InVivoMAb anti-mouse CD1d (CD1.1)
Product Description
Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | CD1.1-transfected rat cell line RBL-CD1.1 followed by CD1.1-transfected human cell line CR1-CD1.1 |
| Reported Applications |
iNKT cell neutralization in vivo CD1d blockade Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10949293 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
iNKT cell neutralization
Pilones, K. A., et al (2014). "Invariant natural killer T cells regulate anti-tumor immunity by controlling the population of dendritic cells in tumor and draining lymph nodes" J Immunother Cancer 2(1): 37.
PubMed
BACKGROUND: Invariant natural killer T (iNKT) cells are CD1d-restricted T cells, which respond rapidly to antigen recognition and promote development of anti-tumor immunity in many tumor models. Surprisingly, we previously found that mice deficient in iNKT cells developed spontaneous CD8(+) T cells responses partially effective at inhibiting metastases in mice bearing the 4T1 mammary carcinoma, and showed a markedly improved response to treatment with local radiotherapy and anti-CTLA-4 antibody compared to wild type (WT) mice. METHODS: To understand the mechanisms of the immunosuppressive function of iNKT cells, dendritic cells (DCs) were analyzed by immunohistochemistry and flow cytometry in WT and iNKT-deficient (iNKT(-/-)) mice. The effects of antibody-mediated blockade of CD1d on DC number and phenotype, priming of anti-tumor T cells, and tumor response to treatment with local radiotherapy and anti-CTLA-4 antibody were evaluated. To determine if the improved response to treatment in the absence of iNKT cells was independent from the immunotherapy employed, 4T1-tumor bearing WT and iNKT(-/-) mice were treated with local radiotherapy in combination with antibody-mediated CD137 co-stimulation. RESULTS: DCs in 4T1 tumors and tumor-draining lymph nodes but not distant lymph nodes were significantly reduced in WT mice compared to iNKT(-/-) mice (p < 0.05), suggesting the selective elimination of DCs cross-presenting tumor-associated antigens by iNKT cells. Consistently, priming of T cells to a tumor-specific CD8 T cell epitope in mice treated with radiotherapy and anti-CTLA-4 or anti-CD137 was markedly enhanced in iNKT(-/-) compared to WT mice. CD1d blockade restored the number of DC in WT mice, improved T cell priming in draining lymph nodes and significantly enhanced response to treatment. CONCLUSIONS: Here we describe a novel mechanism of tumor immune escape mediated by iNKT cells that limit priming of anti-tumor T cells by controlling DC in tumors and draining lymph nodes. These results have important implications for the design of immunotherapies targeting iNKT cells.
iNKT cell neutralization
Hayworth, J. L., et al (2012). "CD1d-independent activation of mouse and human iNKT cells by bacterial superantigens" Immunol Cell Biol 90(7): 699-709.
PubMed
Invariant NKT (iNKT) cells are infrequent but important immunomodulatory lymphocytes that exhibit CD1d-restricted reactivity with glycolipid Ags. iNKT cells express a unique T-cell receptor (TCR) composed of an invariant alpha-chain, paired with a limited range of beta-chains. Superantigens (SAgs) are microbial toxins defined by their ability to activate conventional T cells in a TCR beta-chain variable domain (Vbeta)-specific manner. However, whether iNKT cells are directly activated by bacterial SAgs remains an open question. Herein, we explored the responsiveness of mouse and human iNKT cells to a panel of staphylococcal and streptococcal SAgs and examined the contribution of major histocompatibility complex (MHC) class II and CD1d to these responses. Bacterial SAgs that target mouse Vbeta8, such as staphylococcal enterotoxin B (SEB), were able to activate mouse hybridoma and primary hepatic iNKT cells in the presence of mouse APCs expressing human leukocyte antigen (HLA)-DR4. iNKT cell-mediated cytokine secretion in SEB-challenged HLA-DR4-transgenic mice was CD1d-independent and accompanied by a high interferon-gamma:interleukin-4 ratio consistent with an in vivo Th1 bias. Furthermore, iNKT cells from SEB-injected HLA-DR4-transgenic mice, and iNKT cells from SEB-treated human PBMCs, showed early activation by intracellular cytokine staining and CD69 expression. Unlike iNKT cell stimulation by alpha-galactosylceramide, stimulation by SEB did not induce TCR downregulation of either mouse or human iNKT cells. We conclude that Vbeta8-targeting bacterial SAgs can activate iNKT cells by utilizing a novel pathway that requires MHC class II interactions, but not CD1d. Therefore, iNKT cells fulfill important effector functions in response to bacterial SAgs and may provide attractive targets in the management of SAg-induced illnesses.
iNKT cell neutralization
Flow Cytometry
Yang, W., et al (2011). "NKT cell exacerbation of liver metastases arising from melanomas transplanted into either the eyes or spleens of mice" Invest Ophthalmol Vis Sci 52(6): 3094-3102.
PubMed
PURPOSE: To explore the role of natural killer T (NKT) cells in the development of liver metastases in mice harboring intraocular melanomas. METHODS: Cells derived from the cutaneous B16 melanoma cell line (B16LS9) were transplanted either into the vitreous body or under the spleen capsules of wild-type C57BL/6 mice and NKT-cell-deficient Jalpha18(-/-) and CD1d(-/-) mice. The development of liver metastases was evaluated by histopathology. The effect of NK cells on liver metastases was determined by selective depletion with anti-asialo-GM1 antiserum in vivo and NK-cell-mediated cytolysis of B16LS9 melanoma cells in vitro. The role of IL-10 and transforming growth factor (TGF)-beta in the inhibition of liver NK resistance to liver metastases was determined by in vivo and in vitro neutralization with monoclonal antibodies. RESULTS: Liver NKT cells, especially type I NKT cells, enhanced liver metastases arising from intraocular melanomas. NKT-cell-deficient mice developed significantly fewer liver metastases that were NK-cell dependent. Tumor-induced liver NKT cells, especially type I NKT cells, inhibited liver NK-cell cytotoxicity by an IL-10-dependent process. CONCLUSIONS: NKT cells exert protective effects in many murine tumor models. However, the present results reveal that NKT cells exacerbate liver metastases arising from intraocular melanomas. To the authors’ knowledge, this is the first report that liver NKT cells, especially type I NKT cells, inhibit liver NK-cell antimetastatic activity by the production of IL-10. These results suggest that hepatic NKT cell activity can have an important effect in the immune surveillance of liver metastases.
iNKT cell neutralization
Flow Cytometry
Miellot-Gafsou, A., et al (2010). "Early activation of invariant natural killer T cells in a rheumatoid arthritis model and application to disease treatment" Immunology 130(2): 296-306.
PubMed
Invariant NKT (iNKT) cells are a distinctive subtype of CD1d-restricted T cells involved in regulating autoimmunity and capable of producing various T helper type 1 (Th1), Th2 and Th17 cytokines. Activation of iNKT cells by their exogenous ligand alpha-galactosylceramide (alpha-GalCer) exerts therapeutic effects in autoimmune diseases such as rheumatoid arthritis (RA). However, the pathophysiological role of iNKT cells in RA, in the absence of exogenous stimulation, is incompletely understood. We investigated the potential pathophysiological effects of iNKT cells in mice with collagen-induced arthritis (CIA), a model of RA. We found that iNKT cells underwent activation only in the early phases of the disease (6 days post-induction). In the liver, but not the spleen or lymph nodes, this early activation led to the release of interleukins -4, -17A and -10 and of interferon-gamma; and an increased CD69 expression. Importantly, clinical and histological signs of arthritis were improved by the functional blockade of iNKT cells by a monoclonal antibody to CD1d at the early phase of the disease. This improvement was associated on day 6 post-induction with decreased expression of co-stimulatory molecules (CD80, CD86, CD40) on splenic dendritic cells and macrophages, whereas regulatory T-cell suppressive effects and proportions were not modified. Taken in concert, these findings suggest that iNKT cells are activated early in the course of CIA and contribute to the pathogenesis of arthritis. Therefore, iNKT-cell activation may be a valid treatment target in RA.
in vivo CD1d blockade
Shi, M. Q., et al (2006). "Experimental African trypanosomiasis: lack of effective CD1d-restricted antigen presentation" Parasite Immunol 28(12): 643-647.
PubMed
BALB/c mice are highly susceptible to African trypanosomiasis, whereas C57BL/6 mice are relatively resistant. Other investigators have reported that the synthesis of IgG antibodies to purified membrane form of variant surface glycoprotein (mfVSG) of Trypanosoma brucei is CD1 restricted. In this study, we examine the role of the CD1d/NKT cell pathway in susceptibility and resistance of mice to infection by African trypanosomes. Administration of anti-CD1d antibodies to Trypanosoma congolense-infected BALB/c mice neither affects the parasitemia nor the survival time. Correspondingly, CD1d(-/-) and CD1d(+/+) BALB/c mice infected with T. congolense or T. brucei show no differences in either parasitaemia or survival time. The course of disease in relative resistant C57BL/6 mice infected with T. congolense is also not affected by the absence of CD1d. Parasitaemia, survival time, and plasma levels of IgG2a and IgG3 parasite-specific antibodies in infected CD1d(-/-) C57BL/6 are not different from those of infected CD1d(+/+) C57BL/6 mice. We conclude that CD1d-restricted immune responses do not play an important role in susceptibility/resistance of mice infected with virulent African trypanosomes. We speculate that virulent trypanosomes have an evasion mechanism that prevents the induction of a parasite-specific, CD1d-restricted immune response by the host.
in vivo CD1d blockade
D’Souza, C. D., et al (2000). "A novel nonclassic beta2-microglobulin-restricted mechanism influencing early lymphocyte accumulation and subsequent resistance to tuberculosis in the lung" Am J Respir Cell Mol Biol 23(2): 188-193.
PubMed
In this study, we compared the course of a low-dose aerosol Mycobacterium tuberculosis infection in mice bearing gene disruptions for the beta2-microglobulin molecule, the CD8 molecule, and the CD1 molecule. Over the first 50 d of infection, the CD8- and CD1-disrupted mice were no more susceptible to infection than were the control mice. In contrast, the bacterial load in beta2-microglobulin gene-disrupted mice increased rapidly and attained much higher levels than that observed in the other gene-disrupted mice and in control mice. A second major difference between the beta2-microglobulin gene-disrupted mice and the other animals was the development of lung granulomas; both the CD8- and CD1-disrupted mice developed essentially normal granulomas except for an apparent increased lymphocyte influx in the CD8-disrupted mice. The beta2-microglobulin gene-disrupted mice, on the other hand, developed granulomas virtually devoid of lymphocytes, with these cells instead localized within prominent perivascular cuffing adjacent to the lesions. These data support the hypothesis that a beta2-microglobulin-dependent, non-CD8- and non-CD1-dependent mechanism controls the early and efficient influx of protective lymphocytes into infected lesions, and that the absence of this mechanism decreases the capacity of the animal to initially deal with pulmonary tuberculosis.
in vivo CD1d blockade
Flow Cytometry
Szalay, G., et al (1999). "Cutting edge: anti-CD1 monoclonal antibody treatment reverses the production patterns of TGF-beta 2 and Th1 cytokines and ameliorates listeriosis in mice" J Immunol 162(12): 6955-6958.
PubMed
Protection against intracellular bacteria by T cells is regulated by Ag-presenting molecules, which comprise classical MHC class I molecules, MHC class II molecules, and nonclassical MHC class Ib molecules. The role of CD1 molecules, which are structurally similar to classical MHC class I gene products, but less polymorphic, is not understood so far. We show that CD1 surface expression increased on APC in Listeria-infected mice. The in vivo treatment with anti-CD1 mAb reduced TGF-beta 2 levels and concomitantly increased secretion of the proinflammatory cytokine TNF, the Th1 cell promoting cytokine IL-12, and the Th1 cell cytokine IFN-gamma at the onset of listerial infection. These findings point to a regulatory role of CD1-reactive cells in the immune response against listeriosis.
Product Citations
-
-
Cancer Research
Hepatic iNKT cells facilitate colorectal cancer metastasis by inducing a fibrotic niche in the liver.
In iScience on 16 May 2025 by Nater, M., Brügger, M., et al.
PubMed
The liver is an important metastatic organ that contains many innate immune cells, yet little is known about their role in anti-metastatic defense. We investigated how invariant natural killer T (iNKT) cells influence colorectal cancer-derived liver metastasis using different models in immunocompetent mice. We found that hepatic iNKT cells promote metastasis by creating a supportive niche for disseminated cancer cells. Mechanistically, iNKT cells respond to disseminating cancer cells by producing the fibrogenic cytokines interleukin-4 (IL-4) and IL-13 in a T cell receptor-independent manner. Selective abrogation of IL-4 and IL-13 sensing in hepatic stellate cells prevented their transdifferentiation into extracellular matrix-producing myofibroblasts, which hindered metastatic outgrowth of disseminated cancer cells. This study highlights a novel tumor-promoting axis driven by iNKT cells in the initial stages of metastasis.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
-
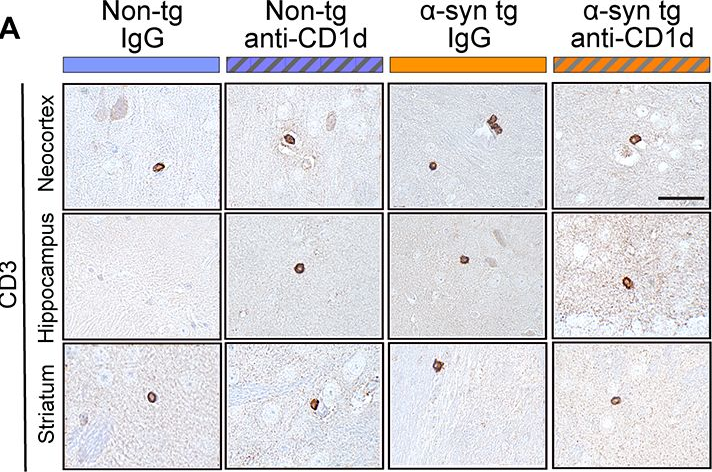
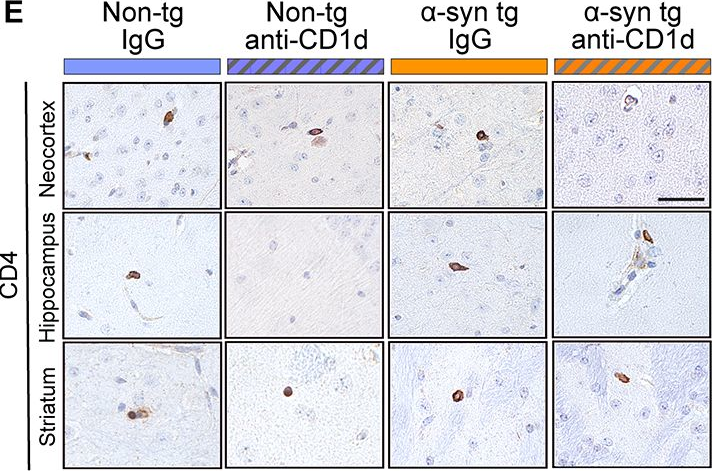
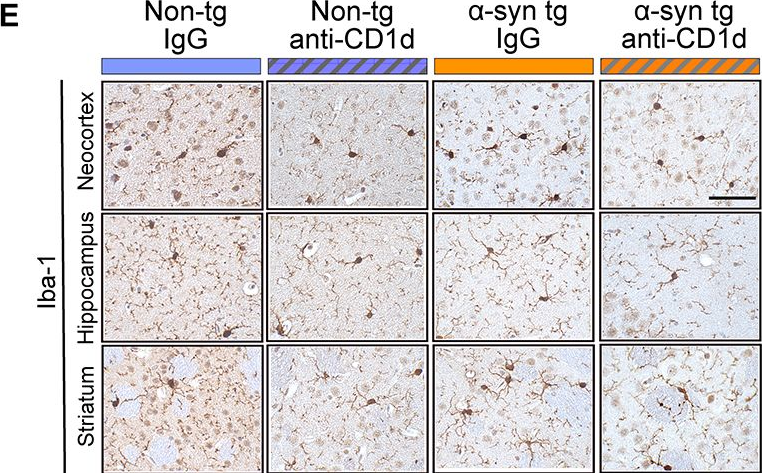
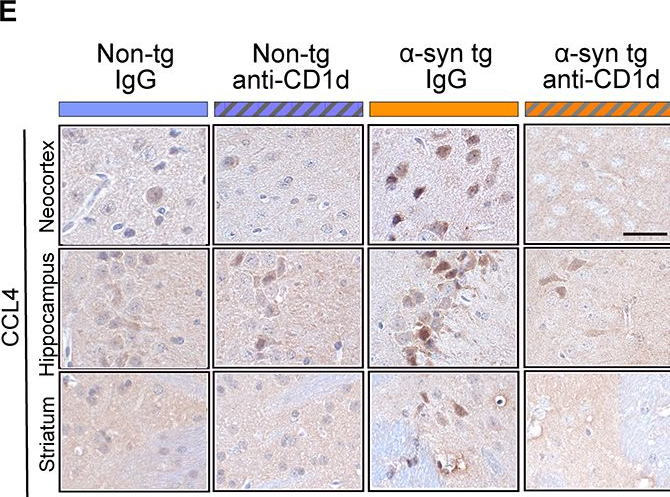
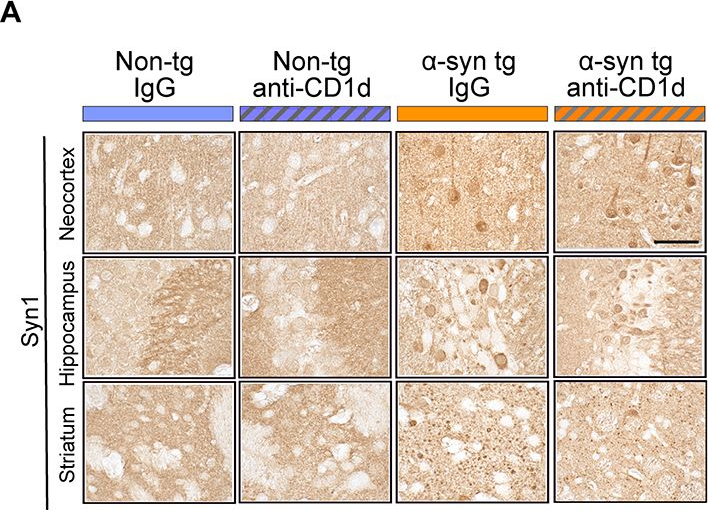
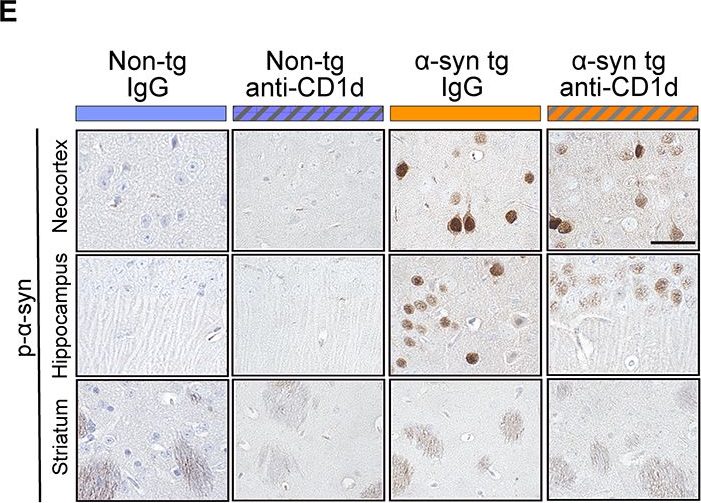
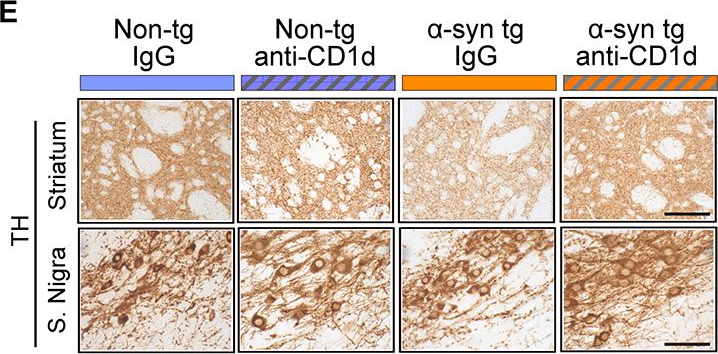
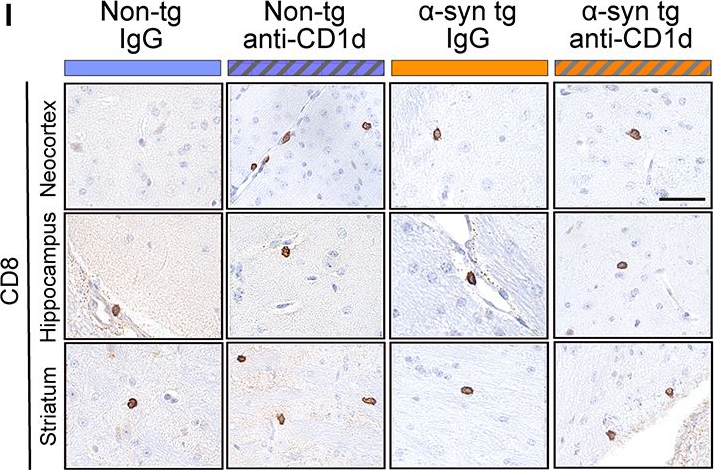
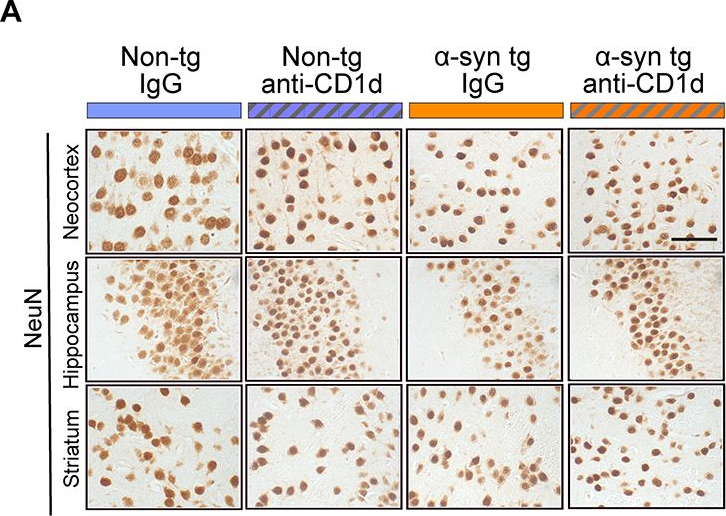
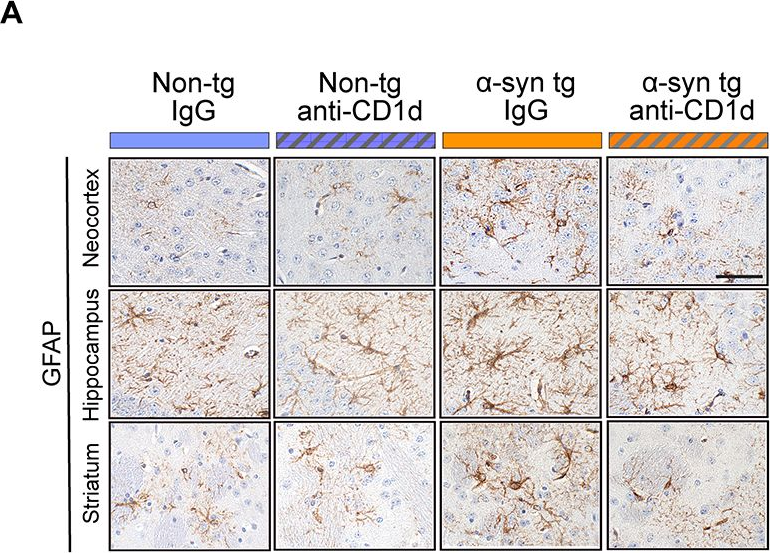
Immunotherapy with an antibody against CD1d modulates neuroinflammation in an α-synuclein transgenic model of Lewy body like disease.
In J Neuroinflammation on 15 April 2024 by Iba, M., Kwon, S., et al.
PubMed
The neuroinflammatory process in synucleinopathies of the aging population such as Parkinson's disease (PD) and dementia with Lewy bodies (DLB) involves microglial activation as well as infiltration of the CNS by T cells and natural killer T cells (NKTs). To evaluate the potential of targeting NKT cells to modulate neuroinflammation, we treated α-syn transgenic (tg) mice (e.g.: Thy1 promoter line 61) with an antibody against CD1d, which is a glycoprotein expressed in antigen presenting cells (APCs). CD1d-presented lipid antigens activate NKT cells through the interaction with T cell receptor in NKTs, resulting in the production of cytokines. Thus, we hypothesized that blocking the APC-NKT interaction with an anti-CD1d antibody might reduce neuroinflammation and neurodegeneration in models of DLB/PD. Treatment with the anti-CD1d antibody did not have effects on CD3 (T cells), slightly decreased CD4 and increased CD8 lymphocytes in the mice. Moreover, double labeling studies showed that compared to control (IgG) treated α-syn tg mice, treatment with anti-CD1d decreased numbers of CD3/interferon γ (IFN γ)-positive cells, consistent with NKTs. Further double labeling studies showed that CD1d-positive cells co-localized with the astrocytes marker GFAP and that anti-CD1d antibody reduced this effect. While in control α-syn tg mice CD3 positive cells were near astrocytes, this was modified by the treatment with the CD1d antibody. By qPCR, levels of IFN γ, CCL4, and interleukin-6 were increased in the IgG treated α-syn tg mice. Treatment with CD1d antibody blunted this cytokine response that was associated with reduced astrocytosis and microgliosis in the CNS of the α-syn tg mice treated with CD1d antibody. Flow cytometric analysis of immune cells in α-syn tg mice revealed that CD1d-tet + T cells were also increased in the spleen of α-syn tg mice, which treatment with the CD1d antibody reduced. Reduced neuroinflammation in the anti-CD1d-treated α-syn tg mice was associated with amelioration of neurodegenerative pathology. These results suggest that reducing infiltration of NKT cells with an antibody against CD1d might be a potential therapeutical approach for DLB/PD.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
-
Genetics
-
DNA hypomethylation silences anti-tumor immune genes in early prostate cancer and CTCs.
In Cell on 22 June 2023 by Guo, H., Vuille, J. A., et al.
PubMed
Cancer is characterized by hypomethylation-associated silencing of large chromatin domains, whose contribution to tumorigenesis is uncertain. Through high-resolution genome-wide single-cell DNA methylation sequencing, we identify 40 core domains that are uniformly hypomethylated from the earliest detectable stages of prostate malignancy through metastatic circulating tumor cells (CTCs). Nested among these repressive domains are smaller loci with preserved methylation that escape silencing and are enriched for cell proliferation genes. Transcriptionally silenced genes within the core hypomethylated domains are enriched for immune-related genes; prominent among these is a single gene cluster harboring all five CD1 genes that present lipid antigens to NKT cells and four IFI16-related interferon-inducible genes implicated in innate immunity. The re-expression of CD1 or IFI16 murine orthologs in immuno-competent mice abrogates tumorigenesis, accompanied by the activation of anti-tumor immunity. Thus, early epigenetic changes may shape tumorigenesis, targeting co-located genes within defined chromosomal loci. Hypomethylation domains are detectable in blood specimens enriched for CTCs.
-
-
-
Immunology and Microbiology
-
Mus musculus (Mouse)
Deletion of C-C Motif Chemokine Ligand 5 Worsens Invariant Natural Killer T-Cell-Mediated Hepatitis via Compensatory Up-regulation of CXCR2-Related Chemokine Activity.
In Cell Mol Gastroenterol Hepatol on 11 January 2019 by Chen, L., Gu, J., et al.
PubMed
Chemokine-mediated immune cell recruitment plays pivotal roles in liver inflammation. C-C motif chemokine ligand 5 (CCL5) has been shown to be responsible for the recruitment of monocytes/macrophages and has been implicated in various liver diseases, including nonalcoholic fatty liver disease, fibrosis, and hepatocellular carcinoma. Previous studies have also shown that inhibition of CCL5 appears to be a promising therapeutic approach for several chronic liver diseases. However, whether blocking CCL5 could benefit immune cell-mediated hepatitis remains largely elusive.
-