cell-derived lymphoma. Germinal centre B cells, unlike most lymphocytes, are tightly confined in lymphoid organs and do not recirculate. Remarkably, deficiency in Galpha13, but not S1PR2, led to germinal centre B-cell dissemination into lymph and blood. GCB-DLBCL cell lines frequently carried mutations in the Galpha13 effector ARHGEF1, and Arhgef1 deficiency also led to germinal centre B-cell dissemination. The incomplete phenocopy of Galpha13- and S1PR2 deficiency led us to discover that P2RY8, an orphan receptor that is mutated in GCB-DLBCL and another germinal centre B-cell-derived malignancy, Burkitt’s lymphoma, also represses germinal centre B-cell growth and promotes confinement via Galpha13. These findings identify a Galpha13-dependent pathway that exerts dual actions in suppressing growth and blocking dissemination of germinal centre B cells that is frequently disrupted in germinal centre B-cell-derived lymphoma.
in vivo CD40 activation
Rabenstein, H., et al (2014). "Differential kinetics of antigen dependency of CD4+ and CD8+ T cells" J Immunol 192(8): 3507-3517.
PubMed
Ag recognition via the TCR is necessary for the expansion of specific T cells that then contribute to adaptive immunity as effector and memory cells. Because CD4+ and CD8+ T cells differ in terms of their priming APCs and MHC ligands we compared their requirements of Ag persistence during their expansion phase side by side. Proliferation and effector differentiation of TCR transgenic and polyclonal mouse T cells were thus analyzed after transient and continuous TCR signals. Following equally strong stimulation, CD4+ T cell proliferation depended on prolonged Ag presence, whereas CD8+ T cells were able to divide and differentiate into effector cells despite discontinued Ag presentation. CD4+ T cell proliferation was neither affected by Th lineage or memory differentiation nor blocked by coinhibitory signals or missing inflammatory stimuli. Continued CD8+ T cell proliferation was truly independent of self-peptide/MHC-derived signals. The subset divergence was also illustrated by surprisingly broad transcriptional differences supporting a stronger propensity of CD8+ T cells to programmed expansion. These T cell data indicate an intrinsic difference between CD4+ and CD8+ T cells regarding the processing of TCR signals for proliferation. We also found that the presentation of a MHC class II-restricted peptide is more efficiently prolonged by dendritic cell activation in vivo than a class I bound one. In summary, our data demonstrate that CD4+ T cells require continuous stimulation for clonal expansion, whereas CD8+ T cells can divide following a much shorter TCR signal.
in vivo CD40 activation
Erickson, J. J., et al (2014). "Programmed death-1 impairs secondary effector lung CD8(+) T cells during respiratory virus reinfection" J Immunol 193(10): 5108-5117.
PubMed
Reinfections with respiratory viruses are common and cause significant clinical illness, yet precise mechanisms governing this susceptibility are ill defined. Lung Ag-specific CD8(+) T cells (T(CD8)) are impaired during acute viral lower respiratory infection by the inhibitory receptor programmed death-1 (PD-1). To determine whether PD-1 contributes to recurrent infection, we first established a model of reinfection by challenging B cell-deficient mice with human metapneumovirus (HMPV) several weeks after primary infection, and found that HMPV replicated to high titers in the lungs. A robust secondary effector lung TCD8 response was generated during reinfection, but these cells were more impaired and more highly expressed the inhibitory receptors PD-1, LAG-3, and 2B4 than primary T(CD8). In vitro blockade demonstrated that PD-1 was the dominant inhibitory receptor early after reinfection. In vivo therapeutic PD-1 blockade during HMPV reinfection restored lung T(CD8) effector functions (i.e., degranulation and cytokine production) and enhanced viral clearance. PD-1 also limited the protective efficacy of HMPV epitope-specific peptide vaccination and impaired lung T(CD8) during heterotypic influenza virus challenge infection. Our results indicate that PD-1 signaling may contribute to respiratory virus reinfection and evasion of vaccine-elicited immune responses. These results have important implications for the design of effective vaccines against respiratory viruses.
in vivo CD40 activation
Hailemichael, Y., et al (2013). "Persistent antigen at vaccination sites induces tumor-specific CD8(+) T cell sequestration, dysfunction and deletion" Nat Med 19(4): 465-472.
PubMed
To understand why cancer vaccine-induced T cells often do not eradicate tumors, we studied immune responses in mice vaccinated with gp100 melanoma peptide in incomplete Freund’s adjuvant (peptide/IFA), which is commonly used in clinical cancer vaccine trials. Peptide/IFA vaccination primed tumor-specific CD8(+) T cells, which accumulated not in tumors but rather at the persisting, antigen-rich vaccination site. Once there, primed T cells became dysfunctional and underwent antigen-driven, interferon-gamma (IFN-gamma)- and Fas ligand (FasL)-mediated apoptosis, resulting in hyporesponsiveness to subsequent vaccination. Provision of CD40-specific antibody, Toll-like receptor 7 (TLR7) agonist and interleukin-2 (IL-2) reduced T cell apoptosis but did not prevent vaccination-site sequestration. A nonpersisting vaccine formulation shifted T cell localization toward tumors, inducing superior antitumor activity while reducing systemic T cell dysfunction and promoting memory formation. These data show that persisting vaccine depots can induce specific T cell sequestration, dysfunction and deletion at vaccination sites; short-lived formulations may overcome these limitations and result in greater therapeutic efficacy of peptide-based cancer vaccines.
in vivo CD40 activation
Kurche, J. S., et al (2012). "Type I IFN-dependent T cell activation is mediated by IFN-dependent dendritic cell OX40 ligand expression and is independent of T cell IFNR expression" J Immunol 188(2): 585-593.
PubMed
Type I IFNs are important for direct control of viral infection and generation of adaptive immune responses. Recently, direct stimulation of CD4(+) T cells via type I IFNR has been shown to be necessary for the formation of functional CD4(+) T cell responses. In contrast, we find that CD4(+) T cells do not require intrinsic type I IFN signals in response to combined TLR/anti-CD40 vaccination. Rather, the CD4 response is dependent on the expression of type I IFNR (IFNalphaR) on innate cells. Further, we find that dendritic cell (DC) expression of the TNF superfamily member OX40 ligand was dependent on type I IFN signaling in the DC, resulting in a reduced CD4(+) T cell response that could be substantially rescued by an agonistic Ab to the receptor OX40. Taken together, we show that the IFNalphaR dependence of the CD4(+) T cell response is accounted for exclusively by defects in DC activation.
in vivo CD40 activation
Locatelli, G., et al (2012). "Primary oligodendrocyte death does not elicit anti-CNS immunity" Nat Neurosci 15(4): 543-550.
PubMed
Anti-myelin immunity is commonly thought to drive multiple sclerosis, yet the initial trigger of this autoreactivity remains elusive. One of the proposed factors for initiating this disease is the primary death of oligodendrocytes. To specifically test such oligodendrocyte death as a trigger for anti-CNS immunity, we inducibly killed oligodendrocytes in an in vivo mouse model. Strong microglia-macrophage activation followed oligodendrocyte death, and myelin components in draining lymph nodes made CNS antigens available to lymphocytes. However, even conditions favoring autoimmunity-bystander activation, removal of regulatory T cells, presence of myelin-reactive T cells and application of demyelinating antibodies-did not result in the development of CNS inflammation after oligodendrocyte death. In addition, this lack of reactivity was not mediated by enhanced myelin-specific tolerance. Thus, in contrast with previously reported impairments of oligodendrocyte physiology, diffuse oligodendrocyte death alone or in conjunction with immune activation does not trigger anti-CNS immunity.
Product Citations
-
AhR Activation Transcriptionally Induces Anti-Microbial Peptide Alpha-Defensin 1 Leading to Reversal of Gut Microbiota Dysbiosis and Colitis.
In Gut Microbes on 1 December 2025 by Palrasu, M., Kakar, K., et al.
PubMed
Alpha-defensin 1 is a small antimicrobial peptide that acts as the first line of defense against pathogens. It is induced following microbial cues and inflammatory signals in neutrophils and Paneth cells in the small intestine, which suggests that it plays a role in microbial homeostasis in the gut. The gut microbial products also serve as ligands for the aryl hydrocarbon receptor (AhR), an environmental sensor. In the current study, we investigated if there is any crosstalk between AhR and alpha-defensin 1. Interestingly, we found a positive correlation between AhR and alpha-defensin 1 protein levels in ileal tissues from active Crohn's' (CD) patients and epithelial cells (IECs) from multiple models of murine colitis. In vitro downregulation of AhR led to inhibition of α-defensin 1, while activation of AhR induced α-defensin 1 in IECs. AhR directly targeted the dioxin response element 3 (DRE3) region on the α-defensin 1 promoter in IECs. AhR-mediated induction of α-defensin 1 in colitis mice reversed the gut microbial dysbiosis and alleviated colitis. Our data identify a novel signaling pathway in which AhR acts as a transcription factor for α-defensin 1, leading to regulation of homeostasis between gut microbiota, intestinal mucosa, and mucosal immunity.
-
-
Immunology and Microbiology
-
Cancer Research
Engineered T cells stimulate dendritic cell recruitment and antigen spreading for potent anti-tumor immunity.
In Cell Rep Med on 16 September 2025 by Xiao, Z., Wang, J., et al.
PubMed
Current T cell-based immunotherapeutic strategies show limited success in treating solid tumors due to insufficient dendritic cell (DC) activity, particularly cross-presenting conventional type 1 dendritic cells (cDC1s). DC scarcity and dysfunction hinder T cell expansion and differentiation, greatly limiting anti-tumor responses. In this study, we propose a T cell engineering strategy to enhance interaction with XCR1+ cDC1s. Adoptively transferred T cells engineered to secrete Flt3L and XCL1 (FX) promote DC trafficking and maturation and improve DC-T cell interaction, while maintaining a pool of TCF1+SlamF6+ stem-like T cells. Importantly, FX-engineered T cells trigger robust antigen spreading and potent endogenous polyclonal T cell response, enabling the recognition and elimination of tumors with heterogeneous antigens and preventing immune escape. The therapeutic efficacy of FX-armed chimeric antigen receptor (CAR)-T cells is further validated in the Flt3KO&hFLT3LG humanized mouse model. This strategy offers a promising avenue for enhancing DC-T cell interactions, paving the way for more effective immunotherapy against solid tumors.
-
-
-
Cancer Research
Targeting the CD40 costimulatory receptor to improve virotherapy efficacy in diffuse midline gliomas.
In Cell Rep Med on 15 July 2025 by Labiano, S., Marco-Sanz, J., et al.
PubMed
Diffuse midline glioma (DMG) is a devastating pediatric brain tumor. The oncolytic adenovirus Delta-24-RGD has shown promising efficacy and safety in DMG patients but is not yet curative. Thus, we hypothesized that activating dendritic cells (DCs) through the CD40 costimulatory receptor could increase antigen presentation and enhance the anti-tumor effect of the virus, resulting in long-term responses. This study shows that the intratumoral co-administration of Delta-24-RGD and a CD40 agonistic antibody is well tolerated and induces long-term anti-tumor immunity, including complete responses (up to 40%) in DMG preclinical models. Mechanistic studies revealed that this therapy increased tumor-proliferating T lymphocytes and proinflammatory myeloid cells, including mature DCs with superior tumor antigen uptake capacity. Moreover, the lack of cross-presenting DCs and the prevention of DC recruitment into the tumor abolish the Delta-24-RGD+anti-CD40 anti-DMG effect. This approach shows potential for combining virotherapy with activating antigen-presenting cells in these challenging tumors.
-
-
-
Immunology and Microbiology
Inflammatory arthritis immune related adverse events represent a unique autoimmune disease entity primarily driven by T cells, but likely not autoantibodies
In medRxiv on 6 June 2025 by Zhu, X., Yu, Y., et al.
-
-
Lymphopoiesis is attenuated upon hepatocyte-specific deletion of the cytochrome c oxidase assembly factor Sco1.
In iScience on 18 April 2025 by Pioli, K. T., Ghosh, S., et al.
PubMed
Mutations that negatively impact mitochondrial function are highly prevalent in humans and lead to disorders with a wide spectrum of disease phenotypes, including deficiencies in immune cell development and/or function. Previous analyses of mice with a hepatocyte-specific cytochrome c oxidase (COX) deficiency revealed an unexpected peripheral blood leukopenia associated with splenic and thymic atrophy. Here, we use mice with a hepatocyte-specific deletion of the COX assembly factor Sco1 to show that metabolic defects extrinsic to the hematopoietic compartment lead to a pan-lymphopenia represented by severe losses in both B and T cells. We further demonstrate that immune defects in these mice are associated with the loss of bone marrow lymphoid progenitors common to both lineages and early signs of autoantibody-mediated autoimmunity. Our findings collectively identify hepatocyte dysfunction as a potential instigator of immunodeficiency in patients with congenital mitochondrial defects who suffer from chronic or recurrent infections.
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Antigen experience history directs distinct functional states of CD8+ CAR T cells during the antileukemia response.
In Nat Immunol on 1 January 2025 by DeGolier, K., Danis, E., et al.
PubMed
Although chimeric antigen receptor (CAR) T cells are effective against B-lineage malignancies, post-CAR relapse is common, and efficacy in other tumors is limited. These challenges may be addressed through rational manipulations to control CAR T cell function. Here we examine the impact of cognate T cell antigen experience on subsequent CD8+ CAR T cell activity. Prior antigen encounter resulted in superior effector function against leukemia expressing low target antigen density at the expense of reduced proliferative capacity and susceptibility to dysfunction at limiting CAR doses. Distinctive temporal transcriptomic and epigenetic profiles in naive-derived and memory-derived CAR T cells identified RUNX family transcription factors as potential targets to augment the function of naive-derived CD8+ CAR T cells. RUNX2 overexpression enhanced antitumor efficacy of mouse CAR T cells, dependent on prior cell state, and heightened human CAR T cell functions. Our data demonstrate that prior antigen experience of CAR T cells determines functional attributes and amenability to transcription factor-mediated functional enhancement.
-
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
PGRN Inhibits Early B-cell Activation and IgE Production Through the IFITM3-STAT1 Signaling Pathway in Asthma.
In Adv Sci (Weinh) on 1 December 2024 by Zhang, P., Ruan, C., et al.
PubMed
Progranulin (PGRN) plays a critical role in bronchial asthma and the function of various immune cells. However, the mechanisms by which PGRN influences B-cell receptor (BCR) signaling and immunoglobulin E(IgE) production are not fully understood. The study aimed to elucidate the molecular mechanisms through which PGRN affects BCR signaling, B-cell differentiation, and IgE production. A PGRN knockout mouse model, along with techniques including flow cytometry, the creation of a bone marrow chimeric mouse model, total internal reflection fluorescence (TIRF), and Western blot (WB) analysis is employed, to investigate the link between PGRN and various aspects of B-cell biology. It is discovered that the absence of PGRN in mice alters peripheral B-cell subpopulations, promotes IgE class switching in a cell-intrinsic manner, and affects B-cell subpopulations. Additionally, PGRN modulates B-cell functions by regulating BCR signaling pathways, metabolic processes, and the actin cytoskeleton during early B-cell activation. Significantly, PGRN deficiency results in diminished production of NP-specific antibodies. Moreover, it is found that PGRN inhibits B-cell activation and IgE production through the PGRN-IFITM3-STAT1 signaling pathway. The findings provide new strategies for the targeted treatment of bronchial asthma, highlighting the crucial role of PGRN in B-cell signaling and IgE production.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
TNFR2 blockade promotes antitumoral immune response in PDAC by targeting activated Treg and reducing T cell exhaustion.
In J Immunother Cancer on 19 November 2024 by Debesset, A., Pilon, C., et al.
PubMed
Pancreatic ductal adenocarcinoma (PDAC) is one of the most aggressive cancers, highly resistant to standard chemotherapy and immunotherapy. Regulatory T cells (Tregs) expressing tumor necrosis factor α receptor 2 (TNFR2) contribute to immunosuppression in PDAC. Treg infiltration correlates with poor survival and tumor progression in patients with PDAC. We hypothesized that TNFR2 inhibition using a blocking monoclonal antibody (mAb) could shift the Treg-effector T cell balance in PDAC, thus enhancing antitumoral responses.
-
-
-
Cancer Research
-
Genetics
-
Immunology and Microbiology
DNA-PK inhibition enhances neoantigen diversity and increases T cell responses to immunoresistant tumors.
In J Clin Invest on 22 October 2024 by Nielsen, A. J., Albert, G. K., et al.
PubMed
Effective antitumor T cell activity relies on the expression and MHC presentation of tumor neoantigens. Tumor cells can evade T cell detection by silencing the transcription of antigens or by altering MHC machinery, resulting in inadequate neoantigen-specific T cell activation. We identified the DNA-protein kinase inhibitor (DNA-PKi) NU7441 as a promising immunomodulator that reduced immunosuppressive proteins, while increasing MHC-I expression in a panel of human melanoma cell lines. In tumor-bearing mice, combination therapy using NU7441 and the immune adjuvants stimulator of IFN genes (STING) ligand and the CD40 agonist NU-SL40 substantially increased and diversified the neoantigen landscape, antigen-presenting machinery, and, consequently, substantially increased both the number and repertoire of neoantigen-reactive, tumor-infiltrating lymphocytes (TILs). DNA-PK inhibition or KO promoted transcription and protein expression of various neoantigens in human and mouse melanomas and induced sensitivity to immune checkpoint blockade (ICB) in resistant tumors. In patients, protein kinase, DNA-activated catalytic subunit (PRKDC) transcript levels were inversely correlated with MHC-I expression and CD8+ TILs but positively correlated with increased neoantigen loads and improved responses to ICB. These studies suggest that inhibition of DNA-PK activity can restore tumor immunogenicity by increasing neoantigen expression and presentation and broadening the neoantigen-reactive T cell population.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Intratumoral NKT cell accumulation promotes antitumor immunity in pancreatic cancer.
In Proc Natl Acad Sci U S A on 16 July 2024 by Li, J., Moresco, P., et al.
PubMed
Pancreatic ductal adenocarcinoma (PDA) is a potentially lethal disease lacking effective treatments. Its immunosuppressive tumor microenvironment (TME) allows it to evade host immunosurveillance and limits response to immunotherapy. Here, using the mouse KRT19-deficient (sgKRT19-edited) PDA model, we find that intratumoral accumulation of natural killer T (NKT) cells is required to establish an immunologically active TME. Mechanistically, intratumoral NKT cells facilitate type I interferon (IFN) production to initiate an antitumor adaptive immune response, and orchestrate the intratumoral infiltration of T cells, dendritic cells, natural killer cells, and myeloid-derived suppressor cells. At the molecular level, NKT cells promote the production of type I IFN through the interaction of their CD40L with CD40 on myeloid cells. To evaluate the therapeutic potential of these observations, we find that administration of folinic acid to mice bearing PDA increases NKT cells in the TME and improves their response to anti-PD-1 antibody treatment. In conclusion, NKT cells have an essential role in the immune response to mouse PDA and are potential targets for immunotherapy.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
rWTC-MBTA Vaccine Induces Potent Adaptive Immune Responses Against Glioblastomas via Dynamic Activation of Dendritic Cells.
In Adv Sci (Weinh) on 1 April 2024 by Wang, H., Medina, R., et al.
PubMed
Despite strides in immunotherapy, glioblastoma multiforme (GBM) remains challenging due to low inherent immunogenicity and suppressive tumor microenvironment. Converting "cold" GBMs to "hot" is crucial for immune activation and improved outcomes. This study comprehensively characterized a therapeutic vaccination strategy for preclinical GBM models. The vaccine consists of Mannan-BAM-anchored irradiated whole tumor cells, Toll-like receptor ligands [lipoteichoic acid (LTA), polyinosinic-polycytidylic acid (Poly (I:C)), and resiquimod (R-848)], and anti-CD40 agonistic antibody (rWTC-MBTA). Intracranial GBM models (GL261, SB28 cells) are used to evaluate the vaccine efficacy. A substantial number of vaccinated mice exhibited complete regression of GBM tumors in a T-cell-dependent manner, with no significant toxicity. Long-term tumor-specific immune memory is confirmed upon tumor rechallenge. In the vaccine-draining lymph nodes of the SB28 model, rWTC-MBTA vaccination triggered a major rise in conventional dendritic cell type 1 (cDC1) 12 h post-treatment, followed by an increase in conventional dendritic cell type 2 (cDC2), monocyte-derived dendritic cell (moDC), and plasmacytoid dendritic cell (pDC) on Day 5 and Day 13. Enhanced cytotoxicity of CD4+ and CD8+ T cells in vaccinated mice is verified in co-culture with tumor cells. Analyses of immunosuppressive signals (T-cell exhaustion, myeloid-derived suppressor cells (MDSC), M2 macrophages) in the GBM microenvironment suggest potential combinations with other immunotherapies for enhanced efficacy. In conclusion, the authors findings demonstrate that rWTC-MBTA induces potent and long-term adaptive immune responses against GBM.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Invasion of spontaneous germinal centers by naive B cells is rapid and persistent.
In Sci Immunol on 22 March 2024 by van den Broek, T., Oleinika, K., et al.
PubMed
In autoreactive germinal centers (GC) initiated by a single rogue B cell clone, wild-type B cells expand and give rise to clones that target other autoantigens, known as epitope spreading. The chronic, progressive nature of epitope spreading calls for early interventions to limit autoimmune pathologies, but the kinetics and molecular requirements for wild-type B cell invasion and participation in GC remain largely unknown. With parabiosis and adoptive transfer approaches in a murine model of systemic lupus erythematosus, we demonstrate that wild-type B cells join existing GCs rapidly, clonally expand, persist, and contribute to autoantibody production and diversification. The invasion of autoreactive GCs by wild-type B cells required TLR7, B cell receptor specificity, antigen presentation, and type I interferon signaling. The adoptive transfer model provides a tool for identifying early events in the breaking of B cell tolerance in autoimmunity.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
CMTM6 maintains B cell-intrinsic CD40 expression to regulate anti-tumor immunity
In bioRxiv on 10 March 2024 by Long, Y., Chen, R., et al.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
B cells orchestrate tolerance to the neuromyelitis optica autoantigen AQP4.
In Nature on 1 March 2024 by Maisam Afzali, A., Nirschl, L., et al.
PubMed
Neuromyelitis optica is a paradigmatic autoimmune disease of the central nervous system, in which the water-channel protein AQP4 is the target antigen1. The immunopathology in neuromyelitis optica is largely driven by autoantibodies to AQP42. However, the T cell response that is required for the generation of these anti-AQP4 antibodies is not well understood. Here we show that B cells endogenously express AQP4 in response to activation with anti-CD40 and IL-21 and are able to present their endogenous AQP4 to T cells with an AQP4-specific T cell receptor (TCR). A population of thymic B cells emulates a CD40-stimulated B cell transcriptome, including AQP4 (in mice and humans), and efficiently purges the thymic TCR repertoire of AQP4-reactive clones. Genetic ablation of Aqp4 in B cells rescues AQP4-specific TCRs despite sufficient expression of AQP4 in medullary thymic epithelial cells, and B-cell-conditional AQP4-deficient mice are fully competent to raise AQP4-specific antibodies in productive germinal-centre responses. Thus, the negative selection of AQP4-specific thymocytes is dependent on the expression and presentation of AQP4 by thymic B cells. As AQP4 is expressed in B cells in a CD40-dependent (but not AIRE-dependent) manner, we propose that thymic B cells might tolerize against a group of germinal-centre-associated antigens, including disease-relevant autoantigens such as AQP4.
-
-
-
Stem Cells and Developmental Biology
-
Immunology and Microbiology
-
Genetics
Memory B cell subsets have divergent developmental origins that are coupled to distinct imprinted epigenetic states.
In Nat Immunol on 1 March 2024 by Callahan, D., Smita, S., et al.
PubMed
Memory B cells (MBCs) are phenotypically and functionally diverse, but their developmental origins remain undefined. Murine MBCs can be divided into subsets by expression of CD80 and PD-L2. Upon re-immunization, CD80/PD-L2 double-negative (DN) MBCs spawn germinal center B cells (GCBCs), whereas CD80/PD-L2 double-positive (DP) MBCs generate plasmablasts but not GCBCs. Using multiple approaches, including generation of an inducible GCBC-lineage reporter mouse, we demonstrate in a T cell-dependent response that DN cells formed independently of the germinal center (GC), whereas DP cells exhibited either extrafollicular (DPEX) or GCBC (DPGC) origins. Chromatin and transcriptional profiling revealed similarity of DN cells with an early memory precursor. Reciprocally, GCBC-derived DP cells shared distinct genomic features with GCBCs, while DPEX cells had hybrid features. Upon restimulation, DPEX cells were more prone to divide, while DPGC cells differentiated toward IgG1+ plasmablasts. Thus, MBC functional diversity is generated through distinct developmental histories, which imprint characteristic epigenetic patterns onto their progeny, thereby programming them for divergent functional responses.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Clinical and molecular features of acquired resistance to immunotherapy in non-small cell lung cancer.
In Cancer Cell on 12 February 2024 by Memon, D., Schoenfeld, A. J., et al.
PubMed
Although immunotherapy with PD-(L)1 blockade is routine for lung cancer, little is known about acquired resistance. Among 1,201 patients with non-small cell lung cancer (NSCLC) treated with PD-(L)1 blockade, acquired resistance is common, occurring in >60% of initial responders. Acquired resistance shows differential expression of inflammation and interferon (IFN) signaling. Relapsed tumors can be separated by upregulated or stable expression of IFNγ response genes. Upregulation of IFNγ response genes is associated with putative routes of resistance characterized by signatures of persistent IFN signaling, immune dysfunction, and mutations in antigen presentation genes which can be recapitulated in multiple murine models of acquired resistance to PD-(L)1 blockade after in vitro IFNγ treatment. Acquired resistance to PD-(L)1 blockade in NSCLC is associated with an ongoing, but altered IFN response. The persistently inflamed, rather than excluded or deserted, tumor microenvironment of acquired resistance may inform therapeutic strategies to effectively reprogram and reverse acquired resistance.
-
-
-
Immunology and Microbiology
Secreted IgM modulates IL-10 expression in B cells.
In Nat Commun on 5 January 2024 by McGettigan, S. E., Aira, L. E., et al.
PubMed
IL-10+ B cells are critical for immune homeostasis and restraining immune responses in infection, cancer, and inflammation; however, the signals that govern IL-10+ B cell differentiation are ill-defined. Here we find that IL-10+ B cells expand in mice lacking secreted IgM ((s)IgM-/-) up to 10-fold relative to wildtype (WT) among all major B cell and regulatory B cell subsets. The IL-10+ B cell increase is polyclonal and presents within 24 hours of birth. In WT mice, sIgM is produced prenatally and limits the expansion of IL-10+ B cells. Lack of the high affinity receptor for sIgM, FcμR, in B cells translates into an intermediate IL-10+ B cell phenotype relative to WT or sIgM-/- mice. Our study thus shows that sIgM regulates IL-10 programming in B cells in part via B cell-expressed FcμR, thereby revealing a function of sIgM in regulating immune homeostasis.
-
-
-
Cancer Research
-
Immunology and Microbiology
Antigen experience history directs distinct functional states of CD8+ CAR T cells during the anti-leukemia response
In Research Square on 21 December 2023 by Fry, T., DeGolier, K., et al.
-
-
-
Cancer Research
-
Immunology and Microbiology
Cancer cell plasticity and MHC-II-mediated immune tolerance promote breast cancer metastasis to lymph nodes.
In J Exp Med on 4 September 2023 by Lei, P. J., Pereira, E. R., et al.
PubMed
Tumor-draining lymph nodes (TDLNs) are important for tumor antigen-specific T cell generation and effective anticancer immune responses. However, TDLNs are often the primary site of metastasis, causing immune suppression and worse outcomes. Through cross-species single-cell RNA-Seq analysis, we identified features defining cancer cell heterogeneity, plasticity, and immune evasion during breast cancer progression and lymph node metastasis (LNM). A subset of cancer cells in the lymph nodes exhibited elevated MHC class II (MHC-II) gene expression in both mice and humans. MHC-II+ cancer cells lacked costimulatory molecule expression, leading to regulatory T cell (Treg) expansion and fewer CD4+ effector T cells in TDLNs. Genetic knockout of MHC-II reduced LNM and Treg expansion, while overexpression of the MHC-II transactivator, Ciita, worsened LNM and caused excessive Treg expansion. These findings demonstrate that cancer cell MHC-II expression promotes metastasis and immune evasion in TDLNs.
-
-
-
Cancer Research
-
Genetics
Defining the spatial distribution of extracellular adenosine revealed a myeloid-dependent immunosuppressive microenvironment in pancreatic ductal adenocarcinoma.
In J Immunother Cancer on 1 August 2023 by Graziano, V., Dannhorn, A., et al.
PubMed
The prognosis for patients with pancreatic ductal adenocarcinoma (PDAC) remains extremely poor. It has been suggested that the adenosine pathway contributes to the ability of PDAC to evade the immune system and hence, its resistance to immuno-oncology therapies (IOT), by generating extracellular adenosine (eAdo).
-