InVivoMAb anti-mouse CD8β (Lyt 3.2)
Product Details
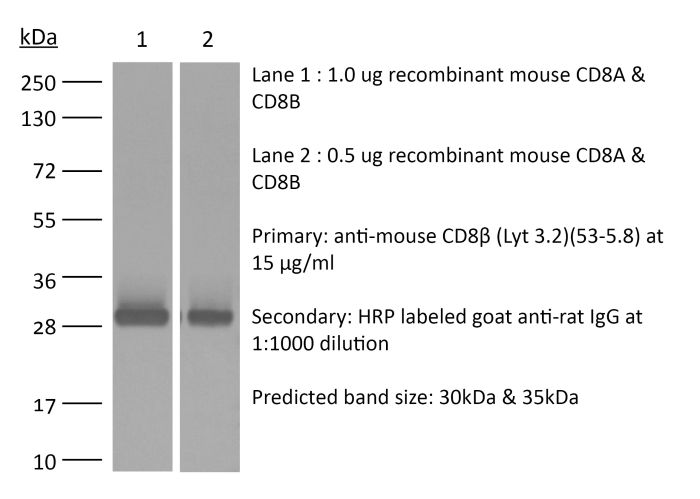
The 53-5.8 monoclonal antibody reacts with mouse CD8β also known as Lyt 3.2. The CD8 antigen is a transmembrane glycoprotein that acts as a co-receptor for the T cell receptor (TCR). Like the TCR, CD8 binds to class I MHC molecules displayed by antigen presenting cells (APC). CD8 is primarily expressed on the surface of cytotoxic T cells, but can also be found on thymocytes, natural killer cells, and some dendritic cell subsets. CD8 most commonly exists as a heterodimer composed of one CD8α and one CD8β chain however, it can also exist as a homodimer composed of two CD8α chains. Both the CD8α and CD8β chains share significant homology to immunoglobulin variable light chains. The molecular weight of each CD8 chain is approximately 34 kDa. The 53-5.8 antibody has been shown to deplete CD8+ T cells completely but not deplete CD8+ CD11c+ dendritic cells when used in vivo.Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse thymus or spleen |
| Reported Applications |
in vivo CD8+ T cell depletion in vitro CD8 blockade Immunofluorescence |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2687706 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
Immunofluorescence
Howland, S. W., et al. (2015). "Activated Brain Endothelial Cells Cross-Present Malaria Antigen" PLoS Pathog 11(6): e1004963. PubMed
In the murine model of cerebral malaria caused by P. berghei ANKA (PbA), parasite-specific CD8+ T cells directly induce pathology and have long been hypothesized to kill brain endothelial cells that have internalized PbA antigen. We previously reported that brain microvessel fragments from infected mice cross-present PbA epitopes, using reporter cells transduced with epitope-specific T cell receptors. Here, we confirm that endothelial cells are the population responsible for cross-presentation in vivo, not pericytes or microglia. PbA antigen cross-presentation by primary brain endothelial cells in vitro confers susceptibility to killing by CD8+ T cells from infected mice. IFNgamma stimulation is required for brain endothelial cross-presentation in vivo and in vitro, which occurs by a proteasome- and TAP-dependent mechanism. Parasite strains that do not induce cerebral malaria were phagocytosed and cross-presented less efficiently than PbA in vitro. The main source of antigen appears to be free merozoites, which were avidly phagocytosed. A human brain endothelial cell line also phagocytosed P. falciparum merozoites. Besides being the first demonstration of cross-presentation by brain endothelial cells, our results suggest that interfering with merozoite phagocytosis or antigen processing may be effective strategies for cerebral malaria intervention.
in vivo CD8+ T cell depletion
Guillerey, C., et al. (2015). "Immunosurveillance and therapy of multiple myeloma are CD226 dependent" J Clin Invest 125(5): 2077-2089. PubMed
Multiple myeloma (MM) is an age-dependent hematological malignancy. Evaluation of immune interactions that drive MM relies on in vitro experiments that do not reflect the complex cellular stroma involved in MM pathogenesis. Here we used Vk*MYC transgenic mice, which spontaneously develop MM, and demonstrated that the immune system plays a critical role in the control of MM progression and the response to treatment. We monitored Vk*MYC mice that had been crossed with Cd226 mutant mice over a period of 3 years and found that CD226 limits spontaneous MM development. The CD226-dependent anti-myeloma immune response against transplanted Vk*MYC MM cells was mediated both by NK and CD8+ T cells through perforin and IFN-gamma pathways. Moreover, CD226 expression was required for optimal antimyeloma efficacy of cyclophosphamide (CTX) and bortezomib (Btz), which are both standardly used to manage MM in patients. Activation of costimulatory receptor CD137 with mAb (4-1BB) exerted strong antimyeloma activity, while inhibition of coinhibitory receptors PD-1 and CTLA-4 had no effect. Taken together, the results of this study provide in vivo evidence that CD226 is important for MM immunosurveillance and indicate that specific immune components should be targeted for optimal MM treatment efficacy. As progressive immunosuppression associates with MM development, strategies aimed to increase immune functions may have important therapeutic implications in MM.
in vivo CD8+ T cell depletion
Kobayashi, T., et al. (2015). "NKT cell-targeted vaccination plus anti-4-1BB antibody generates persistent CD8 T cell immunity against B cell lymphoma" Oncoimmunology 4(3): e990793. PubMed
Harnessing the immune adjuvant properties of natural killer T (NKT) cells is an effective strategy to generate anticancer immunity. The objective of this study was to increase the potency and durability of vaccine-induced immunity against B cell lymphoma by combining alpha-galactosylceramide (alpha-GalCer)-loaded tumor cell vaccination with an agonistic antibody targeting the immune checkpoint molecule 4-1BB (CD137). We observed potent synergy when combining vaccination and anti-4-1BB antibody treatment resulting in significantly enhanced survival of mice harboring Emu-myc tumors, including complete eradication of lymphoma in over 50% of mice. Tumor-free survival required interferon gamma (IFNgamma)-dependent expansion of CD8+ T cells and was associated with 4-1BB-mediated differentiation of KLRG1+ effector CD8+ T cells. ‘Cured’ mice were also resistant to lymphoma re-challenge 80 days later indicating successful generation of immunological memory. Overall, our results demonstrate that therapeutic anticancer vaccination against B cell lymphoma using an NKT cell ligand can be boosted by subsequent co-stimulation through 4-1BB leading to a sustainable immune response that may enhance outcomes to conventional treatment.
in vivo CD8+ T cell depletion
Allard, B., et al. (2013). "Targeting CD73 enhances the antitumor activity of anti-PD-1 and anti-CTLA-4 mAbs" Clin Cancer Res 19(20): 5626-5635. PubMed
PURPOSE: Monoclonal antibodies (mAb) that block programmed death (PD)-1 or cytotoxic T lymphocyte antigen (CTLA-4) receptors have been associated with durable clinical responses against a variety of cancer types and hold great potential as novel cancer therapeutics. Recent evidence suggest that targeted blockade of multiple immunosuppressive pathways can induce synergistic antitumor responses. EXPERIMENTAL DESIGN: In this study, we investigated whether targeted blockade of CD73, an ectonucleotidase that catabolizes the hydrolysis of extracellular adenosine monophosphate (AMP) to adenosine, can enhance the antitumor activity of anti-CTLA-4 and anti-PD-1 mAbs against transplanted and chemically induced mouse tumors. RESULTS: Anti-CD73 mAb significantly enhanced the activity of both anti-CTLA-4 and anti-PD-1 mAbs against MC38-OVA (colon) and RM-1 (prostate) subcutaneous tumors, and established metastatic 4T1.2 breast cancer. Anti-CD73 mAb also significantly enhanced the activity of anti-PD-1 mAb against 3-methylcholanthrene (MCA)-induced fibrosarcomas. Gene-targeted mice revealed that single-agent therapies and combinatorial treatments were dependent on host IFN-gamma and CD8(+) T cells, but independent of perforin. Interestingly, anti-CD73 mAb preferentially synergized with anti-PD-1 mAb. We investigated the effect of extracellular adenosine on tumor-infiltrating T cells and showed that activation of A2A adenosine receptor enhances PD-1 expression, but not CTLA-4 expression, on tumor-specific CD8+ T cells and CD4+ Foxp3+ T regulatory cells. CONCLUSIONS: Taken together, our study revealed that targeted blockade of CD73 can enhance the therapeutic activity of anti-PD-1 and anti-CTLA-4 mAbs and may thus potentiate therapeutic strategies targeting immune checkpoint inhibitors in general.
in vivo CD8+ T cell depletion
Ahmed, K. A., et al. (2012). "Direct in vivo evidence of CD4+ T cell requirement for CTL response and memory via pMHC-I targeting and CD40L signaling" J Leukoc Biol 92(2): 289-300. PubMed
CD4(+) T cell help contributes critically to DC-induced CD8(+) CTL immunity. However, precisely how these three cell populations interact and how CD4(+) T cell signals are delivered to CD8(+) T cells in vivo have been unclear. In this study, we developed a novel, two-step approach, wherein CD4(+) T cells and antigen-presenting DCs productively engaged one another in vivo in the absence of cognate CD8(+) T cells, after which, we selectively depleted the previously engaged CD4(+) T cells or DCs before allowing interactions of either population alone with naive CD8(+) T cells. This protocol thus allows us to clearly document the importance of CD4(+) T-licensed DCs and DC-primed CD4(+) T cells in CTL immunity. Here, we provide direct in vivo evidence that primed CD4(+) T cells or licensed DCs can stimulate CTL response and memory, independent of DC-CD4(+) T cell clusters. Our results suggest that primed CD4(+) T cells with acquired pMHC-I from DCs represent crucial “immune intermediates” for rapid induction of CTL responses and for functional memory via CD40L signaling. Importantly, intravital, two-photon microscopy elegantly provide unequivocal in vivo evidence for direct CD4-CD8(+) T cell interactions via pMHC-I engagement. This study corroborates the coexistence of direct and indirect mechanisms of T cell help for a CTL response in noninflammatory situations. These data suggest a new “dynamic model of three-cell interactions” for CTL immunity derived from stimulation by dissociated, licensed DCs, primed CD4(+) T cells, and DC-CD4(+) T cell clusters and may have significant implications for autoimmunity and vaccine design.
in vivo CD8+ T cell depletion
Verbrugge, I., et al. (2012). "Radiotherapy increases the permissiveness of established mammary tumors to rejection by immunomodulatory antibodies" Cancer Res 72(13): 3163-3174. PubMed
It is becoming increasingly evident that radiotherapy may benefit from coincident or subsequent immunotherapy. In this study, we examined whether the antitumor effects of radiotherapy, in established triple-negative breast tumors could be enhanced with combinations of clinically relevant monoclonal antibodies (mAb), designed to stimulate immunity [anti-(alpha)-CD137, alpha-CD40] or relieve immunosuppression [alpha-programmed death (PD)-1]. While the concomitant targeting of the costimulatory molecules CD137 and CD40 enhanced the antitumor effects of radiotherapy and promoted the rejection of subcutaneous BALB/c-derived 4T1.2 tumors, this novel combination was noncurative in mice bearing established C57BL/6-derived AT-3 tumors. We identified PD-1 signaling within the AT-3 tumors as a critical limiting factor to the therapeutic efficacy of alpha-CD137 therapy, alone and in combination with radiotherapy. Strikingly, all mice bearing established orthotopic AT-3 mammary tumors were cured when alpha-CD137 and alpha-PD-1 mAbs were combined with single- or low-dose fractionated radiotherapy. CD8+ T cells were essential for curative responses to this combinatorial regime. Interestingly, CD137 expression on tumor-associated CD8+ T cells was largely restricted to a subset that highly expressed PD-1. These CD137+PD-1High CD8+ T cells, persisted in irradiated AT-3 tumors, expressed Tim-3, granzyme B and Ki67 and produced IFN-gamma ex vivo in response to phorbol 12-myristate 13-acetate (PMA) and ionomycin stimulation. Notably, radiotherapy did not deplete, but enriched tumors of functionally active, tumor-specific effector cells. Collectively, these data show that concomitant targeting of immunostimulatory and inhibitory checkpoints with immunomodulatory mAbs can enhance the curative capacity of radiotherapy in established breast malignancy.
in vitro CD8 blockade
Takada, K. and S. C. Jameson. (2009). "Self-class I MHC molecules support survival of naive CD8 T cells, but depress their functional sensitivity through regulation of CD8 expression levels" J Exp Med 206(10): 2253-2269. PubMed
Previous studies have suggested that naive CD8 T cells require self-peptide-major histocompatability complex (MHC) complexes for maintenance. However, interpretation of such studies is complicated because of the involvement of lymphopenic animals, as lymphopenia drastically alters naive T cell homeostasis and function. In this study, we explored naive CD8 T cell survival and function in nonlymphopenic conditions by using bone marrow chimeric donors and hosts in which class I MHC expression is absent or limited to radiosensitive versus radioresistant cells. We found that long-term survival of naive CD8 T cells (but not CD4 T cells) was impaired in the absence of class I MHC. However, distinct from this effect, class I MHC deprivation also enhanced naive CD8 T cell responsiveness to low-affinity (but not high-affinity) peptide-MHC ligands. We found that this improved sensitivity was a consequence of up-regulated CD8 levels, which was mediated through a transcriptional mechanism. Hence, our data suggest that, in a nonlymphopenic setting, self-class I MHC molecules support CD8 T cell survival, but that these interactions also attenuate naive T cell sensitivity by dynamic tuning of CD8 levels.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
A tetravalent nanovaccine that inhibits growth of HPV-associated head and neck carcinoma via dendritic and T cell activation.
In IScience on 19 April 2024 by Josi, R., Speiser, D. E., et al.
PubMed
The global incidence of human papillomavirus (HPV) associated head and neck carcinoma is on the rise, in response to this a tetravalent therapeutic vaccine named Qβ-HPVag was developed. This vaccine, utilizing virus-like particles (VLPs) loaded with toll-like receptor ligands and chemically coupled to four HPV16-derived peptides, demonstrated strong anti-tumor effects in a murine head and neck cancer model. Qβ-HPVag impeded tumor progression, increased infiltration of HPV-specific T cells, and significantly improved survival. The vaccine`s efficacy was associated with immune repolarization in the tumor microenvironment, characterized by expanded activated dendritic cell subsets (cDC1, cDC2, DC3). Notably, mice responding to treatment exhibited a higher percentage of migratory DC3 cells expressing CCR7. These findings suggest promising prospects for optimized VLP-based vaccines in treating HPV-associated head and neck cancer. © 2024 The Author(s).
- Mus musculus (House mouse),
- Cancer Research
IFNγ-dependent remodelling of the myeloid landscape underlies control of IFNγ-insensitive tumours
Preprint on BioRxiv : the Preprint Server for Biology on 28 March 2024 by Lau, V. W., Mead, G., et al.
PubMed
Loss of IFNγ-sensitivity by tumours is thought to be a mechanism enabling evasion, as some cancers lacking IFNγ-signalling demonstrate resistance to checkpoint immunotherapy. However, recent studies demonstrated that IFNγ-resistant tumours are well-controlled and sensitized for immunotherapy. The underlying mechanism leading to enhanced immune responses in those patients is unknown. Using IFNγ-insensitive melanoma tumours which were well-controlled by the endogenous anti-tumour response, we found that despite low basal MHC class I expression by tumours, CD8 + T cell infiltration was not hindered and, unexpectedly, their production of IFNγ was still important for tumour control. Mechanistically, IFNγ triggers pro-inflammatory remodelling of IFNγ-insensitive tumours, affecting the differentiation of myeloid cells. Predominantly, immunosuppressive macrophages are inhibited, while inflammatory phenotypes of monocytes and ‘mono-macs’ are preserved in IFNγ-insensitive tumours. This is supported by a co-dependency between CD8 + T cells and monocyte/macrophages, as depletion of one resulted in loss of the other. Our work demonstrates an important mechanistic understanding of how IFNγ resistance does not preclude failure of anti-tumour responses. Importantly, immune remodelling appears to be dominant in IFNγ-sensitive and IFNγ-insensitive mixed tumours, and is enriched in humans with tumours mutated in the IFNγ pathway, suggesting this may be leveraged for therapy in the future.
- Mus musculus (House mouse),
- Cancer Research
S100A8/A9 predicts response to PIM kinase and PD-1/PD-L1 inhibition in triple-negative breast cancer mouse models.
In Commun Med (Lond) on 20 February 2024 by Begg, L. R., Orriols, A., et al.
PubMed
Understanding why some triple-negative breast cancer (TNBC) patients respond poorly to existing therapies while others respond well remains a challenge. This study aims to understand the potential underlying mechanisms distinguishing early-stage TNBC tumors that respond to clinical intervention from non-responders, as well as to identify clinically viable therapeutic strategies, specifically for TNBC patients who may not benefit from existing therapies. We conducted retrospective bioinformatics analysis of historical gene expression datasets to identify a group of genes whose expression levels in early-stage tumors predict poor clinical outcomes in TNBC. In vitro small-molecule screening, genetic manipulation, and drug treatment in syngeneic mouse models of TNBC were utilized to investigate potential therapeutic strategies and elucidate mechanisms of drug action. Our bioinformatics analysis reveals a robust association between increased expression of immunosuppressive cytokine S100A8/A9 in early-stage tumors and subsequent disease progression in TNBC. A targeted small-molecule screen identifies PIM kinase inhibitors as capable of decreasing S100A8/A9 expression in multiple cell types, including TNBC and immunosuppressive myeloid cells. Combining PIM inhibition and immune checkpoint blockade induces significant antitumor responses, especially in otherwise resistant S100A8/A9-high PD-1/PD-L1-positive tumors. Notably, serum S100A8/A9 levels mirror those of tumor S100A8/A9 in a syngeneic mouse model of TNBC. Our data propose S100A8/A9 as a potential predictive and pharmacodynamic biomarker in clinical trials evaluating combination therapy targeting PIM and immune checkpoints in TNBC. This work encourages the development of S100A8/A9-based liquid biopsy tests for treatment guidance. © 2024. The Author(s).
- Cancer Research,
- Immunology and Microbiology
ID1 expressing macrophages support cancer cell stemness and limit CD8+ T cell infiltration in colorectal cancer.
In Nature Communications on 23 November 2023 by Shang, S., Yang, C., et al.
PubMed
Elimination of cancer stem cells (CSCs) and reinvigoration of antitumor immunity remain unmet challenges for cancer therapy. Tumor-associated macrophages (TAMs) constitute the prominant population of immune cells in tumor tissues, contributing to the formation of CSC niches and a suppressive immune microenvironment. Here, we report that high expression of inhibitor of differentiation 1 (ID1) in TAMs correlates with poor outcome in patients with colorectal cancer (CRC). ID1 expressing macrophages maintain cancer stemness and impede CD8+ T cell infiltration. Mechanistically, ID1 interacts with STAT1 to induce its cytoplasmic distribution and inhibits STAT1-mediated SerpinB2 and CCL4 transcription, two secretory factors responsible for cancer stemness inhibition and CD8+ T cell recruitment. Reducing ID1 expression ameliorates CRC progression and enhances tumor sensitivity to immunotherapy and chemotherapy. Collectively, our study highlights the pivotal role of ID1 in controlling the protumor phenotype of TAMs and paves the way for therapeutic targeting of ID1 in CRC. © 2023. The Author(s).
- Mus musculus (House mouse),
- Neuroscience,
- Cancer Research,
- Immunology and Microbiology
TIM-3 blockade in diffuse intrinsic pontine glioma models promotes tumor regression and antitumor immune memory.
In Cancer Cell on 13 November 2023 by Ausejo-Mauleon, I., Labiano, S., et al.
PubMed
Diffuse intrinsic pontine glioma (DIPG) is an aggressive brain stem tumor and the leading cause of pediatric cancer-related death. To date, these tumors remain incurable, underscoring the need for efficacious therapies. In this study, we demonstrate that the immune checkpoint TIM-3 (HAVCR2) is highly expressed in both tumor cells and microenvironmental cells, mainly microglia and macrophages, in DIPG. We show that inhibition of TIM-3 in syngeneic models of DIPG prolongs survival and produces long-term survivors free of disease that harbor immune memory. This antitumor effect is driven by the direct effect of TIM-3 inhibition in tumor cells, the coordinated action of several immune cell populations, and the secretion of chemokines/cytokines that create a proinflammatory tumor microenvironment favoring a potent antitumor immune response. This work uncovers TIM-3 as a bona fide target in DIPG and supports its clinical translation. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
Carcinogen exposure enhances cancer immunogenicity by blocking the development of an immunosuppressive tumor microenvironment.
In The Journal of Clinical Investigation on 16 October 2023 by Huang, M., Xia, Y., et al.
PubMed
Carcinogen exposure is strongly associated with enhanced cancer immunogenicity. Increased tumor mutational burden and resulting neoantigen generation have been proposed to link carcinogen exposure and cancer immunogenicity. However, the neoantigen-independent immunological impact of carcinogen exposure on cancer is unknown. Here, we demonstrate that chemical carcinogen-exposed cancer cells fail to establish an immunosuppressive tumor microenvironment (TME), resulting in their T cell-mediated rejection in vivo. A chemical carcinogen-treated breast cancer cell clone that lacked any additional coding region mutations (i.e., neoantigen) was rejected in mice in a T cell-dependent manner. Strikingly, the coinjection of carcinogen- and control-treated cancer cells prevented this rejection, suggesting that the loss of immunosuppressive TME was the dominant cause of rejection. Reduced M-CSF expression by carcinogen-treated cancer cells significantly suppressed tumor-associated macrophages (TAMs) and resulted in the loss of an immunosuppressive TME. Single-cell analysis of human lung cancers revealed a significant reduction in the immunosuppressive TAMs in former smokers compared with individuals who had never smoked. These findings demonstrate that carcinogen exposure impairs the development of an immunosuppressive TME and indicate a novel link between carcinogens and cancer immunogenicity.
- Mus musculus (House mouse),
- Genetics,
- Cancer Research
Adenosine A2A receptor is a tumor suppressor of NASH-associated hepatocellular carcinoma.
In Cell Reports Medicine on 19 September 2023 by Allard, B., Jacoberger-Foissac, C., et al.
PubMed
Inhibition of adenosine A2A receptor (A2AR) is a promising approach for cancer immunotherapy currently evaluated in several clinical trials. We here report that anti-obesogenic and anti-inflammatory functions of A2AR, however, significantly restrain hepatocellular carcinoma (HCC) development. Adora2a deletion in mice triggers obesity, non-alcoholic steatohepatitis (NASH), and systemic inflammation, leading to spontaneous HCC and promoting dimethylbenzyl-anthracene (DMBA)- or diethylnitrosamine (DEN)-induced HCC. Conditional Adora2a deletion reveals critical roles of myeloid and hepatocyte-derived A2AR signaling in restraining HCC by limiting hepatic inflammation and steatosis. Remarkably, the impact of A2AR pharmacological blockade on HCC development is dependent on pre-existing NASH. In support of our animal studies, low ADORA2A gene expression in human HCC is associated with cirrhosis, hepatic inflammation, and poor survival. Together, our study uncovers a previously unappreciated tumor-suppressive function for A2AR in the liver and suggests caution in the use of A2AR antagonists in patients with NASH and NASH-associated HCC. Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Neuroscience
Lymph node medulla regulates the spatiotemporal unfolding of resident dendritic cell networks.
In Immunity on 8 August 2023 by Ugur, M., Labios, R. J., et al.
PubMed
Unlike macrophage networks composed of long-lived tissue-resident cells within specific niches, conventional dendritic cells (cDCs) that generate a 3D network in lymph nodes (LNs) are short lived and continuously replaced by DC precursors (preDCs) from the bone marrow (BM). Here, we examined whether specific anatomical niches exist within which preDCs differentiate toward immature cDCs. In situ photoconversion and Prtn3-based fate-tracking revealed that the LN medullary cords are preferential entry sites for preDCs, serving as specific differentiation niches. Repopulation and fate-tracking approaches demonstrated that the cDC1 network unfolded from the medulla along the vascular tree toward the paracortex. During inflammation, collective maturation and migration of resident cDC1s to the paracortex created discontinuity in the medullary cDC1 network and temporarily impaired responsiveness. The decrease in local cDC1 density resulted in higher Flt3L availability in the medullary niche, which accelerated cDC1 development to restore the network. Thus, the spatiotemporal development of the cDC1 network is locally regulated in dedicated LN niches via sensing of cDC1 densities. Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology
Integrated Organ Immunity: Antigen-specific CD4-T cell-derived IFN-γ induced by BCG imprints prolonged lung innate resistance against respiratory viruses
Preprint on BioRxiv : the Preprint Server for Biology on 2 August 2023 by Lee, A., Floyd, K., et al.
PubMed
ABSTRACT Bacille Calmette-Guérin (BCG) vaccination can confer non-specific protection against heterologous pathogens. However, the underlying mechanisms remain mysterious. Here, we show that mice immunized intravenously with BCG exhibited reduced weight loss and/or improved viral clearance when challenged with SARS-CoV-2 and influenza. Protection was first evident between 14 - 21 days post vaccination, and lasted for at least 42 days. Remarkably, BCG induced a biphasic innate response in the lung, initially at day 1 and a subsequent prolonged phase starting at ∼15 days post vaccination, and robust antigen-specific Th1 responses. MyD88-dependent TLR signaling was essential for the induction of the innate and Th1 responses, and protection against SARS-CoV-2. Depletion of CD4 + T cells or IFN-γ activity prior to infection obliterated innate activation and protection. Single cell and spatial transcriptomics revealed CD4-dependent expression of interferon-stimulated genes (ISGs) in myeloid, type II alveolar and lung epithelial cells. Thus, BCG elicits “integrated organ immunity” where CD4+ T cells act on local myeloid and epithelial cells to imprint prolonged antiviral innate resistance.
- Immunology and Microbiology
Interventional hydrogel microsphere vaccine as an immune amplifier for activated antitumour immunity after ablation therapy.
In Nature Communications on 11 July 2023 by Liu, X., Zhuang, Y., et al.
PubMed
The response rate of pancreatic cancer to chemotherapy or immunotherapy pancreatic cancer is low. Although minimally invasive irreversible electroporation (IRE) ablation is a promising option for irresectable pancreatic cancers, the immunosuppressive tumour microenvironment that characterizes this tumour type enables tumour recurrence. Thus, strengthening endogenous adaptive antitumour immunity is critical for improving the outcome of ablation therapy and post-ablation immune therapy. Here we present a hydrogel microsphere vaccine that amplifies post-ablation anti-cancer immune response via releasing its cargo of FLT3L and CD40L at the relatively lower pH of the tumour bed. The vaccine facilitates migration of the tumour-resident type 1 conventional dendritic cells (cDC1) to the tumour-draining lymph nodes (TdLN), thus initiating the cDC1-mediated antigen cross-presentation cascade, resulting in enhanced endogenous CD8+ T cell response. We show in an orthotopic pancreatic cancer model in male mice that the hydrogel microsphere vaccine transforms the immunologically cold tumour microenvironment into hot in a safe and efficient manner, thus significantly increasing survival and inhibiting the growth of distant metastases. © 2023. The Author(s).
- Mus musculus (House mouse),
- Immunology and Microbiology
The African-centric P47S Variant of TP53 Confers Immune Dysregulation and Impaired Response to Immune Checkpoint Inhibition.
In Cancer Res Commun on 1 July 2023 by Stieg, D. C., Parris, J. L. D., et al.
PubMed
The tumor suppressor TP53 is the most frequently mutated gene in cancer and is mutationally inactivated in 50% of sporadic tumors. Inactivating mutations in TP53 also occur in Li Fraumeni syndrome (LFS). In addition to germline mutations in TP53 in LFS that completely inactivate this protein, there are many more germline mutant forms of TP53 in human populations that partially inactivate this protein: we call these partially inactivating mutations "hypomorphs." One of these hypomorphs is a SNP that exists in 6%-10% of Africans and 1%-2% of African Americans, which changes proline at amino acid 47 to serine (Pro47Ser; P47S). We previously showed that the P47S variant of p53 is intrinsically impaired for tumor suppressor function, and that this SNP is associated with increased cancer risk in mice and humans. Here we show that this SNP also influences the tumor microenvironment, and the immune microenvironment profile in P47S mice is more protumorigenic. At basal levels, P47S mice show impaired memory T-cell formation and function, along with increased anti-inflammatory (so-called "M2") macrophages. We show that in tumor-bearing P47S mice, there is an increase in immunosuppressive myeloid-derived suppressor cells and decreased numbers of activated dendritic cells, macrophages, and B cells, along with evidence for increased T-cell exhaustion in the tumor microenvironment. Finally, we show that P47S mice demonstrate an incomplete response to anti-PD-L1 therapy. Our combined data suggest that the African-centric P47S variant leads to both intrinsic and extrinsic defects in tumor suppression. Findings presented here show that the P47S variant of TP53 influences the immune microenvironment, and the immune response to cancer. This is the first time that a naturally occurring genetic variant of TP53 has been shown to negatively impact the immune microenvironment and the response to immunotherapy. © 2023 The Authors; Published by the American Association for Cancer Research.
- Immunology and Microbiology
CD8+ T Cells Trigger Auricular Dermatitis and Blepharitis in Mice after Zika Virus Infection in the Absence of CD4+ T Cells.
In The Journal of Investigative Dermatology on 1 June 2023 by Yi-Pin Lee, C., Carissimo, G., et al.
PubMed
Zika virus (ZIKV) became a public health concern when it re-emerged in 2015 owing to its ability to cause congenital deformities in the fetus and neurological complications in adults. Despite extensive data on protection, the interplay of protective and pathogenic adaptive immune responses toward ZIKV infection remains poorly understood. In this study, using a T-cell‒deficient mouse model that retains persistent ZIKV viral titers in the blood and organs, we show that the adoptive transfer of CD8+ T cells led to a significant reduction in viral load. This mouse model reveals that ZIKV can induce grossly visible auricular dermatitis and blepharitis, mediated by ZIKV-specific CD8+ T cells. Single-cell RNA sequencing of these causative CD8+ T cells from the ears shows an overactivated and elevated cytotoxic signature in mice with severe symptoms. Our results strongly suggest a role for CD8+ T-cell‒associated pathologies after ZIKV infection in CD4+ T-cell‒immunodeficient patients. Copyright © 2022 The Authors. Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology,
- Mus musculus (House mouse)
Robust IL-2-dependent antitumor immunotherapy requires targeting the high-affinity IL-2R on tumor-specific CD8+ T cells.
In Journal for Immunotherapy of Cancer on 1 June 2023 by LaPorte, K. M., Hernandez, R., et al.
PubMed
Development of interleukin (IL)-2-dependent antitumor responses focus on targeting the intermediate affinity IL-2R to stimulate memory-phenotypic CD8+ T and natural killer (NK) cells while minimizing regulatory T cell (Treg) expansion. However, this approach may not effectively engage tumor-specific T effector cells. Since tumor-antigen specific T cells upregulate the high-affinity IL-2R, we tested an IL-2 biologic, mouse IL-2/CD25, with selectivity toward the high-affinity IL-2R to support antitumor responses to tumors that vary in their immunogenicity. Mice were first implanted with either CT26, MC38, B16.F10, or 4T1 and after a tumor mass developed, they were treated with high-dose (HD) mouse (m)IL-2/CD25 alone or in combination with anti-programmed cell death protein-1 (PD-1) checkpoint blockade. Tumor growth was monitored and in parallel the immune signature in the tumor microenvironment (TME) was determined by a combination of multiparameter flow cytometry, functional assays, and enumeration of tumor-reactive T cells. We show that HD mIL-2/CD25, which preferentially stimulates the high-affinity IL-2R, but not IL-2/anti-IL-2 complexes with preferential activity toward the intermediate-affinity IL-2R, supports vigorous antitumor responses to immunogenic tumors as a monotherapy that were enhanced when combined with anti-PD-1. Treatment of CT26-bearing mice with HD mIL-2/CD25 led to a high CD8+:Treg ratio in the TME, increased frequency and function of tumor-specific CD8+ T effector cells with a less exhausted phenotype, and antitumor memory responses. Targeting the high-affinity IL-2R on tumor-specific T cells with HD mIL-2/CD25 alone or with PD-1 blockade supports antitumor responses, where the resulting memory response may afford long-term protection against tumor re-emergence. © Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- Cancer Research,
- Immunology and Microbiology,
- Mus musculus (House mouse)
In situ tumour arrays reveal early environmental control of cancer immunity.
In Nature on 1 June 2023 by Ortiz-Muñoz, G., Brown, M., et al.
PubMed
The immune phenotype of a tumour is a key predictor of its response to immunotherapy1-4. Patients who respond to checkpoint blockade generally present with immune-inflamed5-7 tumours that are highly infiltrated by T cells. However, not all inflamed tumours respond to therapy, and even lower response rates occur among tumours that lack T cells (immune desert) or that spatially exclude T cells to the periphery of the tumour lesion (immune excluded)8. Despite the importance of these tumour immune phenotypes in patients, little is known about their development, heterogeneity or dynamics owing to the technical difficulty of tracking these features in situ. Here we introduce skin tumour array by microporation (STAMP)-a preclinical approach that combines high-throughput time-lapse imaging with next-generation sequencing of tumour arrays. Using STAMP, we followed the development of thousands of arrayed tumours in vivo to show that tumour immune phenotypes and outcomes vary between adjacent tumours and are controlled by local factors within the tumour microenvironment. Particularly, the recruitment of T cells by fibroblasts and monocytes into the tumour core was supportive of T cell cytotoxic activity and tumour rejection. Tumour immune phenotypes were dynamic over time and an early conversion to an immune-inflamed phenotype was predictive of spontaneous or therapy-induced tumour rejection. Thus, STAMP captures the dynamic relationships of the spatial, cellular and molecular components of tumour rejection and has the potential to translate therapeutic concepts into successful clinical strategies. © 2023. The Author(s).
- Cancer Research,
- Immunology and Microbiology
PD-L1 methylation restricts PD-L1/PD-1 interactions to control cancer immune surveillance.
In Science Advances on 26 May 2023 by Changsheng, H., Ren, S., et al.
PubMed
Immune checkpoint inhibitors targeting programmed cell death protein 1 (PD-1) or programmed cell death 1 ligand 1 (PD-L1) have enabled some patients with cancer to experience durable, complete treatment responses; however, reliable anti-PD-(L)1 treatment response biomarkers are lacking. Our research found that PD-L1 K162 was methylated by SETD7 and demethylated by LSD2. Furthermore, PD-L1 K162 methylation controlled the PD-1/PD-L1 interaction and obviously enhanced the suppression of T cell activity controlling cancer immune surveillance. We demonstrated that PD-L1 hypermethylation was the key mechanism for anti-PD-L1 therapy resistance, investigated that PD-L1 K162 methylation was a negative predictive marker for anti-PD-1 treatment in patients with non-small cell lung cancer, and showed that the PD-L1 K162 methylation:PD-L1 ratio was a more accurate biomarker for predicting anti-PD-(L)1 therapy sensitivity. These findings provide insights into the regulation of the PD-1/PD-L1 pathway, identify a modification of this critical immune checkpoint, and highlight a predictive biomarker of the response to PD-1/PD-L1 blockade therapy.
- Cancer Research,
- Immunology and Microbiology
Addressing Tumor Heterogeneity by Sensitizing Resistant Cancer Cells to T cell-Secreted Cytokines.
In Cancer Discovery on 4 May 2023 by Ito, Y., Pan, D., et al.
PubMed
Tumor heterogeneity is a major barrier to cancer therapy, including immunotherapy. Activated T cells can efficiently kill tumor cells following recognition of MHC class I (MHC-I)-bound peptides, but this selection pressure favors outgrowth of MHC-I-deficient tumor cells. We performed a genome-scale screen to discover alternative pathways for T cell-mediated killing of MHC-I-deficient tumor cells. Autophagy and TNF signaling emerged as top pathways, and inactivation of Rnf31 (TNF signaling) and Atg5 (autophagy) sensitized MHC-I-deficient tumor cells to apoptosis by T cell-derived cytokines. Mechanistic studies demonstrated that inhibition of autophagy amplified proapoptotic effects of cytokines in tumor cells. Antigens from apoptotic MHC-I-deficient tumor cells were efficiently cross-presented by dendritic cells, resulting in heightened tumor infiltration by IFNγ-and TNFα-producing T cells. Tumors with a substantial population of MHC-I-deficient cancer cells could be controlled by T cells when both pathways were targeted using genetic or pharmacologic approaches. Tumor heterogeneity is a major barrier to immunotherapy. We show that MHC-I-deficient tumor cells are forced into apoptosis by T cell-derived cytokines when TNF signaling and autophagy pathways are targeted. This approach enables T cell-mediated elimination of tumors with a substantial population of resistant, MHC-I-deficient tumor cells. This article is highlighted in the In This Issue feature, p. 1027. ©2023 American Association for Cancer Research.
- Cancer Research,
- Immunology and Microbiology,
- In Vivo,
- Mus musculus (House mouse)
Intrinsic RIG-I restrains STAT5 activation to modulate antitumor activity of CD8+ T cells.
In The Journal of Clinical Investigation on 1 May 2023 by Jiang, X., Lin, J., et al.
PubMed
Antitumor activity of CD8+ T cells is potentially restrained by a variety of negative regulatory pathways that are triggered in the tumor microenvironment, yet, the exact mechanisms remain incompletely defined. Here, we report that intrinsic RIG-I in CD8+ T cells represents such a factor, as evidenced by observations that the tumor-restricting effect of endogenous or adoptively transferred CD8+ T cells was enhanced by intrinsic Rig-I deficiency or inhibition, with the increased accumulation, survival, and cytotoxicity of tumor-infiltrating CD8+ T cells. Mechanistically, T cell activation-induced RIG-I upregulation restrained STAT5 activation via competitive sequestering of HSP90. In accordance with this, the frequency of RIG-I+ tumor-infiltrating CD8+ T cells in human colon cancer positively correlated with attenuated survival and effector signatures of CD8+ T cells as well as poor prognosis. Collectively, these results implicate RIG-I as a potentially druggable factor for improving CD8+ T cell-based tumor immunotherapy.
- Cancer Research,
- Immunology and Microbiology
Oncogenic drivers dictate immune control of acute myeloid leukemia.
In Nature Communications on 14 April 2023 by Austin, R. J., Straube, J., et al.
PubMed
Acute myeloid leukemia (AML) is a genetically heterogeneous, aggressive hematological malignancy induced by distinct oncogenic driver mutations. The effect of specific AML oncogenes on immune activation or suppression is unclear. Here, we examine immune responses in genetically distinct models of AML and demonstrate that specific AML oncogenes dictate immunogenicity, the quality of immune response and immune escape through immunoediting. Specifically, expression of NrasG12D alone is sufficient to drive a potent anti-leukemia response through increased MHC Class II expression that can be overcome with increased expression of Myc. These data have important implications for the design and implementation of personalized immunotherapies for patients with AML. © 2023. The Author(s).
- Immunology and Microbiology
PHD2 Constrains Antitumor CD8+ T-cell Activity.
In Cancer Immunology Research on 1 March 2023 by Bisilliat Donnet, C., Acolty, V., et al.
PubMed
The prolyl hydroxylase domain/hypoxia-inducible factor (PHD/HIF) pathway has been implicated in a wide range of immune and inflammatory processes, including in the oxygen-deprived tumor microenvironment. To examine the effect of HIF stabilization in antitumor immunity, we deleted Phd2 selectively in T lymphocytes using the cre/lox system. We show that the deletion of PHD2 in lymphocytes resulted in enhanced regression of EG7-OVA tumors, in a HIF-1α-dependent manner. The enhanced control of neoplastic growth correlated with increased polyfunctionality of CD8+ tumor-infiltrating lymphocytes, as indicated by enhanced expression of IFNγ, TNFα, and granzyme B. Phenotypic and transcriptomic analyses pointed to a key role of glycolysis in sustaining CTL activity in the tumor bed and identified the PHD2/HIF-1 pathway as a potential target for cancer immunotherapy. ©2023 American Association for Cancer Research.
- Immunology and Microbiology
YAP-controlled MHC-I and CXCL10 expression potentiates antitumor immunity independently of IFNγ signaling
Preprint on BioRxiv : the Preprint Server for Biology on 25 February 2023 by Peng, L., Zhou, L., et al.
PubMed
Many efforts are underway to improve immune checkpoint blockade (ICB) therapy including potentiating MHC-I antigen processing and presentation. Accumulating evidence links the Hippo pathway to immunotherapy response, but the understanding of how the tumor-intrinsic Hippo signaling regulating antitumor immunity is limited. Here, we report that inhibition of the Hippo pathway coactivator YAP in tumor cells increases the expression of genes involving in MHC-I antigen processing and presenting machinery (APM) and CXCL10, promoting robust tumor-infiltrating of cytotoxic CD8 + T lymphocytes (CTLs) and overcoming tumor resistance to anti-PD1 ICB therapy. Mechanically, we find that YAP/TEAD complex directly binds and recruits NuRD complex to the NLRC5 promoter to repress NLRC5 transcription, thereby blunting MHC-I antigen presentation. Patient cohort analysis revealed that YAP expression negatively correlated with the expression of NLRC5 and MHC-I APM and intratumoral infiltration of CTLs. Collectively, our results suggest that a novel tumor- promoting function of YAP depends on NLRC5 to impair MHC-I antigen processing and presentation and provide a rationale for inhibiting YAP activity in ICB therapy for cancer.