InVivoMAb anti-mouse IL-17A
Product Details
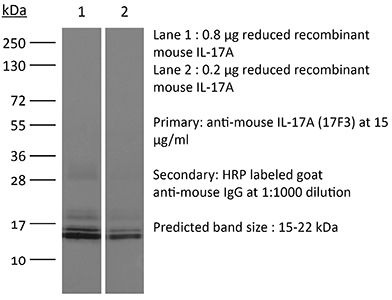
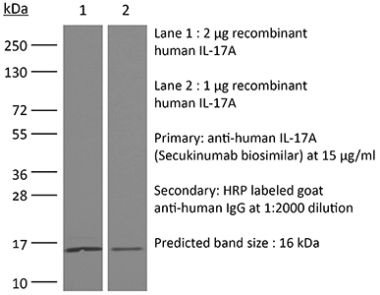
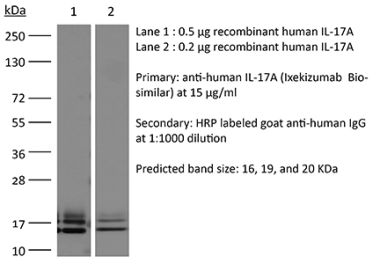
The 17F3 monoclonal antibody reacts with mouse IL-17A a 15-20 kDa cytokine expressed by Th17 cells, γδ T cells, iNKT cells, NK cells, LTi cells, neutrophils, and intestinal Paneth cells. IL-17A has pleiotropic effects in immunoregulation and inflammation. It plays an important role in anti-microbial and chronic inflammation by inducing cytokine and chemokine production, neutrophil influx, and the production of antibacterial peptides but it is also an inflammatory mediator in the development of autoimmune diseases including rheumatoid arthritis, asthma, multiple sclerosis, and psoriasis. The 17F3 antibody has been shown to neutralize IL-17A in vivo.Specifications
| Isotype | Mouse IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb mouse IgG1 isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Mouse IL-17A cross-linked to OVA |
| Reported Applications | in vivo IL-17A neutralization |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10950102 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo IL-17A neutralization
Faraco, G., et al. (2018). "Dietary salt promotes neurovascular and cognitive dysfunction through a gut-initiated TH17 response" Nat Neurosci 21(2): 240-249. PubMed
A diet rich in salt is linked to an increased risk of cerebrovascular diseases and dementia, but it remains unclear how dietary salt harms the brain. We report that, in mice, excess dietary salt suppresses resting cerebral blood flow and endothelial function, leading to cognitive impairment. The effect depends on expansion of TH17 cells in the small intestine, resulting in a marked increase in plasma interleukin-17 (IL-17). Circulating IL-17, in turn, promotes endothelial dysfunction and cognitive impairment by the Rho kinase-dependent inhibitory phosphorylation of endothelial nitric oxide synthase and reduced nitric oxide production in cerebral endothelial cells. The findings reveal a new gut-brain axis linking dietary habits to cognitive impairment through a gut-initiated adaptive immune response compromising brain function via circulating IL-17. Thus, the TH17 cell-IL-17 pathway is a putative target to counter the deleterious brain effects induced by dietary salt and other diseases associated with TH17 polarization.
in vivo IL-17A neutralization
Xiong, H., et al. (2016). "Innate Lymphocyte/Ly6C Monocyte Crosstalk Promotes Klebsiella Pneumoniae Clearance" Cell. doi : 10.1016/j.cell.2016.03.017. PubMed
Increasing antibiotic resistance among bacterial pathogens has rendered some infections untreatable with available antibiotics. Klebsiella pneumoniae, a bacterial pathogen that has acquired high-level antibiotic resistance, is a common cause of pulmonary infections. Optimal clearance of K. pneumoniae from the host lung requires TNF and IL-17A. Herein, we demonstrate that inflammatory monocytes are rapidly recruited to the lungs of K. pneumoniae-infected mice and produce TNF, which markedly increases the frequency of IL-17-producing innate lymphoid cells. While pulmonary clearance of K. pneumoniae is preserved in neutrophil-depleted mice, monocyte depletion or TNF deficiency impairs IL-17A-dependent resolution of pneumonia. Monocyte-mediated bacterial uptake and killing is enhanced by ILC production of IL-17A, indicating that innate lymphocytes engage in a positive-feedback loop with monocytes that promotes clearance of pneumonia. Innate immune defense against a highly antibiotic-resistant bacterial pathogen depends on crosstalk between inflammatory monocytes and innate lymphocytes that is mediated by TNF and IL-17A.
in vivo IL-17A neutralization
Naik, S., et al. (2015). "Commensal-dendritic-cell interaction specifies a unique protective skin immune signature" Nature 520(7545): 104-108. PubMed
The skin represents the primary interface between the host and the environment. This organ is also home to trillions of microorganisms that play an important role in tissue homeostasis and local immunity. Skin microbial communities are highly diverse and can be remodelled over time or in response to environmental challenges. How, in the context of this complexity, individual commensal microorganisms may differentially modulate skin immunity and the consequences of these responses for tissue physiology remains unclear. Here we show that defined commensals dominantly affect skin immunity and identify the cellular mediators involved in this specification. In particular, colonization with Staphylococcus epidermidis induces IL-17A(+) CD8(+) T cells that home to the epidermis, enhance innate barrier immunity and limit pathogen invasion. Commensal-specific T-cell responses result from the coordinated action of skin-resident dendritic cell subsets and are not associated with inflammation, revealing that tissue-resident cells are poised to sense and respond to alterations in microbial communities. This interaction may represent an evolutionary means by which the skin immune system uses fluctuating commensal signals to calibrate barrier immunity and provide heterologous protection against invasive pathogens. These findings reveal that the skin immune landscape is a highly dynamic environment that can be rapidly and specifically remodelled by encounters with defined commensals, findings that have profound implications for our understanding of tissue-specific immunity and pathologies.
in vivo IL-17A neutralization
Sell, S., et al. (2015). "Control of murine cytomegalovirus infection by gammadelta T cells" PLoS Pathog 11(2): e1004481. PubMed
Infections with cytomegalovirus (CMV) can cause severe disease in immunosuppressed patients and infected newborns. Innate as well as cellular and humoral adaptive immune effector functions contribute to the control of CMV in immunocompetent individuals. None of the innate or adaptive immune functions are essential for virus control, however. Expansion of gammadelta T cells has been observed during human CMV (HCMV) infection in the fetus and in transplant patients with HCMV reactivation but the protective function of gammadelta T cells under these conditions remains unclear. Here we show for murine CMV (MCMV) infections that mice that lack CD8 and CD4 alphabeta-T cells as well as B lymphocytes can control a MCMV infection that is lethal in RAG-1(-/-) mice lacking any T- and B-cells. gammadelta T cells, isolated from infected mice can kill MCMV infected target cells in vitro and, importantly, provide long-term protection in infected RAG-1(-/-) mice after adoptive transfer. gammadelta T cells in MCMV infected hosts undergo a prominent and long-lasting phenotypic change most compatible with the view that the majority of the gammadelta T cell population persists in an effector/memory state even after resolution of the acute phase of the infection. A clonotypically focused Vgamma1 and Vgamma2 repertoire was observed at later stages of the infection in the organs where MCMV persists. These findings add gammadelta T cells as yet another protective component to the anti-CMV immune response. Our data provide clear evidence that gammadelta T cells can provide an effective control mechanism of acute CMV infections, particularly when conventional adaptive immune mechanisms are insufficient or absent, like in transplant patient or in the developing immune system in utero. The findings have implications in the stem cell transplant setting, as antigen recognition by gammadelta T cells is not MHC-restricted and dual reactivity against CMV and tumors has been described.
in vivo IL-17A neutralization
Coffelt, S. B., et al. (2015). "IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis" Nature 522(7556): 345-348. PubMed
Metastatic disease remains the primary cause of death for patients with breast cancer. The different steps of the metastatic cascade rely on reciprocal interactions between cancer cells and their microenvironment. Within this local microenvironment and in distant organs, immune cells and their mediators are known to facilitate metastasis formation. However, the precise contribution of tumour-induced systemic inflammation to metastasis and the mechanisms regulating systemic inflammation are poorly understood. Here we show that tumours maximize their chance of metastasizing by evoking a systemic inflammatory cascade in mouse models of spontaneous breast cancer metastasis. We mechanistically demonstrate that interleukin (IL)-1beta elicits IL-17 expression from gamma delta (gammadelta) T cells, resulting in systemic, granulocyte colony-stimulating factor (G-CSF)-dependent expansion and polarization of neutrophils in mice bearing mammary tumours. Tumour-induced neutrophils acquire the ability to suppress cytotoxic T lymphocytes carrying the CD8 antigen, which limit the establishment of metastases. Neutralization of IL-17 or G-CSF and absence of gammadelta T cells prevents neutrophil accumulation and downregulates the T-cell-suppressive phenotype of neutrophils. Moreover, the absence of gammadelta T cells or neutrophils profoundly reduces pulmonary and lymph node metastases without influencing primary tumour progression. Our data indicate that targeting this novel cancer-cell-initiated domino effect within the immune system–the gammadelta T cell/IL-17/neutrophil axis–represents a new strategy to inhibit metastatic disease.
in vivo IL-17A neutralization
Xin, L., et al. (2014). "Commensal microbes drive intestinal inflammation by IL-17-producing CD4+ T cells through ICOSL and OX40L costimulation in the absence of B7-1 and B7-2" Proc Natl Acad Sci U S A 111(29): 10672-10677. PubMed
The costimulatory B7-1 (CD80)/B7-2 (CD86) molecules, along with T-cell receptor stimulation, together facilitate T-cell activation. This explains why in vivo B7 costimulation neutralization efficiently silences a variety of human autoimmune disorders. Paradoxically, however, B7 blockade also potently moderates accumulation of immune-suppressive regulatory T cells (Tregs) essential for protection against multiorgan systemic autoimmunity. Here we show that B7 deprivation in mice overrides the necessity for Tregs in averting systemic autoimmunity and inflammation in extraintestinal tissues, whereas peripherally induced Tregs retained in the absence of B7 selectively mitigate intestinal inflammation caused by Th17 effector CD4(+) T cells. The need for additional immune suppression in the intestine reflects commensal microbe-driven T-cell activation through the accessory costimulation molecules ICOSL and OX40L. Eradication of commensal enteric bacteria mitigates intestinal inflammation and IL-17 production triggered by Treg depletion in B7-deficient mice, whereas re-establishing intestinal colonization with Candida albicans primes expansion of Th17 cells with commensal specificity. Thus, neutralizing B7 costimulation uncovers an essential role for Tregs in selectively averting intestinal inflammation by Th17 CD4(+) T cells with commensal microbe specificity.
in vivo IL-17A neutralization
Kulcsar, K. A., et al. (2014). "Interleukin 10 modulation of pathogenic Th17 cells during fatal alphavirus encephalomyelitis" Proc Natl Acad Sci U S A 111(45): 16053-16058. PubMed
Mosquito-borne alphaviruses are important causes of epidemic encephalomyelitis. Neuronal cell death during fatal alphavirus encephalomyelitis is immune-mediated; however, the types of cells involved and their regulation have not been determined. We show that the virus-induced inflammatory response was accompanied by production of the regulatory cytokine IL-10, and in the absence of IL-10, paralytic disease occurred earlier and mice died faster. To determine the reason for accelerated disease in the absence of IL-10, immune responses in the CNS of IL-10(-/-) and wild-type (WT) mice were compared. There were no differences in the amounts of brain inflammation or peak virus replication; however, IL-10(-/-) animals had accelerated and increased infiltration of CD4(+)IL-17A(+) and CD4(+)IL-17A(+)IFNgamma(+) cells compared with WT animals. Th17 cells infiltrating the brain demonstrated a pathogenic phenotype with the expression of the transcription factor, Tbet, and the production of granzyme B, IL-22, and GM-CSF, with greater production of GM-CSF in IL-10(-/-) mice. Therefore, in fatal alphavirus encephalomyelitis, pathogenic Th17 cells enter the CNS at the onset of neurologic disease and, in the absence of IL-10, appear earlier, develop into Th1/Th17 cells more often, and have greater production of GM-CSF. This study demonstrates a role for pathogenic Th17 cells in fatal viral encephalitis.
in vivo IL-17A neutralization
Khmaladze, I., et al. (2014). "Mannan induces ROS-regulated, IL-17A-dependent psoriasis arthritis-like disease in mice" Proc Natl Acad Sci U S A 111(35): E3669-3678. PubMed
Psoriasis (Ps) and psoriasis arthritis (PsA) are poorly understood common diseases, induced by unknown environmental factors, affecting skin and articular joints. A single i.p. exposure to mannan from Saccharomyces cerevisiae induced an acute inflammation in inbred mouse strains resembling human Ps and PsA-like disease, whereas multiple injections induced a relapsing disease. Exacerbation of disease severity was observed in mice deficient for generation of reactive oxygen species (ROS). Interestingly, restoration of ROS production, specifically in macrophages, ameliorated both skin and joint disease. Neutralization of IL-17A, mainly produced by gammadelta T cells, completely blocked disease symptoms. Furthermore, mice depleted of granulocytes were resistant to disease development. In contrast, certain acute inflammatory mediators (C5, Fcgamma receptor III, mast cells, and histamine) and adaptive immune players (alphabeta T and B cells) were redundant in disease induction. Hence, we propose that mannan-induced activation of macrophages leads to TNF-alpha secretion and stimulation of local gammadelta T cells secreting IL-17A. The combined action of activated macrophages and IL-17A produced in situ drives neutrophil infiltration in the epidermis and dermis of the skin, leading to disease manifestations. Thus, our finding suggests a new mechanism triggered by exposure to exogenous microbial components, such as mannan, that can induce and exacerbate Ps and PsA.
in vivo IL-17A neutralization
Ermann, J., et al. (2014). "Nod/Ripk2 signaling in dendritic cells activates IL-17A-secreting innate lymphoid cells and drives colitis in T-bet-/-.Rag2-/- (TRUC) mice" Proc Natl Acad Sci U S A 111(25): E2559-2566. PubMed
T-bet(-/-).Rag2(-/-) (TRUC) mice spontaneously develop microbiota-driven, TNF-mediated large bowel inflammation that resembles human ulcerative colitis. We show here that IL-23 and IL-1-dependent secretion of IL-17A by innate lymphoid cells (ILCs; defined as CD45(+)lin(-)Thy1(hi)NKp46(-)) is a second critical pathway in this model. Using an in vitro coculture system of bone marrow-derived dendritic cells (DCs) and freshly isolated FACS-purified ILCs, we demonstrate that IL-23 and IL-1 secreted by DCs in response to microbial stimulation work together to induce IL-17A production by ILCs. TNF is not required for IL-17A secretion by ILCs in vitro but synergizes with IL-17A to induce the expression of neutrophil-attracting chemokines. Upstream, activation of the IL-23/IL-17A axis is regulated by nucleotide-binding oligomerization domain containing (Nod)/receptor-interacting serine-threonine kinase 2 (Ripk2) signals in DCs. Genetic ablation of the Nod/Ripk2 signaling pathway protects TRUC mice from developing colitis without affecting the colitogenicity of the intestinal microbiota. Our data provide insight into the complex network of interactions between IL-17A-secreting ILCs and other components of the innate immune system in the development of colitis.
in vivo IL-17A neutralization
Uddin, M. N., et al. (2014). "TNF-alpha-dependent hematopoiesis following Bcl11b deletion in T cells restricts metastatic melanoma" J Immunol 192(4): 1946-1953. PubMed
Using several tumor models, we demonstrate that mice deficient in Bcl11b in T cells, although having reduced numbers of T cells in the peripheral lymphoid organs, developed significantly less tumors compared with wild-type mice. Bcl11b(-/-) CD4(+) T cells, with elevated TNF-alpha levels, but not the Bcl11b(-/-) CD8(+) T cells, were required for the reduced tumor burden, as were NK1.1(+) cells, found in increased numbers in Bcl11b(F/F)/CD4-Cre mice. Among NK1.1(+) cells, the NK cell population was predominant in number and was the only population displaying elevated granzyme B levels and increased degranulation, although not increased proliferation. Although the number of myeloid-derived suppressor cells was increased in the lungs with metastatic tumors of Bcl11b(F/F)/CD4-Cre mice, their arginase-1 levels were severely reduced. The increase in NK cell and myeloid-derived suppressor cell numbers was associated with increased bone marrow and splenic hematopoiesis. Finally, the reduced tumor burden, increased numbers of NK cells in the lung, and increased hematopoiesis in Bcl11b(F/F)/CD4-Cre mice were all dependent on TNF-alpha. Moreover, TNF-alpha treatment of wild-type mice also reduced the tumor burden and increased hematopoiesis and the numbers and activity of NK cells in the lung. In vitro treatment with TNF-alpha of lineage-negative hematopoietic progenitors increased NK and myeloid differentiation, further supporting a role of TNF-alpha in promoting hematopoiesis. These studies reveal a novel role for TNF-alpha in the antitumor immune response, specifically in stimulating hematopoiesis and increasing the numbers and activity of NK cells.
in vivo IL-17A neutralization
Gladiator, A., et al. (2013). "Cutting edge: IL-17-secreting innate lymphoid cells are essential for host defense against fungal infection" J Immunol 190(2): 521-525. PubMed
IL-17-mediated immunity has emerged as a crucial host defense mechanism against fungal infections. Although Th cells are generally thought to act as the major source of IL-17 in response to Candida albicans, we show that fungal control is mediated by IL-17-secreting innate lymphoid cells (ILCs) and not by Th17 cells. By using a mouse model of oropharyngeal candidiasis we found that IL-17A and IL-17F, which are both crucial for pathogen clearance, are produced promptly upon infection in an IL-23-dependent manner, and that ILCs in the oral mucosa are the main source for these cytokines. Ab-mediated depletion of ILCs in RAG1-deficient mice or ILC deficiency in retinoic acid-related orphan receptor c(-/-) mice resulted in a complete failure to control the infection. Taken together, our data uncover the cellular basis for the IL-23/IL-17 axis, which acts right at the onset of infection when it is most needed for fungal control and host protection.
in vivo IL-17A neutralization
Gonzalez-Lombana, C., et al. (2013). "IL-17 mediates immunopathology in the absence of IL-10 following Leishmania major infection" PLoS Pathog 9(3): e1003243. PubMed
Leishmaniasis, resulting from infection with the protozoan parasite Leishmania, consists of a wide spectrum of clinical manifestations, from healing cutaneous lesions to fatal visceral infections. A particularly severe form of cutaneous leishmaniasis, termed mucosal leishmaniasis, exhibits decreased IL-10 levels and an exaggerated inflammatory response that perpetuates the disease. Using a mouse model of leishmaniasis, we investigated what cytokines contribute to increased pathology when IL-10-mediated regulation is absent. Leishmania major infected C57BL/6 mice lacking IL-10 regulation developed larger lesions than controls, but fewer parasites. Both IFN-gamma and IL-17 levels were substantially elevated in mice lacking the capacity to respond to IL-10. IFN-gamma promoted an increased infiltration of monocytes, while IL-17 contributed to an increase in neutrophils. Surprisingly, however, we found that IFN-gamma did not contribute to increased pathology, but instead regulated the IL-17 response. Thus, blocking IFN-gamma led to a significant increase in IL-17, neutrophils and disease. Similarly, the production of IL-17 by cells from leishmaniasis patients was also regulated by IL-10 and IFN-gamma. Additional studies found that the IL-1 receptor was required for both the IL-17 response and increased pathology. Therefore, we propose that regulating IL-17, possibly by downregulating IL-1beta, may be a useful approach for controlling immunopathology in leishmaniasis.
in vivo IL-17A neutralization
Berger, H., et al. (2013). "SOCS3 transactivation by PPARgamma prevents IL-17-driven cancer growth" Cancer Res 73(12): 3578-3590. PubMed
Activation of the transcription factor PPARgamma by the n-3 fatty acid docosahexaenoic acid (DHA) is implicated in controlling proinflammatory cytokine secretion, but the intracellular signaling pathways engaged by PPARgamma are incompletely characterized. Here, we identify the adapter-encoding gene SOCS3 as a critical transcriptional target of PPARgamma. SOCS3 promoter binding and gene transactivation by PPARgamma was associated with a repression in differentiation of proinflammatory T-helper (TH)17 cells. Accordingly, TH17 cells induced in vitro displayed increased SOCS3 expression and diminished capacity to produce interleukin (IL)-17 following activation of PPARgamma by DHA. Furthermore, naive CD4 T cells derived from mice fed a DHA-enriched diet displayed less capability to differentiate into TH17 cells. In two different mouse models of cancer, DHA prevented tumor outgrowth and angiogenesis in an IL-17-dependent manner. Altogether, our results uncover a novel molecular pathway by which PPARgamma-induced SOCS3 expression prevents IL-17-mediated cancer growth.
in vivo IL-17A neutralization
Valdez, P. A., et al. (2012). "Prostaglandin E2 suppresses antifungal immunity by inhibiting interferon regulatory factor 4 function and interleukin-17 expression in T cells" Immunity 36(4): 668-679. PubMed
T helper 17 (Th17) cells play an important role in mucosal host defense through production of the signature cytokines IL-17 and IL-22. Prostaglandin E2 (PGE2) has been shown to enhance IL-17 production by mature Th17 cells. However, when present during Th17 cell differentiation, we found that PGE2 inhibited the transcription factor IRF4 and suppressed production of IL-17 but not IL-22. We show that IRF4 was required for IL-17 expression but inhibited IL-22 expression, highlighting the potential for discordant regulation of these two cytokines in Th17 cells. The pathogenic fungus Cryptococcus neoformans produces PGE2, and we found that it uses PGE2- and IRF4-dependent mechanisms to specifically inhibit induction of IL-17 during Th17 cell differentiation. Blockade of host PGE2 during infection led to increased IL-17 production from CD4(+) T cells and increased survival of mice. These findings suggest that host- or pathogen-derived PGE2 can act directly on Th17 cells during differentiation to inhibit IL-17-dependent antimicrobial responses.
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Neuroscience
MrgprA3 neurons selectively control myeloid-derived cytokines for IL-17 dependent cutaneous immunity.
Preprint on Research Square on 30 November 2023 by Herbert, D., Inclan-Rico, J., et al.
PubMed
Skin employs interdependent cellular networks to facilitate barrier integrity and host immunity through ill-defined mechanisms. This study demonstrates that manipulation of itch-sensing neurons bearing the Mas-related G protein-coupled receptor A3 (MrgprA3) drives IL-17+ γδ T cell expansion, epidermal thickening, and resistance to the human pathogen Schistosoma mansoni through mechanisms that require myeloid antigen presenting cells (APC). Activated MrgprA3 neurons instruct myeloid APCs to downregulate interleukin 33 (IL-33) and up-regulate TNFα partially through the neuropeptide calcitonin gene related peptide (CGRP). Strikingly, cell-intrinsic deletion of IL-33 in myeloid APC basally alters chromatin accessibility at inflammatory cytokine loci and promotes IL-17/23-dependent epidermal thickening, keratinocyte hyperplasia, and resistance to helminth infection. Our findings reveal a previously undescribed mechanism of intercellular cross-talk wherein “itch” neuron activation reshapes myeloid cytokine expression patterns to alter skin composition for cutaneous immunity against invasive pathogens.
- Cancer Research
IL-17A promotes tumorigenesis and upregulates PD-L1 expression in non-small cell lung cancer.
In Journal of Translational Medicine on 17 November 2023 by Liao, H., Chang, X., et al.
PubMed
The tumor microenvironment plays a key role in non-small cell lung cancer (NSCLC) development and also influences the effective response to immunotherapy. The pro-inflammatory factor interleukin-17A mediates important immune responses in the tumor microenvironment. In this study, the potential role and mechanisms of IL-17A in NSCLC were investigated. We detected IL-17A by immunohistochemistry (IHC) in 39 NSCLC patients. Its expression was correlated with the programmed cell death-ligand1 (PD-L1). IL-17A knockdown and overexpression in A549 and SPC-A-1 cell models were constructed. The function of IL-17A was examined in vitro by wound healing, migration, invasion, plate colony formation and T cell killing assay. Western blot analysis, immunofluorescence assay and IHC were performed to investigate the regulation effects of IL-17A on autophagy in A549 and SPC-A-1. The effect of IL-17A on ROS/Nrf2/p62 signaling pathway was detected. Subcutaneous tumor models were established to examine the tumor-promoting effect of IL-17A in vivo and its effect on immunotherapy. We found a prevalent expression of IL-17A in NSCLC tumor tissues and it was positively correlated with PD-L1 expression (r = 0.6121, p < 0.0001). In vitro, IL-17A promotes lung cancer cell migration, invasion and colony formation ability. Moreover, IL-17A upregulated N-cadherin, Twist, and Snail, and downregulated E-cadherin in NSCLC cells. IL-17A enhanced cell survival in the T cell killing assay. Mechanistically, IL-17A induced ROS production and increased Nrf2 and p62 expression, thereby inhibiting autophagy and reducing PD-L1 degradation. In vivo experiments, anti-IL-17A monoclonal antibody alone slowed the growth of subcutaneous tumors in mice. When combined with anti-PD-L1 monoclonal antibody, tumor tissue expression of PD-L1 was reduced and the therapeutic effect was diminished. We found that IL-17A promoted NSCLC progression and inhibited autophagy through the ROS/Nrf2/p62 pathway leading to increased PD-L1 expression in cancer cells. Modulation of IL-17A may affect the therapeutic efficacy of immunotherapy. © 2023. The Author(s).
- Mus musculus (House mouse),
- Genetics,
- Cancer Research
Adenosine A2A receptor is a tumor suppressor of NASH-associated hepatocellular carcinoma.
In Cell Reports Medicine on 19 September 2023 by Allard, B., Jacoberger-Foissac, C., et al.
PubMed
Inhibition of adenosine A2A receptor (A2AR) is a promising approach for cancer immunotherapy currently evaluated in several clinical trials. We here report that anti-obesogenic and anti-inflammatory functions of A2AR, however, significantly restrain hepatocellular carcinoma (HCC) development. Adora2a deletion in mice triggers obesity, non-alcoholic steatohepatitis (NASH), and systemic inflammation, leading to spontaneous HCC and promoting dimethylbenzyl-anthracene (DMBA)- or diethylnitrosamine (DEN)-induced HCC. Conditional Adora2a deletion reveals critical roles of myeloid and hepatocyte-derived A2AR signaling in restraining HCC by limiting hepatic inflammation and steatosis. Remarkably, the impact of A2AR pharmacological blockade on HCC development is dependent on pre-existing NASH. In support of our animal studies, low ADORA2A gene expression in human HCC is associated with cirrhosis, hepatic inflammation, and poor survival. Together, our study uncovers a previously unappreciated tumor-suppressive function for A2AR in the liver and suggests caution in the use of A2AR antagonists in patients with NASH and NASH-associated HCC. Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
- Immunology and Microbiology,
- Mus musculus (House mouse)
Vγ1 and Vγ4 gamma-delta T cells play opposing roles in the immunopathology of traumatic brain injury in males.
In Nature Communications on 18 July 2023 by Abou-El-Hassan, H., Rezende, R. M., et al.
PubMed
Traumatic brain injury (TBI) is a leading cause of morbidity and mortality. The innate and adaptive immune responses play an important role in the pathogenesis of TBI. Gamma-delta (γδ) T cells have been shown to affect brain immunopathology in multiple different conditions, however, their role in acute and chronic TBI is largely unknown. Here, we show that γδ T cells affect the pathophysiology of TBI as early as one day and up to one year following injury in a mouse model. TCRδ-/- mice are characterized by reduced inflammation in acute TBI and improved neurocognitive functions in chronic TBI. We find that the Vγ1 and Vγ4 γδ T cell subsets play opposing roles in TBI. Vγ4 γδ T cells infiltrate the brain and secrete IFN-γ and IL-17 that activate microglia and induce neuroinflammation. Vγ1 γδ T cells, however, secrete TGF-β that maintains microglial homeostasis and dampens TBI upon infiltrating the brain. These findings provide new insights on the role of different γδ T cell subsets after brain injury and lay down the principles for the development of targeted γδ T-cell-based therapy for TBI. © 2023. The Author(s).
- Cell Biology,
- Immunology and Microbiology
Autophagy prevents early proinflammatory responses and neutrophil recruitment during Mycobacterium tuberculosis infection without affecting pathogen burden in macrophages.
In PLoS Biology on 1 June 2023 by Kinsella, R. L., Kimmey, J. M., et al.
PubMed
The immune response to Mycobacterium tuberculosis infection determines tuberculosis disease outcomes, yet we have an incomplete understanding of what immune factors contribute to a protective immune response. Neutrophilic inflammation has been associated with poor disease prognosis in humans and in animal models during M. tuberculosis infection and, therefore, must be tightly regulated. ATG5 is an essential autophagy protein that is required in innate immune cells to control neutrophil-dominated inflammation and promote survival during M. tuberculosis infection; however, the mechanistic basis for how ATG5 regulates neutrophil recruitment is unknown. To interrogate what innate immune cells require ATG5 to control neutrophil recruitment during M. tuberculosis infection, we used different mouse strains that conditionally delete Atg5 in specific cell types. We found that ATG5 is required in CD11c+ cells (lung macrophages and dendritic cells) to control the production of proinflammatory cytokines and chemokines during M. tuberculosis infection, which would otherwise promote neutrophil recruitment. This role for ATG5 is autophagy dependent, but independent of mitophagy, LC3-associated phagocytosis, and inflammasome activation, which are the most well-characterized ways that autophagy proteins regulate inflammation. In addition to the increased proinflammatory cytokine production from macrophages during M. tuberculosis infection, loss of ATG5 in innate immune cells also results in an early induction of TH17 responses. Despite prior published in vitro cell culture experiments supporting a role for autophagy in controlling M. tuberculosis replication in macrophages, the effects of autophagy on inflammatory responses occur without changes in M. tuberculosis burden in macrophages. These findings reveal new roles for autophagy proteins in lung resident macrophages and dendritic cells that are required to suppress inflammatory responses that are associated with poor control of M. tuberculosis infection. Copyright: © 2023 Kinsella et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Targeting lymphoid-derived IL-17 signaling to delay skin aging.
In Nature Aging on 1 June 2023 by Sola-Castrillo, P., Mereu, E., et al.
PubMed
Skin aging is characterized by structural and functional changes that contribute to age-associated frailty. This probably depends on synergy between alterations in the local niche and stem cell-intrinsic changes, underscored by proinflammatory microenvironments that drive pleotropic changes. The nature of these age-associated inflammatory cues, or how they affect tissue aging, is unknown. Based on single-cell RNA sequencing of the dermal compartment of mouse skin, we show a skew towards an IL-17-expressing phenotype of T helper cells, γδ T cells and innate lymphoid cells in aged skin. Importantly, in vivo blockade of IL-17 signaling during aging reduces the proinflammatory state of the skin, delaying the appearance of age-related traits. Mechanistically, aberrant IL-17 signals through NF-κB in epidermal cells to impair homeostatic functions while promoting an inflammatory state. Our results indicate that aged skin shows signs of chronic inflammation and that increased IL-17 signaling could be targeted to prevent age-associated skin ailments. © 2023. The Author(s).
- Mus musculus (House mouse),
- Cardiovascular biology,
- Immunology and Microbiology,
- Neuroscience
Distinct Th17 effector cytokines differentially promote microglial and blood-brain barrier inflammatory responses during post-infectious encephalitis
Preprint on BioRxiv : the Preprint Server for Biology on 12 March 2023 by Wayne, C. R., Bremner, L., et al.
PubMed
SUMMARY Group A Streptococcus (GAS) infections can cause neuropsychiatric sequelae in children due to post-infectious encephalitis. Multiple GAS infections induce migration of Th17 lymphocytes from the nose into the brain, which are critical for microglial activation, blood-brain barrier (BBB) and neural circuit impairment in a mouse disease model. How endothelial cells (ECs) and microglia respond to GAS infections, and which Th17-derived cytokines are essential for these responses are unknown. Using single-cell RNA sequencing and spatial transcriptomics, we found that ECs downregulate BBB genes and microglia upregulate interferon-response, chemokine and antigen-presentation genes after GAS infections. Several microglial-derived chemokines were elevated in patient sera. Administration of a neutralizing antibody against interleukin-17A (IL-17A), but not ablation of granulocyte-macrophage colony-stimulating factor (GM-CSF) in T cells, partially rescued BBB dysfunction and microglial expression of chemokine genes. Thus, IL-17A is critical for neuropsychiatric sequelae of GAS infections and may be targeted to treat these disorders.
- Mus musculus (House mouse)
Candida albicans-specific Th17 cell-mediated response contributes to alcohol-associated liver disease.
In Cell Host & Microbe on 8 March 2023 by Zeng, S., Rosati, E., et al.
PubMed
Alcohol-associated liver disease is accompanied by intestinal mycobiome dysbiosis, yet the impacts on liver disease are unclear. We demonstrate that Candida albicans-specific T helper 17 (Th17) cells are increased in circulation and present in the liver of patients with alcohol-associated liver disease. Chronic ethanol administration in mice causes migration of Candida albicans (C. albicans)-reactive Th17 cells from the intestine to the liver. The antifungal agent nystatin decreased C. albicans-specific Th17 cells in the liver and reduced ethanol-induced liver disease in mice. Transgenic mice expressing T cell receptors (TCRs) reactive to Candida antigens developed more severe ethanol-induced liver disease than transgene-negative littermates. Adoptively transferring Candida-specific TCR transgenic T cells or polyclonal C. albicans-primed T cells exacerbated ethanol-induced liver disease in wild-type mice. Interleukin-17 (IL-17) receptor A signaling in Kupffer cells was required for the effects of polyclonal C. albicans-primed T cells. Our findings indicate that ethanol increases C. albicans-specific Th17 cells, which contribute to alcohol-associated liver disease. Published by Elsevier Inc.
- Immunology and Microbiology
FXYD3 enhances IL-17A signaling to promote psoriasis by competitively binding TRAF3 in keratinocytes.
In Cellular Molecular Immunology on 1 March 2023 by Yang, W., He, R., et al.
PubMed
Psoriasis is a common chronic inflammatory skin disease characterized by inflammatory cell infiltration and epidermal hyperplasia. However, the regulatory complexity of cytokine and cellular networks still needs to be investigated. Here, we show that the expression of FXYD3, a member of the FXYD domain-containing regulators of Na+/K+ ATPases family, is significantly increased in the lesional skin of psoriasis patients and mice with imiquimod (IMQ)-induced psoriasis. IL-17A, a cytokine important for the development of psoriatic lesions, contributes to FXYD3 expression in human primary keratinocytes. FXYD3 deletion in keratinocytes attenuated the psoriasis-like phenotype and inflammation in an IMQ-induced psoriasis model. Importantly, FXYD3 promotes the formation of the IL-17R-ACT1 complex by competing with IL-17R for binding to TRAF3 and then enhances IL-17A signaling in keratinocytes. This promotes the activation of the NF-κB and MAPK signaling pathways and leads to the expression of proinflammatory factors. Our results clarify the mechanism by which FXYD3 serves as a mediator of IL-17A signaling in keratinocytes to form a positive regulatory loop to promote psoriasis exacerbation. Targeting FXYD3 may serve as a potential therapeutic approach in the treatment of psoriasis. © 2023. The Author(s), under exclusive licence to CSI and USTC.
- In Vivo,
- Mus musculus (House mouse)
Nsun2 coupling with RoRγt shapes the fate of Th17 cells and promotes colitis.
In Nature Communications on 16 February 2023 by Yang, W. L., Qiu, W., et al.
PubMed
T helper 17 (Th17) cells are a subset of CD4+ T helper cells involved in the inflammatory response in autoimmunity. Th17 cells secrete Th17 specific cytokines, such as IL-17A and IL17-F, which are governed by the master transcription factor RoRγt. However, the epigenetic mechanism regulating Th17 cell function is still not fully understood. Here, we reveal that deletion of RNA 5-methylcytosine (m5C) methyltransferase Nsun2 in mouse CD4+ T cells specifically inhibits Th17 cell differentiation and alleviates Th17 cell-induced colitis pathogenesis. Mechanistically, RoRγt can recruit Nsun2 to chromatin regions of their targets, including Il17a and Il17f, leading to the transcription-coupled m5C formation and consequently enhanced mRNA stability. Our study demonstrates a m5C mediated cell intrinsic function in Th17 cells and suggests Nsun2 as a potential therapeutic target for autoimmune disease. © 2023. The Author(s).
- Immunology and Microbiology,
- Mus musculus (House mouse)
IL-17 axis is a significant driver of skin inflammation in Card14 mutant pityriasis rubra pilaris model mice
Preprint on Research Square on 2 February 2023 by Yoshikawa, T., Takeichi, T., et al.
PubMed
Pityriasis rubra pilaris (PRP) is a rare inflammatory keratinization disorder with perifollicular erythema, and most autosomal dominant familial cases of atypical juvenile (type V) PRP are caused by gain-of-function mutations in CARD14, which encodes caspase recruitment domain-containing protein 14 (CARD14). We report the first mouse model of PRP to carry a homozygous knock-in mutation, c.380G>C (p.Cys127Ser) corresponding to a PRP-causative human mutation, in CARD14. The Card14C127S/C127S knock-in mice recapitulate key aspects of human PRP, including hair follicle dilatation, follicular plugs, and palmoplantar hyperkeratosis, and show skin barrier dysfunction, the hyperactivation of innate immunity via the IL-36 signaling and inflammasome pathways, and the excessive activation of the IL-17 axis in the outer root sheath and interfollicular epidermis. Administering anti-IL-17A neutralizing antibody significantly attenuates the skin symptoms in mutant mice. Thus, this knock-in mouse is a valid model for further evaluating early events in the PRP pathogenesis and for developing PRP therapies.
- Immunology and Microbiology
GATA4 controls regionalization of tissue immunity and commensal-driven immunopathology.
In Immunity on 10 January 2023 by Earley, Z. M., Lisicka, W., et al.
PubMed
There is growing recognition that regionalization of bacterial colonization and immunity along the intestinal tract has an important role in health and disease. Yet, the mechanisms underlying intestinal regionalization and its dysregulation in disease are not well understood. This study found that regional epithelial expression of the transcription factor GATA4 controls bacterial colonization and inflammatory tissue immunity in the proximal small intestine by regulating retinol metabolism and luminal IgA. Furthermore, in mice without jejunal GATA4 expression, the commensal segmented filamentous bacteria promoted pathogenic inflammatory immune responses that disrupted barrier function and increased mortality upon Citrobacter rodentium infection. In celiac disease patients, low GATA4 expression was associated with metabolic alterations, mucosal Actinobacillus, and increased IL-17 immunity. Taken together, these results reveal broad impacts of GATA4-regulated intestinal regionalization on bacterial colonization and tissue immunity, highlighting an elaborate interdependence of intestinal metabolism, immunity, and microbiota in homeostasis and disease. Copyright © 2022 Elsevier Inc. All rights reserved.
- Immunology and Microbiology,
- Cancer Research
Induction of T-helper-17-cell-mediated anti-tumour immunity by pathogen-mimicking polymer nanoparticles.
In Nature Biomedical Engineering on 1 January 2023 by Son, S., Nam, J., et al.
PubMed
The effectivity of cancer immunotherapies is hindered by immunosuppressive tumour microenvironments that are poorly infiltrated by effector T cells and natural killer cells. In infection and autoimmune disease, the recruitment and activation of effector immune cells is coordinated by pro-inflammatory T helper 17 (TH17) cells. Here we show that pathogen-mimicking hollow nanoparticles displaying mannan (a polysaccharide that activates TH17 cells in microbial cell walls) limit the fraction of regulatory T cells and induce TH17-cell-mediated anti-tumour responses. The nanoparticles activate the pattern-recognition receptor Dectin-2 and Toll-like receptor 4 in dendritic cells, and promote the differentiation of CD4+ T cells into the TH17 phenotype. In mice, intra-tumoural administration of the nanoparticles decreased the fraction of regulatory T cells in the tumour while markedly increasing the fractions of TH17 cells (and the levels of TH17-cell-associated cytokines), CD8+ T cells, natural killer cells and M1-like macrophages. The anti-tumoural activity of the effector cells was amplified by an agonistic antibody against the co-stimulatory receptor OX40 in multiple mouse models. Nanomaterials that induce TH17-cell-mediated immune responses may have therapeutic potential. © 2022. The Author(s), under exclusive licence to Springer Nature Limited.
- Mus musculus (House mouse),
- Cell Biology,
- Immunology and Microbiology
Autophagy is required in macrophages and dendritic cells to prevent early recruitment of neutrophils duringMycobacterium tuberculosisinfection
Preprint on BioRxiv : the Preprint Server for Biology on 4 November 2022 by Kinsella, R. L., Kimmey, J. M., et al.
PubMed
ABSTRACT The immune response to Mycobacterium tuberculosis infection determines tuberculosis disease outcomes, yet we have an incomplete understanding of what immune factors contribute to a protective immune response. Neutrophilic inflammation has been associated with poor disease prognosis in humans and in animal models during M. tuberculosis infection and, therefore, must be tightly regulated. ATG5 is an essential autophagy protein that is required in innate immune cells to control neutrophil-dominated inflammation and promote survival during M. tuberculosis infection, however, the mechanistic basis for how ATG5 regulates neutrophil recruitment is unknown. To interrogate what innate immune cells require ATG5 to control neutrophil recruitment during M. tuberculosis infection, we used different mouse strains that conditionally delete Atg5 in specific cell types. We found that ATG5 is required in CD11c + cells (lung macrophages and dendritic cells) to control the production of proinflammatory cytokines and chemokines during M. tuberculosis infection, which would otherwise promote neutrophil recruitment. This role for ATG5 is autophagy-dependent, but independent of mitophagy, LC3-associated phagocytosis, and inflammasome activation, which are the most well-characterized ways that autophagy proteins regulate inflammation. In addition to the increase in proinflammatory cytokine production during M. tuberculosis infection, loss of ATG5 in innate immune cells also results in an early induction of T H 17 responses. These findings reveal new roles for autophagy proteins in lung resident macrophages and dendritic cells that are required to suppress inflammatory responses that are associated with poor control of M. tuberculosis infection.
- Mus musculus (House mouse),
- Biochemistry and Molecular biology,
- Cell Biology,
- Immunology and Microbiology
Microbiota imbalance induced by dietary sugar disrupts immune-mediated protection from metabolic syndrome.
In Cell on 15 September 2022 by Kawano, Y., Edwards, M., et al.
PubMed
How intestinal microbes regulate metabolic syndrome is incompletely understood. We show that intestinal microbiota protects against development of obesity, metabolic syndrome, and pre-diabetic phenotypes by inducing commensal-specific Th17 cells. High-fat, high-sugar diet promoted metabolic disease by depleting Th17-inducing microbes, and recovery of commensal Th17 cells restored protection. Microbiota-induced Th17 cells afforded protection by regulating lipid absorption across intestinal epithelium in an IL-17-dependent manner. Diet-induced loss of protective Th17 cells was mediated by the presence of sugar. Eliminating sugar from high-fat diets protected mice from obesity and metabolic syndrome in a manner dependent on commensal-specific Th17 cells. Sugar and ILC3 promoted outgrowth of Faecalibaculum rodentium that displaced Th17-inducing microbiota. These results define dietary and microbiota factors posing risk for metabolic syndrome. They also define a microbiota-dependent mechanism for immuno-pathogenicity of dietary sugar and highlight an elaborate interaction between diet, microbiota, and intestinal immunity in regulation of metabolic disorders. Copyright © 2022 Elsevier Inc. All rights reserved.
- Biochemistry and Molecular biology,
- Cancer Research,
- Cell Biology
Targeting Glutamine Metabolism to Enhance Immunoprevention of EGFR-Driven Lung Cancer.
In Advanced Science (Weinheim, Baden-Wurttemberg, Germany) on 1 September 2022 by Huang, M., Xiong, D., et al.
PubMed
Lung cancer is the leading cause of cancer death worldwide. Vaccination against EGFR can be one of the venues to prevent lung cancer. Blocking glutamine metabolism has been shown to improve anticancer immunity. Here, the authors report that JHU083, an orally active glutamine antagonist prodrug designed to be preferentially activated in the tumor microenvironment, has potent anticancer effects on EGFR-driven mouse lung tumorigenesis. Lung tumor development is significantly suppressed when treatment with JHU083 is combined with an EGFR peptide vaccine (EVax) than either single treatment. Flow cytometry and single-cell RNA sequencing of the lung tumors reveal that JHU083 increases CD8+ T cell and CD4+ Th1 cell infiltration, while EVax elicits robust Th1 cell-mediated immune responses and protects mice against EGFRL858R mutation-driven lung tumorigenesis. JHU083 treatment decreases immune suppressive cells, including both monocytic- and granulocytic-myeloid-derived suppressor cells, regulatory T cells, and pro-tumor CD4+ Th17 cells in mouse models. Interestingly, Th1 cells are found to robustly upregulate oxidative metabolism and adopt a highly activated and memory-like phenotype upon glutamine inhibition. These results suggest that JHU083 is highly effective against EGFR-driven lung tumorigenesis and promotes an adaptive T cell-mediated tumor-specific immune response that enhances the efficacy of EVax. © 2022 The Authors. Advanced Science published by Wiley-VCH GmbH.
- Mycoplasmoides pneumoniae (Mycoplasma pneumoniae),
- Immunology and Microbiology
Vaccination with Mycoplasma pneumoniae membrane lipoproteins induces IL-17A driven neutrophilia that mediates Vaccine-Enhanced Disease.
In NPJ Vaccines on 29 July 2022 by Mara, A. B., Gavitt, T. D., et al.
PubMed
Bacterial lipoproteins are an often-underappreciated class of microbe-associated molecular patterns with potent immunomodulatory activity. We previously reported that vaccination of BALB/c mice with Mycoplasma pneumoniae (Mp) lipid-associated membrane proteins (LAMPs) resulted in lipoprotein-dependent vaccine enhanced disease after challenge with virulent Mp, though the immune responses underpinning this phenomenon remain poorly understood. Herein, we report that lipoprotein-induced VED in a mouse model is associated with elevated inflammatory cytokines TNF-α, IL-1β, IL-6, IL-17A, and KC in lung lavage fluid and with suppurative pneumonia marked by exuberant neutrophilia in the pulmonary parenchyma. Whole-lung-digest flow cytometry and RNAScope analysis identified multiple cellular sources for IL-17A, and the numbers of IL-17A producing cells were increased in LAMPs-vaccinated/Mp-challenged animals compared to controls. Specific IL-17A or neutrophil depletion reduced disease severity in our VED model-indicating that Mp lipoproteins induce VED in an IL-17A-dependent manner and through exuberant neutrophil recruitment. IL-17A neutralization reduced levels of TNF-α, IL-1β, IL-6, and KC, indicating that IL-17A preceded other inflammatory cytokines. Surprisingly, we found that IL-17A neutralization impaired bacterial clearance, while neutrophil depletion improved it-indicating that, while IL-17A appears to confer both maladaptive and protective responses, neutrophils play an entirely maladaptive role in VED. Given that lipoproteins are found in virtually all bacteria, the potential for lipoprotein-mediated maladaptive inflammatory responses should be taken into consideration when developing vaccines against bacterial pathogens. © 2022. The Author(s).
- Neutralization,
- Mus musculus (House mouse),
- Immunology and Microbiology
A Murine Point Mutation of Sgpl1 Skin Is Enriched With Vγ6 IL17-Producing Cell and Revealed With Hyperpigmentation After Imiquimod Treatment.
In Frontiers in Immunology on 1 July 2022 by Yang, W., Zhou, B., et al.
PubMed
Sphingosine-1-phosphate lyase is encoded by the Sgpl1 gene, degrades S1P, and is crucial for S1P homeostasis in animal models and humans. S1P lyase deficient patients suffer from adrenal insufficiency, severe lymphopenia, and skin disorders. In this study, we used random mutagenesis screening to identify a mouse line carrying a missense mutation of Sgpl1 (M467K). This mutation caused similar pathologies as Sgpl1 knock-out mice in multiple organs, but greatly preserved its lifespan, which M467K mutation mice look normal under SPF conditions for over 40 weeks, in contrast, the knock-out mice live no more than 6 weeks. When treated with Imiquimod, Sgpl1M467K mice experienced exacerbated skin inflammation, as revealed by aggravated acanthosis and orthokeratotic hyperkeratosis. We also demonstrated that the IL17a producing Vγ6+ cell was enriched in Sgpl1M467K skin and caused severe pathology after imiquimod treatment. Interestingly, hyperchromic plaque occurred in the mutant mice one month after Imiquimod treatment but not in the controls, which resembled the skin disorder found in Sgpl1 deficient patients. Therefore, our results demonstrate that Sgpl1M467K point mutation mice successfully modeled a human disease after being treated with Imiquimod. We also revealed a major subset of γδT cells in the skin, IL17 secreting Vγ6 T cells were augmented by Sgpl1 deficiency and led to skin pathology. Therefore, we have, for the first time, linked the IL17a and γδT cells to SPL insufficiency. Copyright © 2022 Yang, Zhou, Liu, Liu, Wang, Zhang, Lu, Zhang, Zhang, Huang, Zhou, Chao, Gu, Lee, Wang, Liang and He.
- Neutralization,
- Mus musculus (House mouse),
- Immunology and Microbiology
KLF5 protects the intestinal epithelium against Th17 immune response in a murine colitis model.
In JCI Insight on 8 April 2022 by Shieh, J., Chu, T. H., et al.
PubMed
Inflammatory bowel disease (IBD) is a chronic illness characterized by dysregulated immune cascades in the intestines, in which the Th17 immune response plays an important role. We demonstrated that mice with intestinal epithelium-specific deletion of Krüppel-like factor 5 (Klf5) developed Th17-dependent colonic inflammation. In the absence of KLF5, there was aberrant cellular localization of phosphorylated STAT3, an essential mediator of the Th17-associated cytokine, IL-22, which is required for epithelial tissue regeneration. In contrast, mitigation of IL-17A with anti-IL-17A neutralizing antibody attenuated colitis in Klf5-deficient mice. There was also a considerable shift in the colonic microbiota of Klf5-deficient mice that phenocopied human IBD. Notably, the inflammatory response due to Klf5 deletion was alleviated by antibiotic treatment, implicating the role of microbiota in pathogenesis. Finally, human colitic tissues had reduced KLF5 levels when compared with healthy tissues. Together, these findings demonstrated the importance of KLF5 in protecting the intestinal epithelium against Th17-mediated immune and inflammatory responses. The mice described herein may serve as a potential model for human IBD.
- Immunology and Microbiology
Early IL-17A production helps establish Mycobacterium intracellulare infection in mice.
In PLoS Pathogens on 1 April 2022 by Jung, B. G., Samten, B., et al.
PubMed
Nontuberculous mycobacteria (NTM) infection is common in patients with structural lung damage. To address how NTM infection is established and causes lung damage, we established an NTM mouse model by intranasal inoculation of clinical isolates of M. intracellulare. During the 39-week course of infection, the bacteria persistently grew in the lung and caused progressive granulomatous and fibrotic lung damage with mortality exceeding 50%. Lung neutrophils were significantly increased at 1 week postinfection, reduced at 2 weeks postinfection and increased again at 39 weeks postinfection. IL-17A was increased in the lungs at 1-2 weeks of infection and reduced at 3 weeks postinfection. Depletion of neutrophils during early (0-2 weeks) and late (32-34 weeks) infection had no effect on mortality or lung damage in chronically infected mice. However, neutralization of IL-17A during early infection significantly reduced bacterial burden, fibrotic lung damage, and mortality in chronically infected mice. Since it is known that IL-17A regulates matrix metalloproteinases (MMPs) and that MMPs contribute to the pathogenesis of pulmonary fibrosis, we determined the levels of MMPs in the lungs of M. intracellulare-infected mice. Interestingly, MMP-3 was significantly reduced by anti-IL-17A neutralizing antibody. Moreover, in vitro data showed that exogenous IL-17A exaggerated the production of MMP-3 by lung epithelial cells upon M. intracellulare infection. Collectively, our findings suggest that early IL-17A production precedes and promotes organized pulmonary M. intracellulare infection in mice, at least in part through MMP-3 production.