The TREM2 receptor may hold the keys to understanding how myeloid cells affect immune responses to neurological disorders and cancer.
Bio X Cell and The Scientist
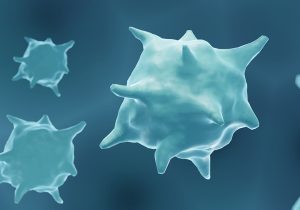
Macrophage-driven immune responses mediate pathogenesis and disease progression-and serve as potential therapeutic targets. ©ISTOCK.COM, Artur Plawgo
Myeloid cells such as monocytes, macrophages, and neutrophils are critical mediators and regulators of immune responses.1 Derived from hematopoietic stem cells found in the bone marrow, these cells are directed through a complex array of receptor-based signaling pathways. For example, pattern recognition receptors alert myeloid cells to potential tissue damage or pathogen presence, while cytokine and chemokine receptors regulate myeloid cell activation and deactivation.1,2 The combined actions of all of these receptor-mediated pathways give myeloid cells a great deal of flexibility and nuance, allowing them to adapt accordingly to specific conditions.1
Triggering receptors expressed on myeloid cells (TREMs) are a cell surface receptor family found on granulocytes, monocytes, macrophages, and dendritic cells-as well as other myeloid cells in general. TREMs define the threshold and duration of myeloid cell responses, both promoting and attenuating myeloid cell activation and differentiation.1 To that end, TREMs have been implicated in numerous diseases and conditions.
TREM2 Signaling in the Brain
TREM2 is expressed by tissue macrophages in various parts of the body, including the central nervous system (microglia), the bone (osteoclasts), liver, adipose tissue, skin, gut, and tumor microenvironment. TREM2 binds to lipids, including phospholipids and lipoproteins. This function allows it to detect apoptotic cells, which expose phospholipids during the programmed cell death process. It also binds proteins with a strong propensity for aggregation and accumulation, such as β-amyloid (Aβ). Indeed, TREM2 has been linked with neurological conditions such as Alzheimer's disease (AD). Researchers have shown that decreased TREM2 function facilitated AD progression, while TREM2 overexpression protected from Aβ plaque pathology.3
TREM2 as a Target for Cancer Therapeutics
Myeloid cells, and macrophages in particular, play key roles in controlling tumor formation, expansion, and metastasis. Unsurprisingly, the TREM2 receptor pathway has also been linked to microglial and macrophage activation during cancer. However, increased receptor activity, while beneficial for neurological disorders, appears to be detrimental in cancer. TREM2 knockout mice are more resistant to tumor growth and show enhanced responses to anti-PD-1 checkpoint inhibitor therapeutic approaches. Indeed, either deleting or blocking TREM2 receptors on macrophages appears to promote immunoactivation, as immunostimulatory myeloid subsets are expanded following treatment, leading to improved anti-tumor T cell responses.4 A recent study likewise indicated that the loss of microglial TREM2 function resulted in increased immunoactivation and tumoricidal capacity against glioblastoma.5 With TREM2 expression found in tumor macrophages in over 200 human cancer cases, the pathway may be a promising target for new therapeutic approaches.4
The Right Tools for Studying TREM2
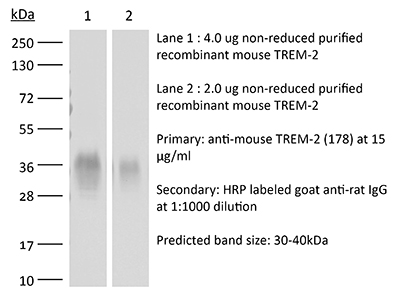
The InVivoMAb anti-mouse TREM2 monoclonal antibody can selectively detect TREM2 protein at low concentrations.
As TREM2-based therapeutic approaches for neurodegeneration and cancer advance in development, researchers must address any issues potentially caused by the differences between the murine and human versions of the receptor.1 Similarly, as TREM2 becomes a key therapeutic target, researchers will seek new ways to detect and alter the receptor pathway. Finally, the full range of potential ligands for TREM2-and their relative affinities-remains to be elucidated.
Distinguishing TREM2 from other TREM family members is crucial for understanding its specific functions and mechanisms. Bio X Cell offers a range of high-purity monoclonal antibodies designed for this purpose. The Bio X Cell InVivoMAb™ antibodies are functional antibodies specifically optimized for in vivo use. These antibodies feature ultra-low endotoxin levels and no preservatives, stabilizers, or carrier proteins to ensure consistent experimental results for pre-clinical studies. RecombiMAb anti-mouse TREM-2 antibody from Bio X Cell is particularly noteworthy for its specificity in Alzheimer's disease research, as it does not cross-react with TREM1 and can be used to effectively block TREM2 signaling in in vivo murine models. This antibody is valuable for investigating the function of the role of TREM2 in microglial function, amyloid plaque clearance, and neuroinflammation in Alzheimer's disease.
The study of TREM2 and other TREM receptors continues to present many unanswered questions, particularly regarding their impact on tau pathology and potential as therapeutic targets in neurodegenerative diseases. These questions can only be resolved if scientists have access to proper tools and reagents.
References
- Colonna, M. The biology of TREM receptors. Nat Rev Immunol. 2023;23,580-594.
- Greene JT, et al. Regulation of myeloid-cell activation. Curr Opin Immunol. 2021;73:34-42.
- Lee CYD, et al. Elevated TREM2 gene dosage reprograms microglia responsivity and ameliorates pathological phenotypes in Alzheimer's disease models. Neuron. 2018;97(5):1032-1048.e5.
- Molgora M, et al. TREM2 modulation remodels the tumor myeloid landscape enhancing anti-PD-1 immunotherapy. Cell. 2020;182(4):886-900.e17.
- Sun R, et al. TREM2 inhibition triggers antitumor cell activity of myeloid cells in glioblastoma. Sci Adv. 2023;9(19):eade3559.