InVivoMAb anti-human CD25 (IL-2Rα)
Product Description
Specifications
| Isotype | Mouse IgG2a |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb mouse IgG2a isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Human PBMCs |
| Reported Applications |
in vivo regulatory T cell depletion in humanized mice Immunoprecipitation Immunofluorescence |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
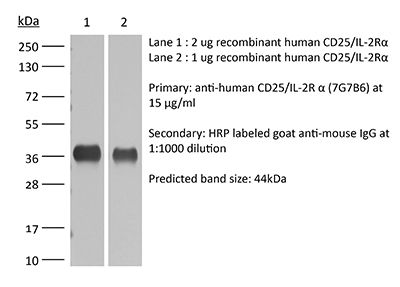
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107617 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo regulatory T cell depletion in humanized mice
Li, Y., et al (2017). "Regulatory T cells control toxicity in a humanized model of IL-2 therapy" Nat Commun 8(1): 1762.
PubMed
While patient selection and clinical management have reduced high-dose IL-2 (HDIL2) immunotherapy toxicities, the immune mechanisms that underlie HDIL2-induced morbidity remain unclear. Here we show that dose-dependent morbidity and mortality of IL-2 immunotherapy can be modeled in human immune system (HIS) mice. Depletion of human T cell subsets during the HDIL2 treatment reduces toxicity, pointing to the central function of T cells. Preferential expansion of effector T cells secondary to defective suppressive capacity of regulatory T (T(reg)) cells after HDIL2 therapy further underscores the importance of T(reg) in the maintenance of immune tolerance. IL-2 toxicity is induced by selective depletion or inhibition of T(reg) after LDIL2 therapy, and is ameliorated in HDIL2-treated HIS mice receiving the PIM-1 kinase inhibitor, Kaempferol. Modeling IL-2 pathophysiology in HIS mice offers a means to understand the functions of effector and regulatory T cells in immune-mediated toxicities associated with cancer immunotherapy.
Immunoprecipitation
Hong, X., et al (2015). "SAP97 blocks the RXR ER retention signal of NMDA receptor subunit GluN1-3 through its SH3 domain" Biochim Biophys Acta 1853(2): 489-499.
PubMed
Plakophilin-1 (PKP-1) is an armadillo family protein critical for desmosomal adhesion and epidermal integrity. In the autoimmune skin-blistering disease pemphigus vulgaris (PV), autoantibodies (IgG) target the desmosomal cadherin desmoglein 3 (Dsg3) and compromise keratinocyte cell-cell adhesion. Here, we report that enhanced expression of PKP-1 protects keratinocytes from PV IgG-induced loss of cell-cell adhesion. PKP-1 prevents loss of Dsg3 and other desmosomal proteins from cell-cell borders and prevents alterations in desmosome ultrastructure in keratinocytes treated with PV IgG. Using a series of Dsg3 chimeras and deletion constructs, we find that PKP-1 clusters Dsg3 with the desmosomal plaque protein desmoplakin in a manner dependent on the plakoglobin-binding domain of the Dsg3 tail. Furthermore, PKP-1 expression transforms desmosome adhesion from a calcium-dependent to a calcium-independent and hyperadhesive state. These results demonstrate that manipulating the expression of a single desmosomal plaque protein can block the pathogenic effects of PV IgG on keratinocyte adhesion.
Immunofluorescence
Tucker, D. K., et al (2014). "Plakophilin-1 protects keratinocytes from pemphigus vulgaris IgG by forming calcium-independent desmosomes" J Invest Dermatol 134(4): 1033-1043.
PubMed
SAP97 is directly involved in exporting NMDA receptors with a specific subunit composition from the endoplasmic reticulum (ER). Characterization of the interactions between SAP97 and an NMDA receptor splice variant, GluN1-3, and of the effects on forward trafficking revealed that an ER-level interaction blocked the RXR ER-retention motif in the GluN1-3 cytoplasmic C-terminus in the context of both reporter molecules and full-length receptors. Binding of SAP97 to the PDZ-binding domain of GluN1-3 was required, but the blockade of ER-retention was mediated by the SH3-GuK domains coupled with the action of the N-terminus of SAP97. While other domains of SAP97 were involved in forward trafficking of GluN1-3 out of the ER, the SH3 domain was necessary and sufficient to block the ER retention. This is the first direct evidence for the masking of ER-retention signals by PDZ domain-containing proteins, and provides detailed underlying mechanistic requirements. Such a mechanism could be central to modulating the ER exit of receptors into local, non-conventional or conventional, secretory pathways in neurons.
Product Citations
-
-
Cancer Research
-
Immunology and Microbiology
CD47 masks pro-phagocytic ligands in cis on tumor cells to suppress antitumor immunity.
In Nat Immunol on 1 December 2023 by Tang, Z., Zhong, M. C., et al.
PubMed
Cancer cells often overexpress CD47, which triggers the inhibitory receptor SIRPα expressed on macrophages, to elude phagocytosis and antitumor immunity. Pharmacological blockade of CD47 or SIRPα is showing promise as anticancer therapy, although CD47 blockade has been associated with hematological toxicities that may reflect its broad expression pattern on normal cells. Here we found that, in addition to triggering SIRPα, CD47 suppressed phagocytosis by a SIRPα-independent mechanism. This mechanism prevented phagocytosis initiated by the pro-phagocytic ligand, SLAMF7, on tumor cells, due to a cis interaction between CD47 and SLAMF7. The CD47-SLAMF7 interaction was disrupted by CD47 blockade and by a first-in-class agonist SLAMF7 antibody, but not by SIRPα blockade, thereby promoting antitumor immunity. Hence, CD47 suppresses phagocytosis not only by engaging SIRPα, but also by masking cell-intrinsic pro-phagocytic ligands on tumor cells and knowledge of this mechanism may influence the decision between CD47 blockade or SIRPα blockade for therapeutic purposes.
-
-
-
In vivo experiments
-
In vivo experiments
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Regulatory T cells control toxicity in a humanized model of IL-2 therapy.
In Nat Commun on 24 November 2017 by Li, Y., Strick-Marchand, H., et al.
PubMed
While patient selection and clinical management have reduced high-dose IL-2 (HDIL2) immunotherapy toxicities, the immune mechanisms that underlie HDIL2-induced morbidity remain unclear. Here we show that dose-dependent morbidity and mortality of IL-2 immunotherapy can be modeled in human immune system (HIS) mice. Depletion of human T cell subsets during the HDIL2 treatment reduces toxicity, pointing to the central function of T cells. Preferential expansion of effector T cells secondary to defective suppressive capacity of regulatory T (Treg) cells after HDIL2 therapy further underscores the importance of Treg in the maintenance of immune tolerance. IL-2 toxicity is induced by selective depletion or inhibition of Treg after LDIL2 therapy, and is ameliorated in HDIL2-treated HIS mice receiving the PIM-1 kinase inhibitor, Kaempferol. Modeling IL-2 pathophysiology in HIS mice offers a means to understand the functions of effector and regulatory T cells in immune-mediated toxicities associated with cancer immunotherapy.
-