InVivoSIM anti-human TNFα (Infliximab Biosimilar)
Product Description
Specifications
| Isotype | Human IgG1 |
|---|---|
| Recommended Isotype Control(s) | RecombiMAb human IgG1 isotype control, anti-hen egg lysozyme |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Human TNFα |
| Reported Applications |
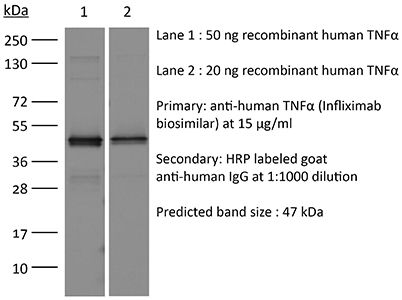
in vitro TNFα neutralization in vitro functional assay Flow Cytometry ELISA Western Blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤0.5EU/mg (≤0.0005EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein A |
| RRID | AB_2894727 |
| Molecular Weight | 150 kDa |
| Murine Pathogen Tests |
Ectromelia/Mousepox Virus: Negative Hantavirus: Negative K Virus: Negative Lactate Dehydrogenase-Elevating Virus: Negative Lymphocytic Choriomeningitis virus: Negative Mouse Adenovirus: Negative Mouse Cytomegalovirus: Negative Mouse Hepatitis Virus: Negative Mouse Minute Virus: Negative Mouse Norovirus: Negative Mouse Parvovirus: Negative Mouse Rotavirus: Negative Mycoplasma Pulmonis: Negative Pneumonia Virus of Mice: Negative Polyoma Virus: Negative Reovirus Screen: Negative Sendai Virus: Negative Theiler’s Murine Encephalomyelitis: Negative |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vitro TNFα neutralization
Wang X, Su S, Zhu Y, Cheng X, Cheng C, Chen L, Lei A, Zhang L, Xu Y, Ye D, Zhang Y, Li W, Zhang J (2023). "Metabolic Reprogramming via ACOD1 depletion enhances function of human induced pluripotent stem cell-derived CAR-macrophages in solid tumors" N
PubMed
The pro-inflammatory state of macrophages, underpinned by their metabolic condition, is essentially affecting their capacity of combating tumor cells. Here we find, via a pooled metabolic gene knockout CRISPR screen that KEAP1 and ACOD1 are strong regulators of the pro-inflammatory state in macrophages. We show that ACOD1 knockout macrophages, generated in our induced pluripotent stem cell-derived CAR-macrophage (CAR-iMAC) platform, are strongly and persistently polarized toward the pro-inflammatory state, which manifests in increased reactive oxygen species (ROS) production, more potent phagocytosis and enhanced cytotoxic functions against cancer cells in vitro. In ovarian or pancreatic cancer mouse models, ACOD1-depleted CAR-iMACs exhibit enhanced capacity in repressing tumors, leading to increased survival. In addition, combining ACOD1-depleted CAR-iMACs with immune checkpoint inhibitors (ICI), such as anti-CD47 or anti-PD1 antibodies, result in even stronger tumor suppressing effect. Mechanistically, the depletion of ACOD1 reduces levels of the immuno-metabolite itaconate, allowing KEAP1 to prevent NRF2 from entering the nucleus to activate an anti-inflammatory program. This study thus lays down the proof of principle for targeting ACOD1 in myeloid cells for cancer immunotherapy and introduces metabolically engineered human iPSC-derived CAR-iMACs cells with enhanced polarization and anti-tumor functions in adoptive cell transfer therapies.
in vitro functional assay
Di Ianni A, Fraone T, Balestra P, Cowan K, Riccardi Sirtori F, Barbero L (2023). "Assessing MAPPs assay as a tool to predict the immunogenicity potential of protein therapeutics" Life Sci Alliance 7(1):e202302095.
PubMed
MHC-II-associated peptide proteomics (MAPPs) is a mass spectrometry-based (MS) method to identify naturally presented MHC-II-associated peptides that could elicit CD4+T cell activation. MAPPs assay is considered one of the assays that better characterize the safety of biotherapeutics by driving the selection of the best candidates concerning their immunogenicity risk. However, there is little knowledge about the impact of bead material on the recovery of MHC-II MS-eluted ligands in MAPPs assays. Here, we firstly describe a robust MAPPs protocol by implementing streptavidin magnetic beads for the isolation of these peptides instead of commonly used NHS-activated beads. Moreover, we assessed the impact of the cell medium used for cell cultures on the morphology and recovery of the in vitro-generated APCs, and its potential implications in the amount of MHC-II isolated peptides. We also described an example of a MAPPs assay application to investigate drug-induced immunogenicity of two bispecific antibodies and compared them with monospecific trastuzumab IgG1 control. This work highlighted the importance of MAPPs in the preclinical in vitro strategy to mitigate the immunogenicity risk of biotherapeutics.
in vitro TNFα neutralization
Zheng N, Fang J, Xue G, Wang Z, Li X, Zhou M, Jin G, Rahman MM, McFadden G, Lu Y (2022). "Induction of tumor cell autosis by myxoma virus-infected CAR-T and TCR-T cells to overcome primary and acquired resistance" Cancer Cell 40(9):973-985.e7.
PubMed
Cytotoxicity of tumor-specific T cells requires tumor cell-to-T cell contact-dependent induction of classic tumor cell apoptosis and pyroptosis. However, this may not trigger sufficient primary responses of solid tumors to adoptive cell therapy or prevent tumor antigen escape-mediated acquired resistance. Here we test myxoma virus (MYXV)-infected tumor-specific T (TMYXV) cells expressing chimeric antigen receptor (CAR) or T cell receptor (TCR), which systemically deliver MYXV into solid tumors to overcome primary resistance. In addition to T cell-induced apoptosis and pyroptosis, tumor eradication by CAR/TCR-TMYXV cells is also attributed to tumor cell autosis induction, a special type of cell death. Mechanistically, T cell-derived interferon γ (IFNγ)-protein kinase B (AKT) signaling synergizes with MYXV-induced M-T5-SKP-1-VPS34 signaling to trigger robust tumor cell autosis. CAR/TCR-TMYXV-elicited autosis functions as a type of potent bystander killing to restrain antigen escape. We uncover an unexpected synergy between T cells and MYXV to bolster solid tumor cell autosis that reinforces tumor clearance.
Product Citations
-
Validation of the i-Tracker Drug and Total Anti-Drug Antibody CLIA Assays on IDS-iSYS for Therapeutic Drug Monitoring in Adalimumab- and Infliximab-Treated Patients.
In Diagnostics (Basel) on 25 September 2025 by Dossou, A. S., Kang, S., et al.
PubMed
Background/Objectives: Adalimumab and Infliximab are biologics used to treat autoimmune diseases. Monitoring drug and anti-drug antibody (ADA) levels in patients helps optimize treatment. However, current quantitation methodologies for drug and total (free and drug-bound) ADAs often involve multi-step workflows. Automated systems can streamline the process. The i-Tracker chemiluminescent immunoassays (CLIA) are cartridge-based kits for quantifying serum levels of drugs such as Adalimumab, Infliximab, and associated ADAs. Herein, we aimed to establish performance characteristics of the i-Tracker Adalimumab, Infliximab, and total ADAs in serum on the random-access analyzer IDS-iSYS and to compare patient results with an electrochemiluminescent immunoassay (ECLIA)-based reference method. Methods: Remnant serum specimens, calibration material, or spiked serum were used to evaluate assay linearity, precision, functional sensitivity, and accuracy on the IDS-iSYS analyzer and to perform the method comparison. Results: The assays displayed linearity, accuracy, and up to 8% imprecision across clinically relevant analyte ranges. Compared to the reference method, the drug assays exhibited a strong linear fit (correlation coefficient > 0.95) with <±1.0 µg/mL mean bias. The total anti-Adalimumab assay demonstrated over 85% qualitative agreement. The total anti-Infliximab assay, however, showed higher detection rate of ADAs in Infliximab-treated patient specimens, yielding < 60% negative agreement with the reference method. Although i-Tracker total ADA assays exhibited drug sensitivity, they still detected ADAs in supratherapeutic drug concentrations. Conclusions: The i-Tracker assays demonstrated robust analytical performance, suggesting potential for clinical application. The method comparison underscored functional differences with the reference method, an important consideration when transitioning assay formats for monitoring Adalimumab- and Infliximab-treated patients.
-
-
Homo sapiens (Human)
-
Immunology and Microbiology
Assessing MAPPs assay as a tool to predict the immunogenicity potential of protein therapeutics.
In Life Sci Alliance on 1 January 2024 by Di Ianni, A., Fraone, T., et al.
PubMed
MHC-II-associated peptide proteomics (MAPPs) is a mass spectrometry-based (MS) method to identify naturally presented MHC-II-associated peptides that could elicit CD4+T cell activation. MAPPs assay is considered one of the assays that better characterize the safety of biotherapeutics by driving the selection of the best candidates concerning their immunogenicity risk. However, there is little knowledge about the impact of bead material on the recovery of MHC-II MS-eluted ligands in MAPPs assays. Here, we firstly describe a robust MAPPs protocol by implementing streptavidin magnetic beads for the isolation of these peptides instead of commonly used NHS-activated beads. Moreover, we assessed the impact of the cell medium used for cell cultures on the morphology and recovery of the in vitro-generated APCs, and its potential implications in the amount of MHC-II isolated peptides. We also described an example of a MAPPs assay application to investigate drug-induced immunogenicity of two bispecific antibodies and compared them with monospecific trastuzumab IgG1 control. This work highlighted the importance of MAPPs in the preclinical in vitro strategy to mitigate the immunogenicity risk of biotherapeutics.
-
-
-
Biochemistry and Molecular biology
-
Cancer Research
-
Cell Biology
-
Stem Cells and Developmental Biology
Metabolic Reprogramming via ACOD1 depletion enhances function of human induced pluripotent stem cell-derived CAR-macrophages in solid tumors.
In Nat Commun on 18 September 2023 by Wang, X., Su, S., et al.
PubMed
The pro-inflammatory state of macrophages, underpinned by their metabolic condition, is essentially affecting their capacity of combating tumor cells. Here we find, via a pooled metabolic gene knockout CRISPR screen that KEAP1 and ACOD1 are strong regulators of the pro-inflammatory state in macrophages. We show that ACOD1 knockout macrophages, generated in our induced pluripotent stem cell-derived CAR-macrophage (CAR-iMAC) platform, are strongly and persistently polarized toward the pro-inflammatory state, which manifests in increased reactive oxygen species (ROS) production, more potent phagocytosis and enhanced cytotoxic functions against cancer cells in vitro. In ovarian or pancreatic cancer mouse models, ACOD1-depleted CAR-iMACs exhibit enhanced capacity in repressing tumors, leading to increased survival. In addition, combining ACOD1-depleted CAR-iMACs with immune checkpoint inhibitors (ICI), such as anti-CD47 or anti-PD1 antibodies, result in even stronger tumor suppressing effect. Mechanistically, the depletion of ACOD1 reduces levels of the immuno-metabolite itaconate, allowing KEAP1 to prevent NRF2 from entering the nucleus to activate an anti-inflammatory program. This study thus lays down the proof of principle for targeting ACOD1 in myeloid cells for cancer immunotherapy and introduces metabolically engineered human iPSC-derived CAR-iMACs cells with enhanced polarization and anti-tumor functions in adoptive cell transfer therapies.
-
-
-
Cancer Research
-
Immunology and Microbiology
Induction of tumor cell autosis by myxoma virus-infected CAR-T and TCR-T cells to overcome primary and acquired resistance.
In Cancer Cell on 12 September 2022 by Zheng, N., Fang, J., et al.
PubMed
Cytotoxicity of tumor-specific T cells requires tumor cell-to-T cell contact-dependent induction of classic tumor cell apoptosis and pyroptosis. However, this may not trigger sufficient primary responses of solid tumors to adoptive cell therapy or prevent tumor antigen escape-mediated acquired resistance. Here we test myxoma virus (MYXV)-infected tumor-specific T (TMYXV) cells expressing chimeric antigen receptor (CAR) or T cell receptor (TCR), which systemically deliver MYXV into solid tumors to overcome primary resistance. In addition to T cell-induced apoptosis and pyroptosis, tumor eradication by CAR/TCR-TMYXV cells is also attributed to tumor cell autosis induction, a special type of cell death. Mechanistically, T cell-derived interferon γ (IFNγ)-protein kinase B (AKT) signaling synergizes with MYXV-induced M-T5-SKP-1-VPS34 signaling to trigger robust tumor cell autosis. CAR/TCR-TMYXV-elicited autosis functions as a type of potent bystander killing to restrain antigen escape. We uncover an unexpected synergy between T cells and MYXV to bolster solid tumor cell autosis that reinforces tumor clearance.
-
-
-
Immunology and Microbiology
Assessing Major Histocompatibility Complex-Associated Peptide Proteomics assay as a tool to predict immunogenicity potential of protein therapeutics and antigens
In Research Square on 19 August 2022 by Barbero, L., Ianni, A. D., et al.
-