InVivoMAb anti-mouse IL-18
Product Description
Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Not available or unknown |
| Reported Applications |
in vivo IL-18 neutralization in vitro IL-18 neutralization in vitro Organoids/Organ-on-Chip |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2687719 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vitro Organoids/Organ-on-Chip
Parsa R, London M, Rezende de Castro TB, Reis B, Buissant des Amorie J, Smith JG, Mucida D (2022). "Newly recruited intraepithelial Ly6A+CCR9+CD4+ T cells protect against enteric viral infection" Immunity 55(7):1234-1
PubMed
The intestinal epithelium comprises the body's largest surface exposed to viruses. Additionally, the gut epithelium hosts a large population of intraepithelial T lymphocytes, or IELs, although their role in resistance against viral infections remains elusive. By fate-mapping T cells recruited to the murine intestine, we observed an accumulation of newly recruited CD4+ T cells after infection with murine norovirus CR6 and adenovirus type-2 (AdV), but not reovirus. CR6- and AdV-recruited intraepithelial CD4+ T cells co-expressed Ly6A and chemokine receptor CCR9, exhibited T helper 1 and cytotoxic profiles, and conferred protection against AdV in vivo and in an organoid model in an IFN-γ-dependent manner. Ablation of the T cell receptor (TCR) or the transcription factor ThPOK in CD4+ T cells prior to AdV infection prevented viral control, while TCR ablation during infection did not impact viral clearance. These results uncover a protective role for intraepithelial Ly6A+CCR9+CD4+ T cells against enteric adenovirus.
in vitro Organoids/Organ-on-Chip
Parsa R, London M, Rezende de Castro TB, Reis B, Buissant des Amorie J, Smith JG, Mucida D (2022). "Newly recruited intraepithelial Ly6A+CCR9+CD4+ T cells protect against enteric viral infection" Immunity 55(7):1234-1
PubMed
The intestinal epithelium comprises the body's largest surface exposed to viruses. Additionally, the gut epithelium hosts a large population of intraepithelial T lymphocytes, or IELs, although their role in resistance against viral infections remains elusive. By fate-mapping T cells recruited to the murine intestine, we observed an accumulation of newly recruited CD4+ T cells after infection with murine norovirus CR6 and adenovirus type-2 (AdV), but not reovirus. CR6- and AdV-recruited intraepithelial CD4+ T cells co-expressed Ly6A and chemokine receptor CCR9, exhibited T helper 1 and cytotoxic profiles, and conferred protection against AdV in vivo and in an organoid model in an IFN-γ-dependent manner. Ablation of the T cell receptor (TCR) or the transcription factor ThPOK in CD4+ T cells prior to AdV infection prevented viral control, while TCR ablation during infection did not impact viral clearance. These results uncover a protective role for intraepithelial Ly6A+CCR9+CD4+ T cells against enteric adenovirus.
in vivo IL-18 neutralization
Cohen, T. S., et al (2018). "S. aureus Evades Macrophage Killing through NLRP3-Dependent Effects on Mitochondrial Trafficking" Cell Rep 22(9): 2431-2441.
PubMed
Clinical severity of Staphylococcus aureus respiratory infection correlates with alpha toxin (AT) expression. AT activates the NLRP3 inflammasome; deletion of Nlrp3, or AT neutralization, protects mice from lethal S. aureus pneumonia. We tested the hypothesis that this protection is not due to a reduction in inflammasome-dependent cytokines (IL-1beta/IL-18) but increased bactericidal function of macrophages. In vivo, neutralization of AT or NLRP3 improved bacterial clearance and survival, while blocking IL-1beta/IL-18 did not. Primary human monocytes were used in vitro to determine the mechanism through which NLRP3 alters bacterial killing. In cells treated with small interfering RNA (siRNA) targeting NLRP3 or infected with AT-null S. aureus, mitochondria co-localize with bacterial-containing phagosomes. Mitochondrial engagement activates caspase-1, a process dependent on complex II of the electron transport chain, near the phagosome, promoting its acidification. These data demonstrate a mechanism utilized by S. aureus to sequester itself from antimicrobial processes within the cell.
in vivo IL-18 neutralization
Robinson, K. M., et al (2018). "The inflammasome potentiates influenza/Staphylococcus aureus superinfection in mice" JCI Insight 3(7).
PubMed
Secondary bacterial respiratory infections are commonly associated with both acute and chronic lung injury. Influenza complicated by bacterial pneumonia is an effective model to study host defense during pulmonary superinfection due to its clinical relevance. Multiprotein inflammasomes are responsible for IL-1β production in response to infection and drive tissue inflammation. In this study, we examined the role of the inflammasome during viral/bacterial superinfection. We demonstrate that ASC-/- mice are protected from bacterial superinfection and produce sufficient quantities of IL-1β through an apoptosis-associated speck-like protein containing CARD (ASC) inflammasome-independent mechanism. Despite the production of IL-1β by ASC-/- mice in response to bacterial superinfection, these mice display decreased lung inflammation. A neutrophil elastase inhibitor blocked ASC inflammasome-independent production of IL-1β and the IL-1 receptor antagonist, anakinra, confirmed that IL-1 remains crucial to the clearance of bacteria during superinfection. Delayed inhibition of NLRP3 during influenza infection by MCC950 decreases bacterial burden during superinfection and leads to decreased inflammatory cytokine production. Collectively, our results demonstrate that ASC augments the clearance of bacteria, but can also contribute to inflammation and mortality. ASC should be considered as a therapeutic target to decrease morbidity and mortality during bacterial superinfection.
in vivo IL-18 neutralization
in vitro IL-18 neutralization
Molgora, M., et al (2017). "IL-1R8 is a checkpoint in NK cells regulating anti-tumour and anti-viral activity" Nature 551(7678): 110-114.
PubMed
Interleukin-1 receptor 8 (IL-1R8, also known as single immunoglobulin IL-1R-related receptor, SIGIRR, or TIR8) is a member of the IL-1 receptor (ILR) family with distinct structural and functional characteristics, acting as a negative regulator of ILR and Toll-like receptor (TLR) downstream signalling pathways and inflammation. Natural killer (NK) cells are innate lymphoid cells which mediate resistance against pathogens and contribute to the activation and orientation of adaptive immune responses. NK cells mediate resistance against haematopoietic neoplasms but are generally considered to play a minor role in solid tumour carcinogenesis. Here we report that IL-1R8 serves as a checkpoint for NK cell maturation and effector function. Its genetic blockade unleashes NK-cell-mediated resistance to hepatic carcinogenesis, haematogenous liver and lung metastasis, and cytomegalovirus infection.
in vivo IL-18 neutralization
Chudnovskiy, A., et al (2016). "Host-Protozoan Interactions Protect from Mucosal Infections through Activation of the Inflammasome" Cell 167(2): 444-456 e414.
PubMed
While conventional pathogenic protists have been extensively studied, there is an underappreciated constitutive protist microbiota that is an integral part of the vertebrate microbiome. The impact of these species on the host and their potential contributions to mucosal immune homeostasis remain poorly studied. Here, we show that the protozoan Tritrichomonas musculis activates the host epithelial inflammasome to induce IL-18 release. Epithelial-derived IL-18 promotes dendritic cell-driven Th1 and Th17 immunity and confers dramatic protection from mucosal bacterial infections. Along with its role as a “protistic” antibiotic, colonization with T. musculis exacerbates the development of T-cell-driven colitis and sporadic colorectal tumors. Our findings demonstrate a novel mutualistic host-protozoan interaction that increases mucosal host defenses at the cost of an increased risk of inflammatory disease.
Product Citations
-
-
Immunology and Microbiology
Damage-induced IL-18 stimulates thymic NK cells limiting endogenous tissue regeneration.
In Nat Immunol on 1 October 2025 by Granadier, D., Cooper, K., et al.
PubMed
Interleukin-18 (IL-18) is an acute-phase proinflammatory molecule crucial for mediating viral clearance by activating T helper 1 CD4+ T cells, cytotoxic CD8+ T cells and natural killer (NK) cells. Here, we show that mature IL-18 is generated in the thymus following numerous distinct forms of tissue damage, all of which cause caspase-1-mediated immunogenic cell death. We report that IL-18-stimulated cytotoxic NK cells limit endogenous thymic regeneration, a critical process that ensures the restoration of immune competence after acute insults such as stress, infection, chemotherapy and radiation. NK cells suppress thymus recovery by aberrantly targeting thymic epithelial cells, which act as the master regulators of organ function and regeneration. Together, our data reveal a new pathway regulating tissue regeneration in the thymus and suggest IL-18 as a potential therapeutic target to boost thymic function. Moreover, given the enthusiasm for IL-18 as a cancer immunotherapy due to its capacity to elicit a type 1 immune response, these findings also offer insight into potential off-target effects.
-
-
Macrophages orchestrate elimination of Shigella from the intestinal epithelial cell niche via TLR-induced IL-12 and IFN-γ.
In Cell Host Microbe on 10 September 2025 by Eislmayr, K. D., Nichols, C. A., et al.
PubMed
Bacteria of the genus Shigella replicate in intestinal epithelial cells and cause shigellosis, a severe diarrheal disease that resolves spontaneously in most healthy individuals. During shigellosis, neutrophils are abundantly recruited to the gut and have long been thought to be central to Shigella control and pathogenesis. However, how shigellosis resolves remains poorly understood due to the longstanding lack of a tractable and physiological animal model. Here, using our newly developed Nlrc4-/-Casp11-/- mouse model of shigellosis, we unexpectedly find no major role for neutrophils in limiting Shigella or in disease pathogenesis. Instead, we uncover an essential role for macrophages in the host control of Shigella. Macrophages respond to Shigella via Toll-like receptors (TLRs) to produce IL-12, which then induces IFN-γ, a cytokine that is essential to control Shigella replication in intestinal epithelial cells. Collectively, our findings reshape our understanding of the innate immune response to Shigella.
-
-
Mus musculus (Mouse)
Macrophages orchestrate elimination ofShigellafrom the intestinal epithelial cell niche via TLR-induced IL-12 and IFN-γ
In bioRxiv on 22 January 2025 by Eislmayr, K. D., Langner, C., et al.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Heightened innate immune state induced by viral vector leads to enhanced response to challenge and prolongs malaria vaccine protection.
In iScience on 20 December 2024 by Gbédandé, K., Ibitokou, S. A., et al.
PubMed
Cytomegalovirus is a promising vaccine vector; however, mechanisms promoting CD4 T cell responses to challenge, by CMV as a vector, are unknown. The ability of MCMV to prolong immunity generated by short-lived malaria vaccine was tested. MCMV provided non-specific protection to challenge with Plasmodium and increased interleukin-12 (IL-12) and CD8α+ dendritic cell (DC) numbers through prolonged MCMV-dependent interferon gamma (IFN-γ) production. This late innate response to MCMV increased IL-12 upon challenge and increased the polyclonal CD4 effector T cell response to Plasmodium, protecting in an IL-12-dependent manner. Although Plasmodium-vaccine-induced protection decayed by d200, MCMV restored protection through IFN-γ. Mechanistically, protection depended on MCMV-induced-IFN-γ increasing CD8α+ DCs and IL-12p40. MCMV expressing a Plasmodium epitope increased parasite-specific CD4 effector and effector memory T cells persisting after malaria vaccination, both phenotypes reported to protect. Overall, enhanced innate cell status, a mechanism of heterologous protection by MCMV, led to a stronger T cell response to challenge.
-
-
Damage-induced IL-18 stimulates thymic NK Cells limiting endogenous tissue regeneration
In bioRxiv on 30 September 2024 by Granadier, D., Cooper, K., et al.
-
-
Cancer Research
Development of NR0B2 as a therapeutic target for the re-education of tumor associated myeloid cells.
In Cancer Lett on 10 August 2024 by Vidana Gamage, H. E., Albright, S. T., et al.
PubMed
Immune checkpoint blockade (ICB) has had limited utility in several solid tumors such as breast cancer, a major cause of cancer-related mortality in women. Therefore, there is considerable interest in alternate strategies to promote an anti-cancer immune response. A paper co-published in this issue describes how NR0B2, a protein involved in cholesterol homeostasis, functions within myeloid immune cells to modulate the inflammasome and reduce the expansion of immune-suppressive regulatory T cells (Treg). Here, we develop NR0B2 as a potential therapeutic target. NR0B2 in tumors is associated with improved survival for several cancer types including breast. Importantly, NR0B2 expression is also prognostic of ICB success. Within breast tumors, NR0B2 expression is inversely associated with FOXP3, a marker of Tregs. While a described agonist (DSHN) had some efficacy, it required high doses and long treatment times. Therefore, we designed and screened several derivatives. A methyl ester derivative (DSHN-OMe) emerged as superior in terms of (1) cellular uptake, (2) ability to regulate expected expression of genes, (3) suppression of Treg expansion using in vitro co-culture systems, and (4) efficacy against the growth of primary and metastatic tumors. This work identifies NR0B2 as a target to re-educate myeloid immune cells and a novel ligand with significant anti-tumor efficacy in preclinical models.
-
-
-
Immunology and Microbiology
-
Cancer Research
NR0B2 re-educates myeloid immune cells to reduce regulatory T cell expansion and progression of breast and other solid tumors.
In Cancer Lett on 10 August 2024 by Vidana Gamage, H. E., Shahoei, S. H., et al.
PubMed
Although survival from breast cancer has dramatically increased, many will develop recurrent, metastatic disease. Unfortunately, survival for this stage of disease remains very low. Activating the immune system has incredible promise since it has the potential to be curative. However, immune checkpoint blockade (ICB) which works through T cells has been largely disappointing for metastatic breast cancer. One reason for this is a suppressive myeloid immune compartment that is unaffected by ICB. Cholesterol metabolism and proteins involved in cholesterol homeostasis play important regulatory roles in myeloid cells. Here, we demonstrate that NR0B2, a nuclear receptor involved in negative feedback of cholesterol metabolism, works in several myeloid cell types to impair subsequent expansion of regulatory T cells (Tregs); Tregs being a subset known to be highly immune suppressive and associated with poor therapeutic response. Within myeloid cells, NR0B2 serves to decrease many aspects of the inflammasome, ultimately resulting in decreased IL1β; IL1β driving Treg expansion. Importantly, mice lacking NR0B2 exhibit accelerated tumor growth. Thus, NR0B2 represents an important node in myeloid cells dictating ensuing Treg expansion and tumor growth, thereby representing a novel therapeutic target to re-educate these cells, having impact across different solid tumor types. Indeed, a paper co-published in this issue demonstrates the therapeutic utility of targeting NR0B2.
-
-
-
Endocrinology and Physiology
Circadian-clock-controlled endocrine and cytokine signals regulate multipotential innate lymphoid cell progenitors in the bone marrow.
In Cell Rep on 28 May 2024 by Liu, Q., Tabrez, S., et al.
PubMed
Innate lymphoid cells (ILCs), strategically positioned throughout the body, undergo population declines over time. A solution to counteract this problem is timely mobilization of multipotential progenitors from the bone marrow. It remains unknown what triggers the mobilization of bone marrow ILC progenitors (ILCPs). We report that ILCPs are regulated by the circadian clock to emigrate and generate mature ILCs in the periphery. We found that circadian-clock-defective ILCPs fail to normally emigrate and generate ILCs. We identified circadian-clock-controlled endocrine and cytokine cues that, respectively, regulate the retention and emigration of ILCPs at distinct times of each day. Activation of the stress-hormone-sensing glucocorticoid receptor upregulates CXCR4 on ILCPs for their retention in the bone marrow, while the interleukin-18 (IL-18) and RORα signals upregulate S1PR1 on ILCPs for their mobilization to the periphery. Our findings establish important roles of circadian signals for the homeostatic efflux of bone marrow ILCPs.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Myeloid A20 is critical for alternative macrophage polarization and type-2 immune-mediated helminth resistance.
In Front Immunol on 29 April 2024 by Petta, I., Thorp, M., et al.
PubMed
Protective immunity against intestinal helminths requires induction of robust type-2 immunity orchestrated by various cellular and soluble effectors which promote goblet cell hyperplasia, mucus production, epithelial proliferation, and smooth muscle contractions to expel worms and re-establish immune homeostasis. Conversely, defects in type-2 immunity result in ineffective helminth clearance, persistent infection, and inflammation. Macrophages are highly plastic cells that acquire an alternatively activated state during helminth infection, but they were previously shown to be dispensable for resistance to Trichuris muris infection.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Low-Dose Chemotherapy Preferentially Shapes the Ileal Microbiome and Augments the Response to Immune Checkpoint Blockade by Activating AIM2 Inflammasome in Ileal Epithelial Cells.
In Adv Sci (Weinh) on 1 March 2024 by Pu, C., Li, Y., et al.
PubMed
Intervention of the gut microbiome is a promising adjuvant strategy in cancer immunotherapy. Chemotherapeutic agents are recognized for their substantial impacts on the gut microbiome, yet their therapeutic potential as microbiome modulators remains uncertain, due to the complexity of microbiome-host-drug interactions. Here, it is showed that low-dose chemotherapy preferentially shapes the ileal microbiome to augment the extraintestinal immune response to anti-programmed death-1 (anti-PD-1) therapy without causing intestinal toxicity. Mechanistically, low-dose chemotherapy causes DNA damage restricted to highly-proliferative ileal epithelial cells, resulting in the accumulation of cytosolic dsDNA and the activation of the absent in melanoma 2 (AIM2) inflammasome. AIM2-dependent IL-18 secretion triggers the interplay between proximal Th1 cells and Paneth cells in ileal crypts, impairing the local antimicrobial host defense and resulting in ileal microbiome change. Intestinal epithelium-specific knockout of AIM2 in mice significantly attenuates CPT-11-caused IL-18 secretion, Paneth cell dysfunction, and ileal microbiome alteration. Moreover, AIM2 deficiency in mice or antibiotic microbial depletion attenuates chemotherapy-augmented antitumor responses to anti-PD1 therapy. Collectively, these findings provide mechanistic insights into how chemotherapy-induced genomic stress is transduced to gut microbiome change and support the rationale of applying low-dose chemotherapy as a promising adjuvant strategy in cancer immunotherapy with minimal toxicity.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
A pairwise cytokine code explains the organism-wide response to sepsis.
In Nat Immunol on 1 February 2024 by Takahama, M., Patil, A., et al.
PubMed
Sepsis is a systemic response to infection with life-threatening consequences. Our understanding of the molecular and cellular impact of sepsis across organs remains rudimentary. Here, we characterize the pathogenesis of sepsis by measuring dynamic changes in gene expression across organs. To pinpoint molecules controlling organ states in sepsis, we compare the effects of sepsis on organ gene expression to those of 6 singles and 15 pairs of recombinant cytokines. Strikingly, we find that the pairwise effects of tumor necrosis factor plus interleukin (IL)-18, interferon-gamma or IL-1β suffice to mirror the impact of sepsis across tissues. Mechanistically, we map the cellular effects of sepsis and cytokines by computing changes in the abundance of 195 cell types across 9 organs, which we validate by whole-mouse spatial profiling. Our work decodes the cytokine cacophony in sepsis into a pairwise cytokine message capturing the gene, cell and tissue responses of the host to the disease.
-
-
-
Immunology and Microbiology
Fusobacterium nucleatum infection activates the noncanonical inflammasome and exacerbates inflammatory response in DSS-induced colitis.
In Eur J Immunol on 1 November 2023 by Boonyaleka, K., Okano, T., et al.
PubMed
Caspase activation results in pyroptosis, an inflammatory cell death that contributes to several inflammatory diseases by releasing inflammatory cytokines and cellular contents. Fusobacterium nucleatum is a periodontal pathogen frequently detected in human cancer and inflammatory bowel diseases. Studies have reported that F. nucleatum infection leads to NLRP3 activation and pyroptosis, but the precise activation process and disease association remain poorly understood. This study demonstrated that F. nucleatum infection exacerbates acute colitis in mice and activates pyroptosis through caspase-11-mediated gasdermin D cleavage in macrophages. Furthermore, F. nucleatum infection in colitis mice induces the enhancement of IL-1⍺ secretion from the colon, affecting weight loss and severe disease activities. Neutralization of IL-1⍺ protects F. nucleatum infected mice from severe colitis. Therefore, F. nucleatum infection facilitates inflammation in acute colitis with IL-1⍺ from colon tissue by activating noncanonical inflammasome through gasdermin D cleavage.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Myeloid A20 is critical for type-2 immune mediated helminth resistance
In bioRxiv on 7 September 2023 by Petta, I., Thorp, M., et al.
-
-
-
Immunology and Microbiology
A cytotoxic T cell inspired oncolytic nanosystem promotes lytic cell death by lipid peroxidation and elicits antitumor immune responses.
In Nat Commun on 6 September 2023 by Zuo, Z., Yin, H., et al.
PubMed
Lytic cell death triggers an antitumour immune response. However, cancer cells evade lytic cell death by several mechanisms. Moreover, a prolonged and uncontrolled immune response conversely leads to T-cell exhaustion. Therefore, an oncolytic system capable of eliciting an immune response by killing cancer cells in a controlled manner is needed. Here, we establish a micro-scale cytotoxic T-cell-inspired oncolytic system (TIOs) to precisely lyse cancer cells by NIR-light-controlled lipid peroxidation. Our TIOs present antigen-based cell recognition, tumour-targeting and catalytic cell-lysis ability; thus, the TIOs induce oncolysis in vivo. We apply TIOs to preclinical cancer models, showing anti-tumor activity with negligible side-effects. Tumour regression is correlated with a T-cell based anti-tumour immune response and TIOs also improve responses to anti-PD-1 therapy or STING activation. Our study provides insights to design oncolytic systems for antitumour immunity. Moreover, activation of STING can reverse T-cell exhaustion in oncolysis.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Re-education of myeloid immune cells to reduce regulatory T cell expansion and impede breast cancer progression
In bioRxiv on 14 August 2023 by Gamage, H. E. V., Shahoei, S. H., et al.
-
-
-
Immunology and Microbiology
NK cell-derived extracellular granzyme B drives epithelial ulceration during HSV-2 genital infection.
In Cell Rep on 25 April 2023 by Lim, Y. S., Lee, A. G., et al.
PubMed
Genital herpes is characterized by recurrent episodes of epithelial blistering. The mechanisms causing this pathology are ill defined. Using a mouse model of vaginal herpes simplex virus 2 (HSV-2) infection, we show that interleukin-18 (IL-18) acts upon natural killer (NK) cells to promote accumulation of the serine protease granzyme B in the vagina, coinciding with vaginal epithelial ulceration. Genetic loss of granzyme B or therapeutic inhibition by a specific protease inhibitor reduces disease and restores epithelial integrity without altering viral control. Distinct effects of granzyme B and perforin deficiency on pathology indicates that granzyme B acts independent of its classic cytotoxic role. IL-18 and granzyme B are markedly elevated in human herpetic ulcers compared with non-herpetic ulcers, suggesting engagement of these pathways in HSV-infected patients. Our study reveals a role for granzyme B in destructing mucosal epithelium during HSV-2 infection, identifying a therapeutic target to augment treatment of genital herpes.
-
-
-
Immunology and Microbiology
Organism-Wide Analysis of Sepsis Reveals Mechanisms of Systemic Inflammation
In bioRxiv on 2 February 2023 by Takahama, M., Patil, A., et al.
-
-
-
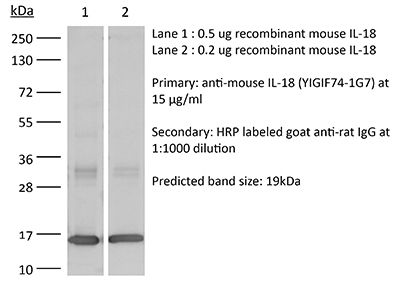
Western Blotting
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Alveolar macrophages instruct CD8+ T cell expansion by antigen cross-presentation in lung.
In Cell Rep on 13 December 2022 by Kawasaki, T., Ikegawa, M., et al.
PubMed
Lung CD8+ memory T cells play central roles in protective immunity to respiratory viruses, such as influenza A virus (IAV). Here, we find that alveolar macrophages (AMs) function as antigen-presenting cells that support the expansion of lung CD8+ memory T cells. Intranasal antigen administration to mice subcutaneously immunized with antigen results in a rapid expansion of antigen-specific CD8+ T cells in the lung, which is dependent on antigen cross-presentation by AMs. AMs highly express interleukin-18 (IL-18), which mediates subsequent formation of CD103+CD8+ resident memory T (TRM) cells in the lung. In a mouse model of IAV infection, AMs are required for expansion of virus-specific CD8+ T cells and CD103+CD8+ TRM cells and inhibiting virus replication in the lungs during secondary infection. These results suggest that AMs instruct a rapid expansion of antigen-specific CD8+ T cells in lung, which protect the host from respiratory virus infection.
-
-
-
Mus musculus (Mouse)
Integrated proteomic and transcriptomic landscape of macrophages in mouse tissues.
In Nat Commun on 30 November 2022 by Qie, J., Liu, Y., et al.
PubMed
Macrophages are involved in tissue homeostasis and are critical for innate immune responses, yet distinct macrophage populations in different tissues exhibit diverse gene expression patterns and biological processes. While tissue-specific macrophage epigenomic and transcriptomic profiles have been reported, proteomes of different macrophage populations remain poorly characterized. Here we use mass spectrometry and bulk RNA sequencing to assess the proteomic and transcriptomic patterns, respectively, of 10 primary macrophage populations from seven mouse tissues, bone marrow-derived macrophages and the cell line RAW264.7. The results show distinct proteomic landscape and protein copy numbers between tissue-resident and recruited macrophages. Construction of a hierarchical regulatory network finds cell-type-specific transcription factors of macrophages serving as hubs for denoting tissue and functional identity of individual macrophage subsets. Finally, Il18 is validated to be essential in distinguishing molecular signatures and cellular function features between tissue-resident and recruited macrophages in the lung and liver. In summary, these deposited datasets and our open proteome server ( http://macrophage.mouseprotein.cn ) integrating all information will provide a valuable resource for future functional and mechanistic studies of mouse macrophages.
-
-
-
Immunology and Microbiology
Excessive IL-10 and IL-18 trigger hemophagocytic lymphohistiocytosis-like hyperinflammation and enhanced myelopoiesis.
In J Allergy Clin Immunol on 1 November 2022 by Tang, Y., Xu, Q., et al.
PubMed
Hyperinflammation is a life-threatening condition associated with various clinical disorders characterized by excessive immune activation and tissue damage. Multiple cytokines promote the development of hyperinflammation; however, the contribution of IL-10 remains unclear despite emerging speculations for a pathological role. Clinical observations from hemophagocytic lymphohistiocytosis (HLH), a prototypical hyperinflammatory disease, suggest that IL-18 and IL-10 may collectively promote the onset of a hyperinflammatory state.
-