InVivoMAb anti-mouse OX40 (CD134)
Product Description
Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse OX40-CD4 chimeric protein |
| Reported Applications |
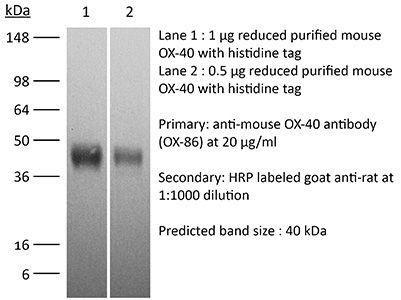
in vivo OX40 activation in vitro OX40 activation Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107592 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo OX40 activation
Bartkowiak, T., et al (2015). "Unique potential of 4-1BB agonist antibody to promote durable regression of HPV+ tumors when combined with an E6/E7 peptide vaccine" Proc Natl Acad Sci U S A 112(38): E5290-5299.
PubMed
Antibody modulation of T-cell coinhibitory (e.g., CTLA-4) or costimulatory (e.g., 4-1BB) receptors promotes clinical responses to a variety of cancers. Therapeutic cancer vaccination, in contrast, has produced limited clinical benefit and no curative therapies. The E6 and E7 oncoproteins of human papilloma virus (HPV) drive the majority of genital cancers, and many oropharyngeal tumors. We discovered 15-19 amino acid peptides from HPV-16 E6/E7 for which induction of T-cell immunity correlates with disease-free survival in patients treated for high-grade cervical neoplasia. We report here that intranasal vaccination with these peptides and the adjuvant alpha-galactosylceramide elicits systemic and mucosal T-cell responses leading to reduced HPV(+) TC-1 tumor growth and prolonged survival in mice. We hypothesized that the inability of these T cells to fully reject established tumors resulted from suppression in the tumor microenvironment which could be ameliorated through checkpoint modulation. Combining this E6/E7 peptide vaccine with checkpoint blockade produced only modest benefit; however, coadministration with a 4-1BB agonist antibody promoted durable regression of established genital TC-1 tumors. Relative to other therapies tested, this combination of vaccine and alpha4-1BB promoted the highest CD8(+) versus regulatory FoxP3(+) T-cell ratios, elicited 2- to 5-fold higher infiltration by E7-specific CTL, and evoked higher densities of highly cytotoxic TcEO (T cytotoxic Eomesodermin) CD8 (>70-fold) and ThEO (T helper Eomesodermin) CD4 (>17-fold) T cells. These findings have immediate clinical relevance both in terms of the direct clinical utility of the vaccine studied and in illustrating the potential of 4-1BB antibody to convert therapeutic E6/E7 vaccines already in clinical trials into curative therapies.
in vivo OX40 activation
Makkouk, A., et al (2015). "Three steps to breaking immune tolerance to lymphoma: a microparticle approach" Cancer Immunol Res 3(4): 389-398.
PubMed
In situ immunization aims at generating antitumor immune responses through manipulating the tumor microenvironment. On the basis of recent advances in the understanding of antitumor immunity, we designed a three-step approach to in situ immunization to lymphoma: (i) inducing immunogenic tumor cell death with the chemotherapeutic drug doxorubicin. Doxorubicin enhances the expression of “eat-me” signals by dying tumor cells, facilitating their phagocytosis by dendritic cells (DC). Because of the vesicant activity of doxorubicin, microparticles made of biodegradable polymer poly(lactide-co-glycolide) or PLGA can safely deliver doxorubicin intratumorally and are effective vaccine adjuvants, (ii) enhancing T-cell activation using anti-OX40 and (iii) sustaining T-cell responses by checkpoint blockade using anti-CTLA-4. In vitro, doxorubicin microparticles were less cytotoxic to DCs than to B lymphoma cells, did not require internalization by tumor cells, and significantly enhanced phagocytosis of tumor cells by DCs as compared with soluble doxorubicin. In mice, this three-step therapy induced CD4- and CD8-dependent systemic immune responses that enhanced T-cell infiltration into distant tumors, leading to their eradication and significantly improving survival. Our findings demonstrate that systemic antitumor immune responses can be generated locally by three-step therapy and merit further investigation as an immunotherapy for patients with lymphoma.
in vivo OX40 activation
Zander, R. A., et al (2015). "PD-1 Co-inhibitory and OX40 Co-stimulatory Crosstalk Regulates Helper T Cell Differentiation and Anti-Plasmodium Humoral Immunity" Cell Host Microbe 17(5): 628-641.
PubMed
The differentiation and protective capacity of Plasmodium-specific T cells are regulated by both positive and negative signals during malaria, but the molecular and cellular details remain poorly defined. Here we show that malaria patients and Plasmodium-infected rodents exhibit atypical expression of the co-stimulatory receptor OX40 on CD4 T cells and that therapeutic enhancement of OX40 signaling enhances helper CD4 T cell activity, humoral immunity, and parasite clearance in rodents. However, these beneficial effects of OX40 signaling are abrogated following coordinate blockade of PD-1 co-inhibitory pathways, which are also upregulated during malaria and associated with elevated parasitemia. Co-administration of biologics blocking PD-1 and promoting OX40 signaling induces excessive interferon-gamma that directly limits helper T cell-mediated support of humoral immunity and decreases parasite control. Our results show that targeting OX40 can enhance Plasmodium control and that crosstalk between co-inhibitory and co-stimulatory pathways in pathogen-specific CD4 T cells can impact pathogen clearance.
in vivo OX40 activation
Guo, Z., et al (2014). "PD-1 blockade and OX40 triggering synergistically protects against tumor growth in a murine model of ovarian cancer" PLoS One 9(2): e89350.
PubMed
The co-inhibitory receptor Programmed Death-1 (PD-1) curtails immune responses and prevent autoimmunity, however, tumors exploit this pathway to escape from immune destruction. The co-stimulatory receptor OX40 is upregulated on T cells following activation and increases their clonal expansion, survival and cytokine production when engaged. Although antagonistic anti-PD-1 or agonistic anti-OX40 antibodies can promote the rejection of several murine tumors, some poorly immunogenic tumors were refractory to this treatment. In the present study, we evaluated the antitumor effects and mechanisms of combinatorial PD-1 blockade and OX40 triggering in a murine ID8 ovarian cancer model. Although individual anti-PD-1 or OX40 mAb treatment was ineffective in tumor protection against 10-day established ID8 tumor, combined anti-PD-1/OX40 mAb treatment markedly inhibited tumor outgrowth with 60% of mice tumor free 90 days after tumor inoculation. Tumor protection was associated with a systemic immune response with memory and antigen specificity and required CD4(+) cells and CD8(+) T cells. The anti-PD-1/OX40 mAb treatment increased CD4(+) and CD8(+) cells and decreased immunosuppressive CD4(+)FoxP3(+) regulatory T (Treg) cells and CD11b(+)Gr-1(+) myeloid suppressor cells (MDSC), giving rise to significantly higher ratios of both effector CD4(+) and CD8(+) cells to Treg and MDSC in peritoneal cavity; Quantitative RT-PCR data further demonstrated the induction of a local immunostimulatory milieu by anti-PD-1/OX40 mAb treatment. The splenic CD8(+) T cells from combined mAb treated mice produced high levels of IFN-gamma upon tumor antigen stimulation and exhibited antigen-specific cytolytic activity. To our knowledge, this is the first study testing the antitumor effects of combined anti-PD-1/OX40 mAb in a murine ovarian cancer model, and our results provide a rationale for clinical trials evaluating ovarian cancer immunotherapy using this combination of mAb.
in vivo OX40 activation
Krupnick, A. S., et al (2014). "Central memory CD8+ T lymphocytes mediate lung allograft acceptance" J Clin Invest 124(3): 1130-1143.
PubMed
Memory T lymphocytes are commonly viewed as a major barrier for long-term survival of organ allografts and are thought to accelerate rejection responses due to their rapid infiltration into allografts, low threshold for activation, and ability to produce inflammatory mediators. Because memory T cells are usually associated with rejection, preclinical protocols have been developed to target this population in transplant recipients. Here, using a murine model, we found that costimulatory blockade-mediated lung allograft acceptance depended on the rapid infiltration of the graft by central memory CD8+ T cells (CD44(hi)CD62L(hi)CCR7+). Chemokine receptor signaling and alloantigen recognition were required for trafficking of these memory T cells to lung allografts. Intravital 2-photon imaging revealed that CCR7 expression on CD8+ T cells was critical for formation of stable synapses with antigen-presenting cells, resulting in IFN-gamma production, which induced NO and downregulated alloimmune responses. Thus, we describe a critical role for CD8+ central memory T cells in lung allograft acceptance and highlight the need for tailored approaches for tolerance induction in the lung.
in vivo OX40 activation
Redmond, W. L., et al (2014). "Combined targeting of costimulatory (OX40) and coinhibitory (CTLA-4) pathways elicits potent effector T cells capable of driving robust antitumor immunity" Cancer Immunol Res 2(2): 142-153.
PubMed
Ligation of the TNF receptor family costimulatory molecule OX40 (CD134) with an agonist anti-OX40 monoclonal antibody (mAb) enhances antitumor immunity by augmenting T-cell differentiation as well as turning off the suppressive activity of the FoxP3(+)CD4(+) regulatory T cells (Treg). In addition, antibody-mediated blockade of the checkpoint inhibitor CTLA-4 releases the “brakes” on T cells to augment tumor immunotherapy. However, monotherapy with these agents has limited therapeutic benefit particularly against poorly immunogenic murine tumors. Therefore, we examined whether the administration of agonist anti-OX40 therapy in the presence of CTLA-4 blockade would enhance tumor immunotherapy. Combined anti-OX40/anti-CTLA-4 immunotherapy significantly enhanced tumor regression and the survival of tumor-bearing hosts in a CD4 and CD8 T cell-dependent manner. Mechanistic studies revealed that the combination immunotherapy directed the expansion of effector T-bet(high)/Eomes(high) granzyme B(+) CD8 T cells. Dual immunotherapy also induced distinct populations of Th1 [interleukin (IL)-2, IFN-gamma], and, surprisingly, Th2 (IL-4, IL-5, and IL-13) CD4 T cells exhibiting increased T-bet and Gata-3 expression. Furthermore, IL-4 blockade inhibited the Th2 response, while maintaining the Th1 CD4 and effector CD8 T cells that enhanced tumor-free survival. These data demonstrate that refining the global T-cell response during combination immunotherapy can further enhance the therapeutic efficacy of these agents.
in vitro OX40 activation
Hu, Z., et al (2013). "Regulatory CD8+ T cells associated with erosion of immune surveillance in persistent virus infection suppress in vitro and have a reversible proliferative defect" J Immunol 191(1): 312-322.
PubMed
CD4(+) T cell help is critical for CD8(+) T cell memory and immune surveillance against persistent virus infections. Our recent data have showed the lack of CD4(+) T cells leads to the generation of an IL-10-producing CD8(+) T cell population during persistent murine gamma-herpesvirus-68 (MHV-68) infection. IL-10 from these cells is partly responsible for erosion in immune surveillance, leading to spontaneous virus reactivation in lungs. In this study, we further characterized the generation, phenotype, and function of these IL-10-producing CD8(+) T cells by comparing with a newly identified IL-10-producing CD8(+) T cell population present during the acute stage of the infection. The IL-10-producing CD8(+) populations in acute and chronic stages differed in their requirement for CD4(+) T cell help, the dependence on IL-2/CD25 and CD40-CD40L pathways, and the ability to proliferate in vitro in response to anti-CD3 stimulation. IL-10-producing CD8(+) T cells in the chronic stage showed a distinct immunophenotypic profile, sharing partial overlap with the markers of previously reported regulatory CD8(+) T cells, and suppressed the proliferation of naive CD8(+) T cells. Notably, they retained the ability to produce effector cytokines and cytotoxic activity. In addition, the proliferative defect of the cells could be restored by addition of exogenous IL-2 or blockade of IL-10. These data suggest that the IL-10-producing CD8(+) T cells arising in chronic MHV-68 infection in the absence of CD4(+) T cell help belong to a subset of CD8(+) regulatory T cells.
in vivo OX40 activation
Kurche, J. S., et al (2012). "Type I IFN-dependent T cell activation is mediated by IFN-dependent dendritic cell OX40 ligand expression and is independent of T cell IFNR expression" J Immunol 188(2): 585-593.
PubMed
Type I IFNs are important for direct control of viral infection and generation of adaptive immune responses. Recently, direct stimulation of CD4(+) T cells via type I IFNR has been shown to be necessary for the formation of functional CD4(+) T cell responses. In contrast, we find that CD4(+) T cells do not require intrinsic type I IFN signals in response to combined TLR/anti-CD40 vaccination. Rather, the CD4 response is dependent on the expression of type I IFNR (IFNalphaR) on innate cells. Further, we find that dendritic cell (DC) expression of the TNF superfamily member OX40 ligand was dependent on type I IFN signaling in the DC, resulting in a reduced CD4(+) T cell response that could be substantially rescued by an agonistic Ab to the receptor OX40. Taken together, we show that the IFNalphaR dependence of the CD4(+) T cell response is accounted for exclusively by defects in DC activation.
in vivo OX40 activation
Xiao, X., et al (2012). "New insights on OX40 in the control of T cell immunity and immune tolerance in vivo" J Immunol 188(2): 892-901.
PubMed
OX40 is a T cell costimulatory molecule that belongs to the TNFR superfamily. In the absence of immune activation, OX40 is selectively expressed by Foxp3(+) regulatory T cells (Tregs), but not by resting conventional T cells. The exact role of OX40 in Treg homeostasis and function remains incompletely defined. In this study, we demonstrate that OX40 engagement in vivo in naive mice induces initial expansion of Foxp3(+) Tregs, but the expanded Tregs have poor suppressive function and exhibit features of exhaustion. We also show that OX40 enables the activation of the Akt and Stat5 pathways in Tregs, resulting in transient proliferation of Tregs and reduced levels of Foxp3 expression. This creates a state of relative IL-2 deficiency in naive mice that further impacts Tregs. This exhausted Treg phenotype can be prevented by exogenous IL-2, as both OX40 and IL-2 agonists drive further expansion of Tregs in vivo. Importantly, Tregs expanded by both OX40 and IL-2 agonists are potent suppressor cells, and in a heart transplant model, they promote long-term allograft survival. Our data reveal a novel role for OX40 in promoting immune tolerance and may have important clinical implications.
in vivo OX40 activation
Murray, S. E., et al (2011). "NF-kappaB-inducing kinase plays an essential T cell-intrinsic role in graft-versus-host disease and lethal autoimmunity in mice" J Clin Invest 121(12): 4775-4786.
PubMed
NF-kappaB-inducing kinase (NIK) is an essential upstream kinase in noncanonical NF-kappaB signaling. NIK-dependent NF-kappaB activation downstream of several TNF receptor family members mediates lymphoid organ development and B cell homeostasis. Peripheral T cell populations are normal in the absence of NIK, but the role of NIK during in vivo T cell responses to antigen has been obscured by other developmental defects in NIK-deficient mice. Here, we have identified a T cell-intrinsic requirement for NIK in graft-versus-host disease (GVHD), wherein NIK-deficient mouse T cells transferred into MHC class II mismatched recipients failed to cause GVHD. Although NIK was not necessary for antigen receptor signaling, it was absolutely required for costimulation through the TNF receptor family member OX40 (also known as CD134). When we conditionally overexpressed NIK in T cells, mice suffered rapid and fatal autoimmunity characterized by hyperactive effector T cells and poorly suppressive Foxp3(+) Tregs. Together, these data illuminate a critical T cell-intrinsic role for NIK during immune responses and suggest that its tight regulation is critical for avoiding autoimmunity.
Product Citations
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Genetics
-
Immunology and Microbiology
Enhanced durability of a Zika virus self-amplifying RNA vaccine through combinatorial OX40 and 4-1BB agonism.
In JCI Insight on 22 May 2025 by Lu, H. H., dos Santos Alves, R. P., et al.
PubMed
The SARS-CoV-2 pandemic highlighted the potential of mRNA vaccines in rapidly responding to emerging pathogens. However, immunity induced by conventional mRNA vaccines wanes quickly, requiring frequent boosters. Self-amplifying RNA (saRNA) vaccines, which extend antigen expression via self-replication, offer a promising strategy to induce more durable immune responses. In this study, we developed an saRNA vaccine encoding Zika virus (ZIKV) membrane and envelope proteins and evaluated its efficacy in mice. A single vaccination elicited strong humoral and cellular immune responses and reduced viral loads but only for 28 days. By day 84, antibody titers and T cell responses had significantly declined, resulting in reduced efficacy. To address this, we evaluated agonist antibodies targeting the T cell costimulatory molecules OX40 and 4-1BB. Coadministration of agonist antibodies enhanced CD8+ T cell responses to vaccination, resulting in sustained immunity and reduced viral loads at day 84. Depletion and passive transfer studies verified that long-term antiviral immunity was primarily CD8+ T cell dependent, with minimal contributions from antibody responses. These findings suggest that agonists targeting members of the tumor necrosis receptor superfamily, such as OX40 and 4-1BB, might enhance the durability of saRNA vaccine-induced protection, addressing a key limitation of current mRNA vaccine platforms.
-
-
-
Cancer Research
-
Immunology and Microbiology
Sindbis Virus Platform Provides an Oncolytic-Virus-Mediated and Immunotherapeutic Strategy to Overcome the Challenging Microenvironment of Pancreatic Cancer.
In Pharmaceuticals (Basel) on 15 May 2025 by Opp, S., Pampeno, C., et al.
PubMed
Background/Objectives: Our laboratory has been developing a Sindbis viral (SV) vector platform for treatments of several types of cancers. In this study, we assess treatment efficacy for metastatic and immunosuppressive pancreatic cancer. Methods: Orthotopic mouse models were generated by injection of tumor cells into the pancreatic parenchyma. Sindbis vectors were inoculated intraperitoneally. Imaging of tumors was performed by either MRI or in vivo imaging using luciferase. Flow cytometry, multi-immunofluorescence and elispot analysis were performed for certain tumors. Results: SV can infect and reduce pancreatic tumors in three mouse model systems: a model bearing human pancreatic tumors, a highly metastatic model, and a model that reflects the highly immunosuppressive, desmoplastic microenvironment common to human pancreatic cancer. Conclusions: Combination of SV vector expressing IL12 with an immune co-stimulatory agent, anti-OX40, can reduce tumors, facilitate an influx of immune response cells into the tumor microenvironment, and prevent tumors in mice rechallenged with tumor cells promising an effective treatment for pancreatic cancer.
-
-
Single-cell and chromatin accessibility profiling reveals regulatory programs of pathogenic Th2 cells in allergic asthma.
In Nat Commun on 15 March 2025 by Khan, M., Alteneder, M., et al.
PubMed
Lung pathogenic T helper type 2 (pTh2) cells are important in mediating allergic asthma, but fundamental questions remain regarding their heterogeneity and epigenetic regulation. Here we investigate immune regulation in allergic asthma by single-cell RNA sequencing in mice challenged with house dust mite, in the presence and absence of histone deacetylase 1 (HDAC1) function. Our analyses indicate two distinct highly proinflammatory subsets of lung pTh2 cells and pinpoint thymic stromal lymphopoietin (TSLP) and Tumour Necrosis Factor Receptor Superfamily (TNFRSF) members as important drivers to generate pTh2 cells in vitro. Using our in vitro model, we uncover how signalling via TSLP and a TNFRSF member shapes chromatin accessibility at the type 2 cytokine gene loci by modulating HDAC1 repressive function. In summary, we have generated insights into pTh2 cell biology and establish an in vitro model for investigating pTh2 cells that proves useful for discovering molecular mechanisms involved in pTh2-mediated allergic asthma.
-
-
Immunology and Microbiology
-
Cancer Research
Endothelial OX40 activation facilitates tumor cell escape from T cell surveillance through S1P/YAP-mediated angiogenesis.
In J Clin Invest on 3 March 2025 by He, B., Zhao, R., et al.
PubMed
Understanding the complexity of the tumor microenvironment is vital for improving immunotherapy outcomes. Here, we report that the T cell costimulatory molecule OX40 was highly expressed in tumor endothelial cells (ECs) and was negatively associated with the prognosis of patients, which is irrelevant to T cell activation. Analysis of conditional OX40 loss- and gain-of-function transgenic mice showed that OX40 signal in ECs counteracted the antitumor effects produced in T cells by promoting angiogenesis. Mechanistically, leucine-rich repeat-containing GPCR5 (Lgr5+ ) cancer stem cells induced OX40 expression in tumor ECs via EGF/STAT3 signaling. Activated OX40 interacted with Spns lysolipid transporter 2 (Spns2), obstructing the export of sphingosine 1-phosphate (S1P) and resulting in S1P intracellular accumulation. Increased S1P directly bound to Yes 1-associated protein (YAP), disrupting its interaction with large tumor suppressor kinase 1 (LATS1) and promoting YAP nuclear translocation. Finally, the YAP inhibitor verteporfin enhanced the antitumor effects of the OX40 agonist. Together, these findings reveal an unexpected protumor role of OX40 in ECs, highlighting the effect of nonimmune cell compartments on immunotherapy.
-
-
-
Cancer Research
-
Immunology and Microbiology
Developing an Effective Therapeutic HPV Vaccine to Eradicate Large Tumors by Genetically Fusing Xcl1 and Incorporating IL-9 as Molecular Adjuvants.
In Vaccines (Basel) on 9 January 2025 by Sun, Z., Wu, Z., et al.
PubMed
Human papillomavirus (HPV) is a prevalent infection affecting both men and women, leading to various cytological lesions. Therapeutic vaccines mount a HPV-specific CD8+ cytotoxic T lymphocyte response, thus clearing HPV-infected cells. However, no therapeutic vaccines targeting HPV are currently approved for clinical treatment due to limited efficacy. Our goal is to develop a vaccine that can effectively eliminate tumors caused by HPV.
-
-
-
Mus musculus (Mouse)
-
Biochemistry and Molecular biology
Endothelial Immunosuppression in Atherosclerosis : Translational Control by Elavl1/HuR
In bioRxiv on 4 August 2024 by Nicholas, S. E., Helming, S. R., et al.
-
-
-
Flow cytometry/Cell sorting
-
Flow cytometry/Cell sorting
-
Mus musculus (Mouse)
Therapeutic potential of co-signaling receptor modulation in hepatitis B.
In Cell on 25 July 2024 by Andreata, F., Laura, C., et al.
PubMed
Reversing CD8+ T cell dysfunction is crucial in treating chronic hepatitis B virus (HBV) infection, yet specific molecular targets remain unclear. Our study analyzed co-signaling receptors during hepatocellular priming and traced the trajectory and fate of dysfunctional HBV-specific CD8+ T cells. Early on, these cells upregulate PD-1, CTLA-4, LAG-3, OX40, 4-1BB, and ICOS. While blocking co-inhibitory receptors had minimal effect, activating 4-1BB and OX40 converted them into antiviral effectors. Prolonged stimulation led to a self-renewing, long-lived, heterogeneous population with a unique transcriptional profile. This includes dysfunctional progenitor/stem-like (TSL) cells and two distinct dysfunctional tissue-resident memory (TRM) populations. While 4-1BB expression is ubiquitously maintained, OX40 expression is limited to TSL. In chronic settings, only 4-1BB stimulation conferred antiviral activity. In HBeAg+ chronic patients, 4-1BB activation showed the highest potential to rejuvenate dysfunctional CD8+ T cells. Targeting all dysfunctional T cells, rather than only stem-like precursors, holds promise for treating chronic HBV infection.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
Impact of isotype on the mechanism of action of agonist anti-OX40 antibodies in cancer: implications for therapeutic combinations.
In J Immunother Cancer on 4 July 2024 by Willoughby, J. E., Dou, L., et al.
PubMed
OX40 has been widely studied as a target for immunotherapy with agonist antibodies taken forward into clinical trials for cancer where they are yet to show substantial efficacy. Here, we investigated potential mechanisms of action of anti-mouse (m) OX40 and anti-human (h) OX40 antibodies, including a clinically relevant monoclonal antibody (mAb) (GSK3174998) and evaluated how isotype can alter those mechanisms with the aim to develop improved antibodies for use in rational combination treatments for cancer.
-
-
-
Cancer Research
-
Immunology and Microbiology
Nano-Pulse Stimulation Treatment Inhibits Pan02 Murine Pancreatic Tumor Growth and Induces a Long-Term Adaptive Immune Response with Abscopal Effects When Combined with Immune-Enhancing Agents.
In Bioelectricity on 1 June 2024 by McDaniel, A., Rothstein, K. V., et al.
PubMed
Pancreatic cancer is associated with a poor prognosis and immunotherapy alone has not demonstrated sufficient efficacy in the treatment of nonresectable tumors. Nano-Pulse Stimulation™ therapy (NPS™) applies nanosecond electric pulses that lead to regulated cell death, exposing tumor antigen to the immune system. To establish a primary Pan02 tumor, mice were intradermally injected with Pan02 cells into the right flank. Secondary, rechallenge tumors and distal, secondary tumors (abscopal response) were established by injecting Pan02 cells into the opposite left flank. After 5 days of tumor growth, one of the tumors was treated with NPS, followed by injection with an immune-enhancing agent to stimulate an immune response. Growth of the treated primary tumor and untreated rechallenge tumors (injected 60-days post-treatment) or distal secondary tumors (injected simultaneously with the primary) was monitored. NPS in combination with the adjuvant and TLR agonist, resiquimod (RES), was the optimal treatment regimen for both eliminating a primary Pan02 tumor as well as inhibiting growth of a Pan02 cell rechallenge tumor. This inhibition of the rechallenge tumor injected 2 months after eliminating the primary tumor suggests a long-term immune response had been stimulated. Additional support for this came from the observations that depleting CD8+ T-cells reduced inhibition of rechallenge tumor growth by 35% and rechallenge tumors had 3-fold more CD8+ T-cells than tumors injected after surgical resection of the primary tumor. When the NPS-treated tumor was immediately injected with the anti-OX40 antibody to agonize the function of the costimulatory T cell receptor, OX40, up to 80% of untreated abscopal tumors were eliminated. NPS plus RES was the most effective at both eliminating a primary tumor and inhibiting a rechallenge tumor. NPS treatment followed by injection of aOX40 was the most effective at inhibiting the growth of an untreated abscopal tumor.
-
-
-
Cancer Research
-
Immunology and Microbiology
OX40 expressed in endothelial cells facilitates tumor cells to escape from T-cell surveillance through S1P-YAP axis
In Research Square on 14 May 2024 by Zhang, B., He, B., et al.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Recently activated CD4 T cells in tuberculosis express OX40 as a target for host-directed immunotherapy.
In Nat Commun on 19 December 2023 by Gress, A. R., Ronayne, C. E., et al.
PubMed
After Mycobacterium tuberculosis (Mtb) infection, many effector T cells traffic to the lungs, but few become activated. Here we use an antigen receptor reporter mouse (Nur77-GFP) to identify recently activated CD4 T cells in the lungs. These Nur77-GFPHI cells contain expanded TCR clonotypes, have elevated expression of co-stimulatory genes such as Tnfrsf4/OX40, and are functionally more protective than Nur77-GFPLO cells. By contrast, Nur77-GFPLO cells express markers of terminal exhaustion and cytotoxicity, and the trafficking receptor S1pr5, associated with vascular localization. A short course of immunotherapy targeting OX40+ cells transiently expands CD4 T cell numbers and shifts their phenotype towards parenchymal protective cells. Moreover, OX40 agonist immunotherapy decreases the lung bacterial burden and extends host survival, offering an additive benefit to antibiotics. CD4 T cells from the cerebrospinal fluid of humans with HIV-associated tuberculous meningitis commonly express surface OX40 protein, while CD8 T cells do not. Our data thus propose OX40 as a marker of recently activated CD4 T cells at the infection site and a potential target for immunotherapy in tuberculosis.
-
-
-
Cancer Research
-
Immunology and Microbiology
Enzyme-mediated depletion of methylthioadenosine restores T cell function in MTAP-deficient tumors and reverses immunotherapy resistance.
In Cancer Cell on 9 October 2023 by Gjuka, D., Adib, E., et al.
PubMed
Chromosomal region 9p21 containing tumor suppressors CDKN2A/B and methylthioadenosine phosphorylase (MTAP) is one of the most frequent genetic deletions in cancer. 9p21 loss is correlated with reduced tumor-infiltrating lymphocytes (TILs) and resistance to immune checkpoint inhibitor (ICI) therapy. Previously thought to be caused by CDKN2A/B loss, we now show that it is loss of MTAP that leads to poor outcomes on ICI therapy and reduced TIL density. MTAP loss causes accumulation of methylthioadenosine (MTA) both intracellularly and extracellularly and profoundly impairs T cell function via the inhibition of protein arginine methyltransferase 5 (PRMT5) and by adenosine receptor agonism. Administration of MTA-depleting enzymes reverses this immunosuppressive effect, increasing TILs and drastically impairing tumor growth and importantly, synergizes well with ICI therapy. As several studies have shown ICI resistance in 9p21/MTAP null/low patients, we propose that MTA degrading therapeutics may have substantial therapeutic benefit in these patients by enhancing ICI effectiveness.
-
-
-
Cancer Research
-
Cardiovascular biology
-
Immunology and Microbiology
-
Mus musculus (Mouse)
Fasting mimicking diet in mice delays cancer growth and reduces immunotherapy-associated cardiovascular and systemic side effects.
In Nat Commun on 8 September 2023 by Cortellino, S., Quagliariello, V., et al.
PubMed
Immune checkpoint inhibitors cause side effects ranging from autoimmune endocrine disorders to severe cardiotoxicity. Periodic Fasting mimicking diet (FMD) cycles are emerging as promising enhancers of a wide range of cancer therapies including immunotherapy. Here, either FMD cycles alone or in combination with anti-OX40/anti-PD-L1 are much more effective than immune checkpoint inhibitors alone in delaying melanoma growth in mice. FMD cycles in combination with anti-OX40/anti-PD-L1 also show a trend for increased effects against a lung cancer model. As importantly, the cardiac fibrosis, necrosis and hypertrophy caused by immune checkpoint inhibitors are prevented/reversed by FMD treatment in both cancer models whereas immune infiltration of CD3+ and CD8+ cells in myocardial tissues and systemic and myocardial markers of oxidative stress and inflammation are reduced. These results indicate that FMD cycles in combination with immunotherapy can delay cancer growth while reducing side effects including cardiotoxicity.
-
-
-
Mus musculus (Mouse)
Single-cell profiling uncovers regulatory programs of pathogenic Th2 cells in allergic asthma
In bioRxiv on 14 August 2023 by Khan, M., Alteneder, M., et al.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Radioactive-immunoassays
Curcumin Enhances the Abscopal Effect in Mice with Colorectal Cancer by Acting as an Immunomodulator.
In Pharmaceutics on 17 May 2023 by Shih, K. C., Chan, H. W., et al.
PubMed
Radiotherapy (RT) is an effective cancer treatment. The abscopal effect, referring to the unexpected shrinkage observed in non-irradiated tumors after radiation therapy, is thought to be mediated by systemic immune activation. However, it has low incidence and is unpredictable. Here, RT was combined with curcumin to investigate how curcumin affects RT-induced abscopal effects in mice with bilateral CT26 colorectal tumors. Indium 111-labeled DOTA-anti-OX40 mAb was synthesized to detect the activated T cell accumulations in primary and secondary tumors correlating with the changes in protein expressions and tumor growth to understand the overall effects of the combination of RT and curcumin. The combination treatment caused the most significant tumor suppression in both primary and secondary tumors, accompanied by the highest 111In-DOTA-OX40 mAb tumor accumulations. The combination treatment elevated expressions of proapoptotic proteins (Bax and cleaved caspase-3) and proinflammatory proteins (granzyme B, IL-6, and IL-1β) in both primary and secondary tumors. Based on the biodistribution of 111In-DOTA-OX40 mAb, tumor growth inhibition, and anti-tumor protein expression, our findings suggest that curcumin could act as an immune booster to augment RT-induced anti-tumor and abscopal effects effectively.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Dendritic cell therapy augments antitumor immunity triggered by CDK4/6 inhibition and immune checkpoint blockade by unleashing systemic CD4 T-cell responses.
In J Immunother Cancer on 1 May 2023 by Kumar, A., Ramani, V., et al.
PubMed
Cyclin-dependent kinase 4/6 inhibitors (CDK4/6i) combined with endocrine therapy are a mainstay treatment for hormone receptor-positive breast cancer. While their principal mechanism is inhibition of cancer cell proliferation, preclinical and clinical evidence suggests that CDK4/6i can also promote antitumor T-cell responses. However, this pro-immunogenic property is yet to be successfully harnessed in the clinic, as combining CDK4/6i with immune checkpoint blockade (ICB) has not shown a definitive benefit in patients.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Multiagent Intratumoral Immunotherapy Can Be Effective in A20 Lymphoma Clearance and Generation of Systemic T Cell Immunity.
In Cancers (Basel) on 24 March 2023 by Gilman, K. E., Matiatos, A. P., et al.
PubMed
The use of immunotherapies has shown promise against selective human cancers. Identifying novel combinations of innate and adaptive immune cell-activating agents that can work synergistically to suppress tumor growth and provide additional protection against resistance or recurrence is critical. The A20 murine lymphoma model was used to evaluate the effect of various combination immunotherapies administered intratumorally. We show that single-modality treatment with Poly(I:C) or GM-CSF-secreting allogeneic cells only modestly controls tumor growth, whereas when given together there is an improved benefit, with 50% of animals clearing tumors and surviving long-term. Neither heat nor irradiation of GM-CSF-secreting cells enhanced the response over use of live cells. The use of a TIM-3 inhibitory antibody and an OX40 agonist in combination with Poly(I:C) allowed for improved tumor control, with 90% of animals clearing tumors with or without a combination of GM-CSF-secreting cells. Across all treatment groups, mice rejecting their primary A20 tumors were immune to subsequent challenge with A20, and this longstanding immunity was T-cell dependent. The results herein support the use of combinations of innate and adaptive immune activating agents for immunotherapy against lymphoma and should be investigated in other cancer types.
-
-
-
Cancer Research
-
Immunology and Microbiology
-
Mus musculus (Mouse)
Targeting T cell checkpoints 41BB and LAG3 and myeloid cell CXCR1/CXCR2 results in antitumor immunity and durable response in pancreatic cancer.
In Nat Cancer on 1 January 2023 by Gulhati, P., Schalck, A., et al.
PubMed
Pancreatic ductal adenocarcinoma (PDAC) is considered non-immunogenic, with trials showing its recalcitrance to PD1 and CTLA4 immune checkpoint therapies (ICTs). Here, we sought to systematically characterize the mechanisms underlying de novo ICT resistance and to identify effective therapeutic options for PDAC. We report that agonist 41BB and antagonist LAG3 ICT alone and in combination, increased survival and antitumor immunity, characterized by modulating T cell subsets with antitumor activity, increased T cell clonality and diversification, decreased immunosuppressive myeloid cells and increased antigen presentation/decreased immunosuppressive capability of myeloid cells. Translational analyses confirmed the expression of 41BB and LAG3 in human PDAC. Since single and dual ICTs were not curative, T cell-activating ICTs were combined with a CXCR1/2 inhibitor targeting immunosuppressive myeloid cells. Triple therapy resulted in durable complete responses. Given similar profiles in human PDAC and the availability of these agents for clinical testing, our findings provide a testable hypothesis for this lethal disease.
-
-
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
Potent and Targeted Sindbis Virus Platform for Immunotherapy of Ovarian Cancer.
In Cells on 24 December 2022 by Opp, S., Hurtado, A., et al.
PubMed
Our laboratory has been developing a Sindbis viral (SV) vector platform for treatments of ovarian and other types of cancers. In this study we show that SV.IL-12 combined with an agonistic OX40 antibody can eliminate ovarian cancer in a Mouse Ovarian Surface Epithelial Cell Line (MOSEC) model and further prevent tumors in mice rechallenged with tumor cells after approximately 5 months. Treatment efficacy is shown to be dependent upon T-cells that are transcriptionally and metabolically reprogramed. An influx of immune cells to the tumor microenvironment occurs. Combination of sequences encoding both IL-12 and anti-OX40 into a single SV vector, SV.IgGOX40.IL-12, facilitates the local delivery of immunoregulatory agents to tumors enhancing the anti-tumor response. We promote SV.IgGOX40.IL-12 as a safe and effective therapy for multiple types of cancer.
-
-
-
Mass Spectrometry
-
Cancer Research
-
Immunology and Microbiology
-
Mass Spectrometry
-
Mus musculus (Mouse)
Stromal Reprogramming by FAK Inhibition Overcomes Radiation Resistance to Allow for Immune Priming and Response to Checkpoint Blockade.
In Cancer Discov on 2 December 2022 by Krisnawan, V. E., Belle, J. I., et al.
PubMed
The effects of radiotherapy (RT) on tumor immunity in pancreatic ductal adenocarcinoma (PDAC) are not well understood. To better understand if RT can prime antigen-specific T-cell responses, we analyzed human PDAC tissues and mouse models. In both settings, there was little evidence of RT-induced T-cell priming. Using in vitro systems, we found that tumor-stromal components, including fibroblasts and collagen, cooperate to blunt RT efficacy and impair RT-induced interferon signaling. Focal adhesion kinase (FAK) inhibition rescued RT efficacy in vitro and in vivo, leading to tumor regression, T-cell priming, and enhanced long-term survival in PDAC mouse models. Based on these data, we initiated a clinical trial of defactinib in combination with stereotactic body RT in patients with PDAC (NCT04331041). Analysis of PDAC tissues from these patients showed stromal reprogramming mirroring our findings in genetically engineered mouse models. Finally, the addition of checkpoint immunotherapy to RT and FAK inhibition in animal models led to complete tumor regression and long-term survival.
-