InVivoMAb anti-mouse DR5 (CD262)
Product Details
The MD5-1 monoclonal antibody reacts with mouse death receptor 5 (DR5) also known as CD262 and TRAIL-R2. DR5 is a 55 kDa member of the TNF receptor superfamily and is expressed by most cell types. Upon binding to its ligand TRAIL, DR5 activates NF-κB and induces TRAIL-mediated apoptosis. The MD5-1 antibody has been shown to induce TRAIL-mediated apoptosis in vitro and in vivo.Specifications
| Isotype | Armenian Hamster IgG, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse DR5-Ig fusion protein |
| Reported Applications |
in vivo induction TRAIL-mediated apoptosis in vitro induction TRAIL-mediated apoptosis |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10950391 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
in vivo induction TRAIL-mediated apoptosis
Oliver, A. J., et al. (2020). "Primary and metastatic breast tumors cross-talk to influence immunotherapy responses" Oncoimmunology 9(1): 1802979. PubMed
The presence of a tumor can alter host immunity systematically. The immune-tumor interaction in one site may impact the local immune microenvironment in distal tissues through the circulation, and therefore influence the efficacy of immunotherapies to distant metastases. Improved understanding of the immune-tumor interactions during immunotherapy treatment in a metastatic setting may enhance the efficacy of current immunotherapies. Here we investigate the response to αPD-1/αCTLA4 and trimAb (αDR5, α4-1BB, αCD40) of 67NR murine breast tumors grown simultaneously in the mammary fat pad (MFP) and lung, a common site of breast cancer metastasis, and compared to tumors grown in isolation. Lung tumors present in isolation were resistant to both therapies. However, in MFP and lung tumor-bearing mice, the presence of a MFP tumor could increase lung tumor response to immunotherapy and decrease the number of lung metastases, leading to complete eradication of lung tumors in a proportion of mice. The MFP tumor influence on lung metastases was mediated by CD8(+) T cells, as CD8(+) T cell depletion abolished the difference in lung metastases. Furthermore, mice with concomitant MFP and lung tumors had increased tumor specific, effector CD8(+) T cells infiltration in the lungs. Thus, we propose a model where tumors in an immunogenic location can give rise to systemic anti-tumor CD8(+) T cell responses that could be utilized to target metastatic tumors. These results highlight the requirement for clinical consideration of cross-talk between primary and metastatic tumors for effective immunotherapy for cancers otherwise resistant to immunotherapy.
in vivo induction TRAIL-mediated apoptosis, in vitro induction TRAIL-mediated apoptosis
Condamine, T., et al. (2014). "ER stress regulates myeloid-derived suppressor cell fate through TRAIL-R-mediated apoptosis" J Clin Invest 124(6): 2626-2639. PubMed
Myeloid-derived suppressor cells (MDSCs) dampen the immune response thorough inhibition of T cell activation and proliferation and often are expanded in pathological conditions. Here, we studied the fate of MDSCs in cancer. Unexpectedly, MDSCs had lower viability and a shorter half-life in tumor-bearing mice compared with neutrophils and monocytes. The reduction of MDSC viability was due to increased apoptosis, which was mediated by increased expression of TNF-related apoptosis-induced ligand receptors (TRAIL-Rs) in these cells. Targeting TRAIL-Rs in naive mice did not affect myeloid cell populations, but it dramatically reduced the presence of MDSCs and improved immune responses in tumor-bearing mice. Treatment of myeloid cells with proinflammatory cytokines did not affect TRAIL-R expression; however, induction of ER stress in myeloid cells recapitulated changes in TRAIL-R expression observed in tumor-bearing hosts. The ER stress response was detected in MDSCs isolated from cancer patients and tumor-bearing mice, but not in control neutrophils or monocytes, and blockade of ER stress abrogated tumor-associated changes in TRAIL-Rs. Together, these data indicate that MDSC pathophysiology is linked to ER stress, which shortens the lifespan of these cells in the periphery and promotes expansion in BM. Furthermore, TRAIL-Rs can be considered as potential targets for selectively inhibiting MDSCs.
in vivo induction TRAIL-mediated apoptosis, in vitro induction TRAIL-mediated apoptosis
Martin, B. P., et al. (2011). "Antitumor activities and on-target toxicities mediated by a TRAIL receptor agonist following cotreatment with panobinostat" Int J Cancer 128(11): 2735-2747. PubMed
The recent development of novel targeted anticancer therapeutics such as histone deacetylase inhibitors (HDACi) and activators of the TRAIL pathway provide opportunities for the introduction of new treatment regimens in oncology. HDACi and recombinant TRAIL or agonistic anti-TRAIL receptor antibodies have been shown to induce synergistic tumor cell apoptosis and some therapeutic activity in vivo. Herein, we have used syngeneic preclinical models of human solid cancers to demonstrate that the HDACi panobinostat can sensitize tumor cells to apoptosis mediated by the anti-mouse TRAIL receptor antibody MD5-1. We demonstrate that the combination of panobinostat and MD5-1 can eradicate tumors grown subcutaneously and orthotopically in immunocompetent mice, while single agent treatment has minimal effect. However, escalation of the dose of panobinostat to enhance antitumor activity resulted in on-target MD5-1-mediated gastrointestinal toxicities that were fatal to the treated mice. Studies performed in mice with knockout of the TRAIL receptor showed that these mice could tolerate doses of the panobinostat/MD5-1 combination that were lethal in wild type mice resulting in superior tumor clearance. Given that clinical studies using HDACi and activators of the TRAIL pathway have been initiated, our preclinical data highlight the potential toxicities that could limit the use of such a treatment regimen. Our studies also demonstrate the power of using syngeneic in vivo tumor models as physiologically relevant preclinical systems to test the antitumor effects and identify potential side effects of novel anticancer regimens.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Inhibition of myeloid-derived suppressor cell arginase-1 production enhances T-cell-based immunotherapy against Cryptococcus neoformans infection.
In Nature Communications on 14 July 2022 by Li, Y. N., Wang, Z. W., et al.
PubMed
Cryptococcosis is a potentially lethal disease that is primarily caused by the fungus Cryptococcus neoformans, treatment options for cryptococcosis are limited. Here, we show glucuronoxylomannan, the major polysaccharide component of C. neoformans, induces the recruitment of neutrophilic myeloid-derived suppressor cells in mice and patients with cryptococcosis. Depletion of neutrophilic myeloid-derived suppressor cells enhances host defense against C. neoformans infection. We identify C-type lectin receptor-2d recognizes glucuronoxylomannan to potentiate the immunosuppressive activity of neutrophilic myeloid-derived suppressor cells by initiating p38-mediated production of the enzyme arginase-1, which inhibits T-cell mediated antifungal responses. Notably, pharmacological inhibition of arginase-1 expression by a specific inhibitor of p38, SB202190, or an orally available receptor tyrosine kinase inhibitor, vandetanib, significantly enhances T-cell mediated antifungal responses against cryptococcosis. These data reveal a crucial suppressive role of neutrophilic myeloid-derived suppressor cells during cryptococcosis and highlight a promising immunotherapeutic application by inhibiting arginase-1 production to combat infectious diseases. © 2022. The Author(s).
- Immu-depl,
- In Vivo,
- Mus musculus (House mouse)
Hepatic RACK1 deficiency protects against fulminant hepatitis through myeloid-derived suppressor cells.
In Theranostics on 11 March 2022 by Liu, G., Wang, Q., et al.
PubMed
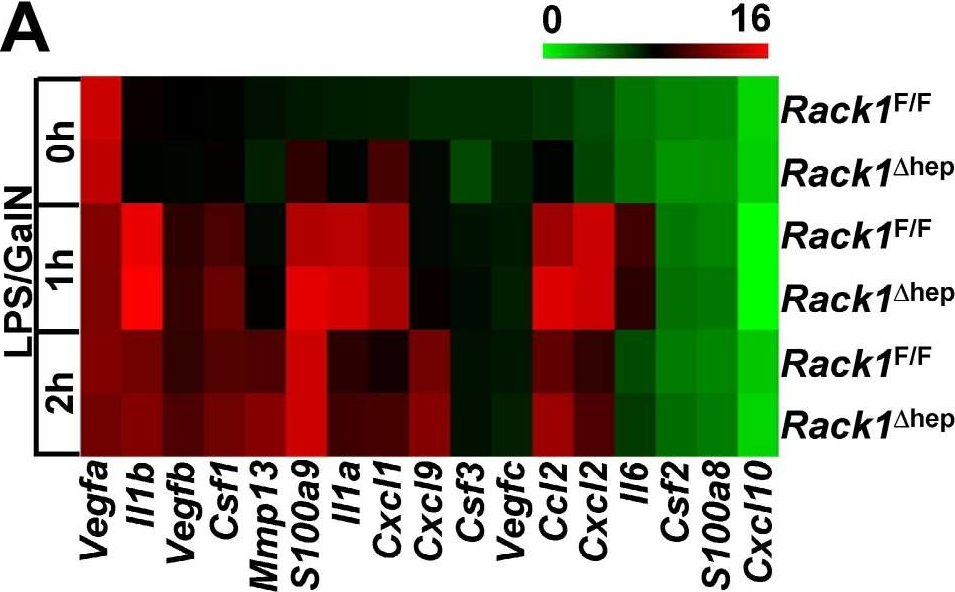
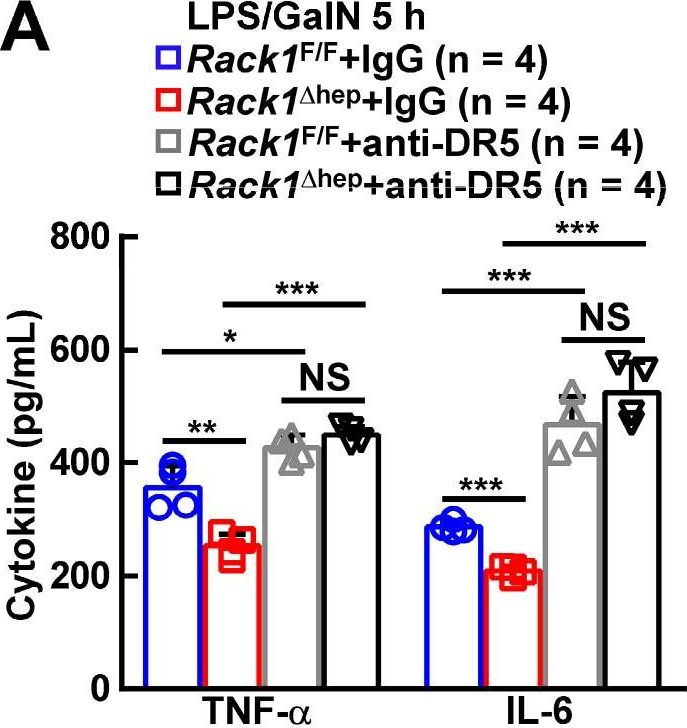
Fulminant hepatitis (FH) is a life-threatening disease with partially understood pathogenesis. It has been demonstrated that myeloid-derived suppressor cells (MDSCs) are recruited into the liver during this process, and their augmented accumulation by various strategies protects against liver injury. However, the underlying mechanism(s) remain elusive. Receptor for activated C kinase 1 (RACK1), a multi-functional scaffold protein, is highly expressed in normal liver and has been implicated in liver physiology and diseases, but the in vivo role of hepatic RACK1 in FH remains unknown. Methods: Survival curves and liver damage were monitored to investigate the in vivo role of hepatic RACK1 in FH. The liver microenvironment was explored by microarray-based transcriptome analysis, flow cytometry, immunoblotting, and immunohistochemistry. MDSCs were identified with phenotypic and functional characteristics. Functional antibodies were used to target MDSCs. Co-culture techniques were used to study the underlying mechanism(s) of protection. The interaction of RACK1 with histone deacetylase 1 (HDAC1) and the consequent effects on HDAC1 ubiquitination were analyzed. Ectopic expression of HDAC1 with recombinant adeno-associated virus serotype 8 was conducted to confirm the role of HDAC1 in the protective effects of hepatic RACK1 deficiency against FH. Post-translational modifications of RACK1 were also investigated during the induction of FH. Results: Liver-specific RACK1 deficiency rendered mice resistant to FH. RACK1-deficient livers exhibited high basal levels of chemokine (C-X-C motif) ligand 1 (CXCL1) and S100 calcium-binding protein A9 (S100A9), associated with MDSC accumulation under steady-state conditions. Targeting MDSCs with an antibody against either Gr1 or DR5 abrogated the protective effects of liver-specific RACK1 deficiency. Accumulated MDSCs inhibited inflammatory cytokine production from macrophages and enhanced IκB kinase (IKK)/NF-κB pathway activation in hepatocytes. Further investigation revealed that RACK1 maintained HDAC1 protein level in hepatocytes by direct binding, thereby controlling histone H3K9 and H3K27 acetylation at the Cxcl1 and S100a9 promoters. Ectopic expression of HDAC1 in livers with RACK1 deficiency partially reversed the augmented Cxcl1/S100a9 → MDSCs → IKK/NF-κB axis. During FH induction, RACK1 was phosphorylated at serine 110, enhancing its binding to ubiquitin-conjugating enzyme E2T and promoting its ubiquitination and degradation. Conclusion: Liver-specific RACK1 deficiency protects against FH through accelerated HDAC1 degradation and the consequent CXCL1/S100A9 upregulation and MDSC accumulation. © The author(s).
- Cancer Research
Targeting Depletion of Myeloid-Derived Suppressor Cells Enhances PD-L1 Blockade Efficacy in Gastric Cancer
Preprint on Research Square on 8 March 2022 by Tang, Y., Zhou, C., et al.
PubMed
h4>Background: /h4> Gastric cancer (GC) remains one of the most common malignancieswith poor prognosis worldwide. Immunotherapy based on PD-1/PD-L1 immune checkpoints has achieved robust and durable responses in various types of cancer, but only a subset of gastric cancer patients benefits from it.Myeloid-derived suppressor cells (MDSCs) have been demonstrated to suppress antitumor immunityand induceresistanceto PD-1/PD-L1 blockade immunotherapy. Death receptor5 (DR5), a receptor of TNF-related apoptosis-inducing ligand(TRAIL), is upregulated in MDSCs and is also commonly expressed on cancer cells, making it a desirable target for both MDSCs and DR5-positive GC. In this study, we evaluated the MDSCs depleting and immune modulating effect of the agonist DR5 antibody (MD5-1), and tested the therapeutic effectof targeting DR5 in combination with anti-PD-L1 as a new strategyfor the treatment of GC. Methods The MDSCs and their DR5 expression insyngeneic GC murine model were evaluated. TheMDSCs depleting effect by MD5-1 wereinvestigated. We compared the antitumor efficacy of MD5-1 in GC bearing T cell-deficient nude mice andsyngeneic 615 mice, and assessed its immune correlates. The antitumor effect of MD5-1 combininganti-PD-L1 in syngeneic GC murine model were tested, the tumor growth, mice survival and intratumoral T cell infiltration and activation were evaluated. Results The MDSCs accumulate in the gastric tumor-bearing 615 mice express high levels of DR5. Targeting DR5 using MD5-1specifically depleted MDSCs and enhancedT cell antitumor response, resulted in tumor growth inhibition.MD5-1 enhanced the antitumor effect of anti-PD-L1 antibody, led to complete regression in 40% ofestablished tumors and significantly extended the survival tumor-bearing mice. The enhanced antitumor effect by MD5-1 combining anti-PD-L1 was associatedwith increased CD8 + T cell infiltration and activation. Conclusions These results show that targeting DR5 enhances the antitumor effect of PD-L1 blockadetherapy in gastric cancer through eliminating MDSCs and improving CD8 + T cell antitumor response.Thus, targeting DR5 in combination with anti-PD-L1 may be a novel immunotherapy strategy forgastric cancer.
- In Vivo,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Primary and metastatic breast tumors cross-talk to influence immunotherapy responses.
In Oncoimmunology on 30 August 2020 by Oliver, A. J., Keam, S. P., et al.
PubMed
The presence of a tumor can alter host immunity systematically. The immune-tumor interaction in one site may impact the local immune microenvironment in distal tissues through the circulation, and therefore influence the efficacy of immunotherapies to distant metastases. Improved understanding of the immune-tumor interactions during immunotherapy treatment in a metastatic setting may enhance the efficacy of current immunotherapies. Here we investigate the response to αPD-1/αCTLA4 and trimAb (αDR5, α4-1BB, αCD40) of 67NR murine breast tumors grown simultaneously in the mammary fat pad (MFP) and lung, a common site of breast cancer metastasis, and compared to tumors grown in isolation. Lung tumors present in isolation were resistant to both therapies. However, in MFP and lung tumor-bearing mice, the presence of a MFP tumor could increase lung tumor response to immunotherapy and decrease the number of lung metastases, leading to complete eradication of lung tumors in a proportion of mice. The MFP tumor influence on lung metastases was mediated by CD8+ T cells, as CD8+ T cell depletion abolished the difference in lung metastases. Furthermore, mice with concomitant MFP and lung tumors had increased tumor specific, effector CD8+ T cells infiltration in the lungs. Thus, we propose a model where tumors in an immunogenic location can give rise to systemic anti-tumor CD8+ T cell responses that could be utilized to target metastatic tumors. These results highlight the requirement for clinical consideration of cross-talk between primary and metastatic tumors for effective immunotherapy for cancers otherwise resistant to immunotherapy. © 2020 The Author(s). Published with license by Taylor Francis Group, LLC.



