InVivoMAb anti-mouse CD83
Product Details
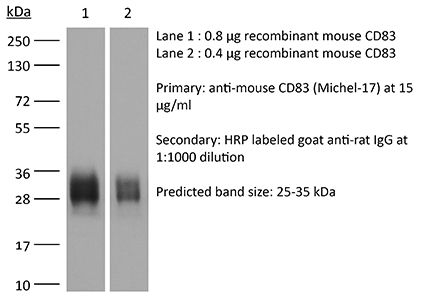
The Michel-17 monoclonal antibody reacts with mouse CD83, a 45 kDa cell surface glycoprotein and a member of the Ig superfamily. CD83 is expressed on mature dendritic cells and activated lymphocytes. CD83 is a specific maturation marker for dendritic cells and also plays a role in thymic T cell maturation as well as peripheral T cell activation. CD83 is also involved in the regulation of B cell function.Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | CD83-Ig fusion proteins |
| Reported Applications |
in vivo CD83 blockade in vitro CD83 blockade Flow cytometry ELISA |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
in vivo CD83 blockade
Kateryna Onyshchenko, Ren Luo, Xi Rao, Xuanwei Zhang, Simone Gaedicke, Anca-Ligia Grosu, Elke Firat, Gabriele Niedermann. (2024). "Hypofractionated radiotherapy combined with lenalidomide improves systemic antitumor activity in mouse solid tumor models" Theranostics 14(6):2573-2588. PubMed
Background: Hypofractionated radiotherapy (hRT) can induce a T cell-mediated abscopal effect on non-irradiated tumor lesions, especially in combination with immune checkpoint blockade (ICB). However, clinically, this effect is still rare, and ICB-mediated adverse events are common. Lenalidomide (lena) is an anti-angiogenic and immunomodulatory drug used in the treatment of hematologic malignancies. We here investigated in solid tumor models whether lena can enhance the abscopal effect in double combination with hRT. Methods: In two syngeneic bilateral tumor models (B16-CD133 melanoma and MC38 colon carcinoma), the primary tumor was treated with hRT. Lena was given daily for 3 weeks. Besides tumor size and survival, the dependence of the antitumor effects on CD8+ cells, type-I IFN signaling, and T cell costimulation was determined with depleting or blocking antibodies. Tumor-specific CD8+ T cells were quantified, and their differentiation and effector status were characterized by multicolor flow cytometry using MHC-I tetramers and various antibodies. In addition, dendritic cell (DC)-mediated tumor antigen cross-presentation in vitro and directly ex vivo and the composition of tumor-associated vascular endothelial cells were investigated. Results: In both tumor models, the hRT/lena double combination induced a significant abscopal effect. Control of the non-irradiated secondary tumor and survival were considerably better than with the respective monotherapies. The abscopal effect was strongly dependent on CD8+ cells and associated with an increase in tumor-specific CD8+ T cells in the non-irradiated tumor and its draining lymph nodes. Additionally, we found more tumor-specific T cells with a stem-like (TCF1+ TIM3- PD1+) and a transitory (TCF1- TIM3+ CD101- PD1+) exhausted phenotype and more expressing effector molecules such as GzmB, IFNγ, and TNFα. Moreover, in the non-irradiated tumor, hRT/lena treatment also increased DCs cross-presenting a tumor model antigen. Blocking type-I IFN signaling, which is essential for cross-presentation, completely abrogated the abscopal effect. A gene expression analysis of bone marrow-derived DCs revealed that lena augmented the expression of IFN response genes and genes associated with differentiation, maturation (including CD70, CD83, and CD86), migration to lymph nodes, and T cell activation. Flow cytometry confirmed an increase in CD70+ CD83+ CD86+ DCs in both irradiated and abscopal tumors. Moreover, the hRT/lena-induced abscopal effect was diminished when these costimulatory molecules were blocked simultaneously using antibodies. In line with the enhanced infiltration by DCs and tumor-specific CD8+ T cells, including more stem-like cells, hRT/lena also increased tumor-associated high endothelial cells (TA-HECs) in the non-irradiated tumor. Conclusions: We demonstrate that lena can augment the hRT-induced abscopal effect in mouse solid tumor models in a CD8 T cell- and IFN-I-dependent manner, correlating with enhanced anti-tumor CD8 T cell immunity, DC cross-presentation, and TA-HEC numbers. Our findings may be helpful for the planning of clinical trials in (oligo)metastatic patients.
Flow Cytometry
Rotem S, Bar-Haim E, Elia U, Cohen H, Lazar S, Cohen O, Chitlaru T, Gal Y. (2022). "A Novel Approach to Vaccine Development: Concomitant Pathogen Inactivation and Host Immune Stimulation by Peroxynitrite" Vaccines (Basel) 10(10):1593. PubMed
The design of efficient vaccines for long-term protective immunity against pathogens represents an objective of utmost public health priority. In general, live attenuated vaccines are considered to be more effective than inactivated pathogens, yet potentially more reactogenic. Accordingly, inactivation protocols which do not compromise the pathogen's ability to elicit protective immunity are highly beneficial. One of the sentinel mechanisms of the host innate immune system relies on the production of reactive nitrogen intermediates (RNI), which efficiently inactivate pathogens. Peroxynitrite (PN) is a prevalent RNI, assembled spontaneously upon the interaction of nitric oxide (NO) with superoxide. PN exerts its bactericidal effect by via the efficient oxidation of a broad range of biological molecules. Furthermore, the interaction of PN with proteins results in structural/chemical modifications, such as the oxidation of tryptophan, tyrosine, and cysteine residues, as well as the formation of carbonyl, dityrosine, and nitrotyrosine (NT). In addition to their role in innate immunity, these PN-mediated modifications of pathogen components may also augment the antigenicity of pathogen peptides and proteins, hence contributing to specific humoral responses. In the study reported here, a novel approach for vaccine development, consisting of pathogen inactivation by PN, combined with increased immunity of NT-containing peptides, is implemented as a proof-of-concept for vaccination against the intracellular pathogen Francisella tularensis (F. tularensis). In vivo experiments in a murine model of tularemia confirm that PN-inactivated F. tularensis formulations may rapidly stimulate innate and adaptive immune cells, conferring efficient protection against a lethal challenge, superior to that elicited by bacteria inactivated by the widely used formalin treatment.
in vitro CD83 blockade, Flow Cytometry
Carlsson JA, Wold AE, Sandberg AS, Östman SM. (2015). "The Polyunsaturated Fatty Acids Arachidonic Acid and Docosahexaenoic Acid Induce Mouse Dendritic Cells Maturation but Reduce T-Cell Responses In Vitro" PLoS One 10(11):e0143741. PubMed
Long-chain polyunsaturated fatty acids (PUFAs) might regulate T-cell activation and lineage commitment. Here, we measured the effects of omega-3 (n-3), n-6 and n-9 fatty acids on the interaction between dendritic cells (DCs) and naïve T cells. Spleen DCs from BALB/c mice were cultured in vitro with ovalbumin (OVA) with 50 μM fatty acids; α-linolenic acid, arachidonic acid (AA), eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), linoleic acid or oleic acid and thereafter OVA-specific DO11.10 T cells were added to the cultures. Fatty acids were taken up by the DCs, as shown by gas chromatography analysis. After culture with arachidonic acid or DHA CD11c+ CD11b+ and CD11c+ CD11bneg DCs expressed more CD40, CD80, CD83, CD86 and PDL-1, while IAd remained unchanged. However, fewer T cells co-cultured with these DCs proliferated (CellTrace Violet low) and expressed CD69 or CD25, while more were necrotic (7AAD+). We noted an increased proportion of T cells with a regulatory T cell (Treg) phenotype, i.e., when gating on CD4+ FoxP3+ CTLA-4+, CD4+ FoxP3+ Helios+ or CD4+ FoxP3+ PD-1+, in co-cultures with arachidonic acid- or DHA-primed DCs relative to control cultures. The proportion of putative Tregs was inversely correlated to T-cell proliferation, indicating a suppressive function of these cells. With arachidonic acid DCs produced higher levels of prostaglandin E2 while T cells produced lower amounts of IL-10 and IFNγ. In conclusion arachidonic acid and DHA induced up-regulation of activation markers on DCs. However arachidonic acid- and DHA-primed DCs reduced T-cell proliferation and increased the proportion of T cells expressing FoxP3, indicating that these fatty acids can promote induction of regulatory T cells.
ELISA
Lüthje K, Cramer SO, Ehrlich S, Veit A, Steeg C, Fleischer B, Bonin Av, Breloer M. (2006). "Transgenic expression of a CD83-immunoglobulin fusion protein impairs the development of immune-competent CD4-positive T cells" Eur J Immunol 36(8):2035-45. PubMed
The murine transmembrane glycoprotein CD83 is an important regulator for both thymic T cell maturation and peripheral T cell response. CD83 deficiency leads to a block in the thymic maturation of CD4-positive T cells, and interference with peripheral CD83/CD83 ligand interaction by addition of soluble CD83 suppresses immune responses in vivo and in vitro. Here we report the generation of a mouse transgenic for a fusion protein consisting of the extracellular domain of murine CD83 fused to the constant part of human IgG1 heavy chain. Thymic selection of CD4-positive T cells was unchanged in CD83Ig transgenic and in CD83Ig/OT-2 double-transgenic mice. However, thymic and peripheral CD4-positive T cells derived from CD83Ig/OT-2 transgenic mice displayed a reduced cytokine response to antigenic stimulation in vitro, whereas CD83Ig/OT-1-derived CD8-positive T cells showed normal cytokine secretion. The T cell defect was relevant in vivo, since a sub-lethal infection with Trypanosoma cruzi led to an increased parasitemia and reduced survival rate of CD83Ig transgenic mice compared to wild-type C57BL/6 mice. In contrast, in vivo application of recombinant CD83Ig did not result in an increase in parasitemia. Taken together our data suggest that thymic selection in the presence of CD83Ig leads to an intrinsic T cell defect of CD4-positive T cells resembling the phenotype described for CD4-positive T cells derived from CD83-deficient mouse strains.