InVivoMAb anti-mouse IL-1 R (CD121a)
Product Description
Specifications
| Isotype | Armenian Hamster IgG, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure pH 6.0T Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Extracellular domain of mouse IL-1 R type 1 |
| Reported Applications |
in vivo IL-1 R blockade in vitro IL-1 R blockade |
| Formulation |
PBS, pH 6.0 0.01% Tween Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2661843 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo IL-1 R blockade
Singh, S., et al (2021). "IL-1alpha Mediates Innate and Acquired Resistance to Immunotherapy in Melanoma" J Immunol 206(8): 1966-1975.
PubMed
Inflammation has long been associated with cancer initiation and progression; however, how inflammation causes immune suppression in the tumor microenvironment and resistance to immunotherapy is not well understood. In this study, we show that both innate proinflammatory cytokine IL-1alpha and immunotherapy-induced IL-1alpha make melanoma resistant to immunotherapy. In a mouse melanoma model, we found that tumor size was inversely correlated with response to immunotherapy. Large tumors had higher levels of IL-1alpha, Th2 cytokines, polymorphonuclear myeloid-derived suppressor cells (PMN-MDSCs), and regulatory T cells but lower levels of IL-12, Th1 cytokines, and activated T cells. We found that therapy with adenovirus-encoded CD40L (rAd.CD40L) increased tumor levels of IL-1alpha and PMN-MDSCs. Blocking the IL-1 signaling pathway significantly decreased rAd.CD40L-induced PMN-MDSCs and their associated PD-L1 expression in the tumor microenvironment and enhanced tumor-specific immunity. Similarly, blocking the IL-1 signaling pathway improved the antimelanoma activity of anti-PD-L1 Ab therapy. Our study suggests that blocking the IL-1alpha signaling pathway may increase the efficacy of immunotherapies against melanoma.
in vivo IL-1 R blockade
Kongsomboonvech, A. K., et al (2020). "Naïve CD8 T cell IFNγ responses to a vacuolar antigen are regulated by an inflammasome-independent NLRP3 pathway and Toxoplasma gondii ROP5" PLoS Pathog 16(8): e1008327.
PubMed
Host resistance to Toxoplasma gondii relies on CD8 T cell IFNγ responses, which if modulated by the host or parasite could influence chronic infection and parasite transmission between hosts. Since host-parasite interactions that govern this response are not fully elucidated, we investigated requirements for eliciting naïve CD8 T cell IFNγ responses to a vacuolar resident antigen of T. gondii, TGD057. Naïve TGD057 antigen-specific CD8 T cells (T57) were isolated from transnuclear mice and responded to parasite-infected bone marrow-derived macrophages (BMDMs) in an antigen-dependent manner, first by producing IL-2 and then IFNγ. T57 IFNγ responses to TGD057 were independent of the parasite’s protein export machinery ASP5 and MYR1. Instead, host immunity pathways downstream of the regulatory Immunity-Related GTPases (IRG), including partial dependence on Guanylate-Binding Proteins, are required. Multiple T. gondii ROP5 isoforms and allele types, including ‘avirulent’ ROP5A from clade A and D parasite strains, were able to suppress CD8 T cell IFNγ responses to parasite-infected BMDMs. Phenotypic variance between clades B, C, D, F, and A strains suggest T57 IFNγ differentiation occurs independently of parasite virulence or any known IRG-ROP5 interaction. Consistent with this, removal of ROP5 is not enough to elicit maximal CD8 T cell IFNγ production to parasite-infected cells. Instead, macrophage expression of the pathogen sensors, NLRP3 and to a large extent NLRP1, were absolute requirements. Other members of the conventional inflammasome cascade are only partially required, as revealed by decreased but not abrogated T57 IFNγ responses to parasite-infected ASC, caspase-1/11, and gasdermin D deficient cells. Moreover, IFNγ production was only partially reduced in the absence of IL-12, IL-18 or IL-1R signaling. In summary, T. gondii effectors and host machinery that modulate parasitophorous vacuolar membranes, as well as NLR-dependent but inflammasome-independent pathways, determine the full commitment of CD8 T cells IFNγ responses to a vacuolar antigen.
in vivo IL-1 R blockade
Allen, B. M., et al (2020). "Systemic dysfunction and plasticity of the immune macroenvironment in cancer models" Nat Med 26(7): 1125-1134.
PubMed
Understanding of the factors governing immune responses in cancer remains incomplete, limiting patient benefit. In this study, we used mass cytometry to define the systemic immune landscape in response to tumor development across five tissues in eight mouse tumor models. Systemic immunity was dramatically altered across models and time, with consistent findings in the peripheral blood of patients with breast cancer. Changes in peripheral tissues differed from those in the tumor microenvironment. Mice with tumor-experienced immune systems mounted dampened responses to orthogonal challenges, including reduced T cell activation during viral or bacterial infection. Antigen-presenting cells (APCs) mounted weaker responses in this context, whereas promoting APC activation rescued T cell activity. Systemic immune changes were reversed with surgical tumor resection, and many were prevented by interleukin-1 or granulocyte colony-stimulating factor blockade, revealing remarkable plasticity in the systemic immune state. These results demonstrate that tumor development dynamically reshapes the composition and function of the immune macroenvironment.
in vivo IL-1 R blockade
Choi, G. E., et al (2018). "Autophagy deficiency in myeloid cells exacerbates eosinophilic inflammation in chronic rhinosinusitis" J Allergy Clin Immunol 141(3): 938-950 e912.
PubMed
BACKGROUND: Eosinophilic inflammation is a major pathologic feature of chronic rhinosinusitis (CRS) and is frequently associated with severe refractory disease. Prostaglandin (PG) D2 levels are increased in patients with CRS, and PGD2 is an important contributing factor to eosinophilic inflammation. Autophagy has a pleiotropic effect on immune responses and disease pathogenesis. Recent studies suggest the potential involvement of autophagy in patients with CRS and the PG pathway. OBJECTIVE: We sought to investigate whether altered function of autophagy is associated with eosinophilic inflammation and dysregulated production of PGD2 in patients with CRS. METHODS: We used myeloid cell-specific deletion of autophagy-related gene 7 (Atg7), which is vital for autophagy, and investigated the effects of impaired autophagy on eosinophilic inflammation in a murine model of eosinophilic chronic rhinosinusitis (ECRS). The effect of autophagy on PGD2 production and gene expression profiles associated with allergy and the PG pathway were assessed. RESULTS: We found that impaired autophagy in myeloid cells aggravated eosinophilia, epithelial hyperplasia, and mucosal thickening in mice with ECRS. This aggravation was associated with gene expression profiles that favor eosinophilic inflammation, TH2 response, mast cell infiltration, and PGD2 dysregulation. Supporting this, PGD2 production was also increased significantly by impaired autophagy. Among other myeloid cells, macrophages were associated with autophagy deficiency, leading to increased IL-1beta levels. Macrophage depletion or blockade of IL-1 receptor led to alleviation of eosinophilic inflammation and sinonasal anatomic abnormalities associated with autophagy deficiency. CONCLUSION: Our results suggest that impaired autophagy in myeloid cells, particularly macrophages, has a causal role in eosinophilic inflammation and ECRS pathogenesis.
Gimblet, C., et al (2017). "Cutaneous Leishmaniasis Induces a Transmissible Dysbiotic Skin Microbiota that Promotes Skin Inflammation" Cell Host Microbe 22(1): 13-24.e14.
PubMed
Skin microbiota can impact allergic and autoimmune responses, wound healing, and anti-microbial defense. We investigated the role of skin microbiota in cutaneous leishmaniasis and found that human patients infected with Leishmania braziliensis develop dysbiotic skin microbiota, characterized by increases in the abundance of Staphylococcus and/or Streptococcus. Mice infected with L. major exhibit similar changes depending upon disease severity. Importantly, this dysbiosis is not limited to the lesion site, but is transmissible to normal skin distant from the infection site and to skin from co-housed naive mice. This observation allowed us to test whether a pre-existing dysbiotic skin microbiota influences disease, and we found that challenging dysbiotic naive mice with L. major or testing for contact hypersensitivity results in exacerbated skin inflammatory responses. These findings demonstrate that a dysbiotic skin microbiota is not only a consequence of tissue stress, but also enhances inflammation, which has implications for many inflammatory cutaneous diseases.
in vivo IL-1 R blockade
Naik, S., et al (2017). "Inflammatory memory sensitizes skin epithelial stem cells to tissue damage" Nature 550(7677): 475-480.
PubMed
The skin barrier is the body’s first line of defence against environmental assaults, and is maintained by epithelial stem cells (EpSCs). Despite the vulnerability of EpSCs to inflammatory pressures, neither the primary response to inflammation nor its enduring consequences are well understood. Here we report a prolonged memory to acute inflammation that enables mouse EpSCs to hasten barrier restoration after subsequent tissue damage. This functional adaptation does not require skin-resident macrophages or T cells. Instead, EpSCs maintain chromosomal accessibility at key stress response genes that are activated by the primary stimulus. Upon a secondary challenge, genes governed by these domains are transcribed rapidly. Fuelling this memory is Aim2, which encodes an activator of the inflammasome. The absence of AIM2 or its downstream effectors, caspase-1 and interleukin-1beta, erases the ability of EpSCs to recollect inflammation. Although EpSCs benefit from inflammatory tuning by heightening their responsiveness to subsequent stressors, this enhanced sensitivity probably increases their susceptibility to autoimmune and hyperproliferative disorders, including cancer.
in vivo IL-1 R blockade
Lin, C. C., et al (2016). "IL-1-induced Bhlhe40 identifies pathogenic T helper cells in a model of autoimmune neuroinflammation" J Exp Med 213(2): 251-271.
PubMed
The features that define autoreactive T helper (Th) cell pathogenicity remain obscure. We have previously shown that Th cells require the transcription factor Bhlhe40 to mediate experimental autoimmune encephalomyelitis (EAE), a mouse model of multiple sclerosis. Here, using Bhlhe40 reporter mice and analyzing both polyclonal and TCR transgenic Th cells, we found that Bhlhe40 expression was heterogeneous after EAE induction, with Bhlhe40-expressing cells displaying marked production of IFN-γ, IL-17A, and granulocyte-macrophage colony-stimulating factor. In adoptive transfer EAE models, Bhlhe40-deficient Th1 and Th17 cells were both nonencephalitogenic. Pertussis toxin (PTX), a classical co-adjuvant for actively induced EAE, promoted IL-1β production by myeloid cells in the draining lymph node and served as a strong stimulus for Bhlhe40 expression in Th cells. Furthermore, PTX co-adjuvanticity was Bhlhe40 dependent. IL-1β induced Bhlhe40 expression in polarized Th17 cells, and Bhlhe40-expressing cells exhibited an encephalitogenic transcriptional signature. In vivo, IL-1R signaling was required for full Bhlhe40 expression by Th cells after immunization. Overall, we demonstrate that Bhlhe40 expression identifies encephalitogenic Th cells and defines a PTX-IL-1-Bhlhe40 pathway active in EAE.
in vitro IL-1 R blockade
Ha, H. L., et al (2014). "IL-17 drives psoriatic inflammation via distinct, target cell-specific mechanisms" Proc Natl Acad Sci U S A 111(33): E3422-3431.
PubMed
Psoriasis is a chronic inflammatory skin disease characterized by abnormal keratinocyte proliferation and differentiation and by an influx of inflammatory cells. The mechanisms underlying psoriasis in humans and in mouse models are poorly understood, although evidence strongly points to crucial contributions of IL-17 cytokines, which signal via the obligatory adaptor CIKS/Act1. Here we identify critical roles of CIKS/Act1-mediated signaling in imiquimod-induced psoriatic inflammation, a mouse model that shares features with the human disease. We found that IL-17 cytokines/CIKS-mediated signaling into keratinocytes is essential for neutrophilic microabscess formation and contributes to hyperproliferation and markedly attenuated differentiation of keratinocytes, at least in part via direct effects. In contrast, IL-17 cytokines/CIKS-mediated signaling into nonkeratinocytes, particularly into dermal fibroblasts, promotes cellular infiltration and, importantly, leads to enhanced the accumulation of IL-17-producing gammadeltaT cells in skin, comprising a positive feed-forward mechanism. Thus, CIKS-mediated signaling is central in the development of both dermal and epidermal hallmarks of psoriasis, inducing distinct pathologies via target cell-specific effects. CIKS-mediated signaling represents a potential therapeutic target in psoriasis.
Product Citations
-
-
Immunology and Microbiology
-
Genetics
-
COVID-19
-
Cancer Research
SARS-CoV-2 mRNA vaccines sensitize tumours to immune checkpoint blockade.
In Nature on 1 November 2025 by Grippin, A., Marconi, C., et al.
PubMed
Immune checkpoint inhibitors (ICIs) extend survival in many patients with cancer but are ineffective in patients without pre-existing immunity1-9. Although personalized mRNA cancer vaccines sensitize tumours to ICIs by directing immune attacks against preselected antigens, personalized vaccines are limited by complex and time-intensive manufacturing processes10-14. Here we show that mRNA vaccines targeting SARS-CoV-2 also sensitize tumours to ICIs. In preclinical models, SARS-CoV-2 mRNA vaccines led to a substantial increase in type I interferon, enabling innate immune cells to prime CD8+ T cells that target tumour-associated antigens. Concomitant ICI treatment is required for maximal efficacy in immunologically cold tumours, which respond by increasing PD-L1 expression. Similar correlates of vaccination response are found in humans, including increases in type I interferon, myeloid-lymphoid activation in healthy volunteers and PD-L1 expression on tumours. Moreover, receipt of SARS-CoV-2 mRNA vaccines within 100 days of initiating ICI is associated with significantly improved median and three-year overall survival in multiple large retrospective cohorts. This benefit is similar among patients with immunologically cold tumours. Together, these results demonstrate that clinically available mRNA vaccines targeting non-tumour-related antigens are potent immune modulators capable of sensitizing tumours to ICIs.
-
-
-
Immunology and Microbiology
Engineered bacteria launch and control an oncolytic virus.
In Nat Biomed Eng on 15 August 2025 by Singer, Z. S., Pabon, J., et al.
PubMed
The ability of bacteria and viruses to selectively replicate in tumours has led to synthetic engineering of new microbial therapies. Here we design a cooperative strategy whereby Salmonella typhimurium bacteria transcribe and deliver the Senecavirus A RNA genome inside host cells, launching a potent oncolytic viral infection. 'Encapsidated' by bacteria, the viral genome can further bypass circulating antiviral antibodies to reach the tumour and initiate replication and spread within immune mice. Finally, we engineer the virus to require a bacterially delivered protease to achieve virion maturation, demonstrating bacterial control over the virus. Together, we refer to this platform as 'CAPPSID' for Coordinated Activity of Prokaryote and Picornavirus for Safe Intracellular Delivery. This work extends bacterially delivered therapeutics to viral genomes, and shows how a consortium of microbes can achieve a cooperative aim.
-
-
Mycobacterium bovis frd operon phase variation hijacks succinate signaling to drive immunometabolic rewiring and pathogenicity.
In Nat Commun on 16 July 2025 by Dong, Y., Ge, X., et al.
PubMed
Tuberculosis (TB), caused by Mycobacterium tuberculosis complex (MTBC) pathogens, remains a global health threat. While bacterial genetic adaptations during host infection are poorly understood, phase variation in genomic homopolymeric tracts (HT) may drive pathogenicity evolution. Here, we demonstrate that M. bovis exploits HT insertion mutations in the fumarate reductase-encoding frd operon to subvert host immunometabolism. In macrophages, wild-type M. bovis secretes FRD-catalyzed succinate, stabilizing hypoxia-inducible factor-1α (HIF-1α) to drive glycolytic reprogramming and IL-1β production. This activates IL-1R-dependent Th1 immunity, restraining bacterial replication. Conversely, M. bovis frd HT insertion mutants impair succinate secretion, suppressing HIF-1α/IL-1β signaling and redirecting immunity toward pathogenic Th17 responses that promote neutrophil infiltration and tissue necrosis. Mice infection models reveal that M. bovis frd mutants exhibit enhanced pathogenicity, with higher pulmonary bacterial burdens. IL-1R blockade phenocopies frd HT insertion mutation effects, exacerbating lung pathology. Crucially, conserved frd HT polymorphisms in clinical M. tb isolates suggest shared immune evasion strategies across MTBC pathogens. Our work uncovers the bacterial gene phase variation mechanism of hijacking the succinate/HIF-1α/IL-1β axis to operate host immunity, providing a framework for targeting host metabolic checkpoints in TB therapy.
-
-
Cell Biology
-
Immunology and Microbiology
Caspase-11 drives macrophage hyperinflammation in models of Polg-related mitochondrial disease.
In Nat Commun on 20 May 2025 by VanPortfliet, J. J., Lei, Y., et al.
PubMed
Mitochondrial diseases (MtD) represent a significant public health challenge due to their heterogenous clinical presentation, often severe and progressive symptoms, and lack of effective therapies. Environmental exposures, such bacterial and viral infection, can further compromise mitochondrial function and exacerbate the progression of MtD. However, the underlying immune alterations that enhance immunopathology in MtD remain unclear. Here we employ in vitro and in vivo approaches to clarify the molecular and cellular basis for innate immune hyperactivity in models of polymerase gamma (Polg)-related MtD. We reveal that type I interferon (IFN-I)-mediated upregulation of caspase-11 and guanylate-binding proteins (GBP) increase macrophage sensing of the opportunistic microbe Pseudomonas aeruginosa (PA) in Polg mutant mice. Furthermore, we show that excessive cytokine secretion and activation of pyroptotic cell death pathways contribute to lung inflammation and morbidity after infection with PA. Our work provides a mechanistic framework for understanding innate immune dysregulation in MtD and reveals potential targets for limiting infection- and inflammation-related complications in Polg-related MtD.
-
-
Earlier onset of chemotherapy-induced neuropathic pain in females by ICAM-1-mediated accumulation of perivascular macrophages.
In Sci Adv on 18 April 2025 by Chen, L., Zou, X., et al.
PubMed
Sex differences in the pathogenesis of a variety of diseases have drawn increasing attention. However, it remains unclear whether such differences exist in chemotherapy-induced neuropathic pain. Here, we conducted a retrospective analysis of clinical case data and found that peripheral sensory disorders occurred earlier in females than in males following bortezomib (BTZ) treatment in patients with multiple myeloma. BTZ treatment led to an early elevation of intercellular adhesion molecule-1, which triggered the infiltration of peripheral monocytes into the perivascular region of the spinal cord in female mice. The CC-chemokine ligand 1 released by infiltrating macrophages directly activated neurons or indirectly activated neurons by enhancing the astrocyte activity, ultimately leading to the earlier onset of BTZ-induced neuropathic pain in females. Together, clarifying the mechanism underlying the earlier onset of BTZ-induced neuropathic pain will contribute to the precise treatment of multiple myeloma in females.
-
-
Immunology and Microbiology
The AhR-Ovol1-Id1 regulatory axis in keratinocytes promotes epidermal and immune homeostasis in atopic dermatitis-like skin inflammation.
In Cell Mol Immunol on 1 March 2025 by Chen, Z., Dragan, M., et al.
PubMed
The skin is our outer permeability and immune defense barrier against myriad external assaults. Aryl hydrocarbon receptor (AhR) senses environmental factors and regulates barrier robustness and immune homeostasis. AhR agonists have been approved by the FDA for psoriasis treatment and are in clinical trials for the treatment of atopic dermatitis (AD), but the underlying mechanism of action remains poorly defined. Here, we report that OVOL1/Ovol1 is a conserved and direct transcriptional target of AhR in epidermal keratinocytes. We show that OVOL1/Ovol1 influences AhR-mediated regulation of keratinocyte gene expression and that OVOL1/Ovol1 ablation in keratinocytes impairs the barrier-promoting function of AhR, exacerbating AD-like inflammation. Mechanistically, we have identified Ovol1's direct downstream targets genome-wide and provided in vivo evidence supporting the role of Id1 as a functional target in barrier maintenance, disease suppression, and neutrophil accumulation. Furthermore, our findings reveal that an IL-1/dermal γδT cell axis exacerbates type 2 and 3 immune responses downstream of barrier perturbation in Ovol1-deficient AD skin. Finally, we present data suggesting the clinical relevance of OVOL1 and ID1 functions in human AD skin. Our study highlights a keratinocyte-intrinsic AhR-Ovol1-Id1 regulatory axis that promotes both epidermal and immune homeostasis in the context of skin inflammation, identifying new therapeutic targets.
-
-
-
Immunology and Microbiology
-
Cancer Research
T Cells Instruct Immune Checkpoint Inhibitor Therapy Resistance in Tumors Responsive to IL1 and TNFα Inflammation.
In Cancer Immunol Res on 3 February 2025 by Cho, N. W., Guldberg, S. M., et al.
PubMed
Resistance to immune checkpoint inhibitors (ICI) is common, even in tumors with T-cell infiltration. We thus investigated consequences of ICI-induced T-cell infiltration in the microenvironment of resistant tumors. T cells and neutrophil numbers increased in ICI-resistant tumors following treatment, in contrast to ICI-responsive tumors. Resistant tumors were distinguished by high expression of IL1 receptor 1, enabling a synergistic response to IL1 and TNFα to induce G-CSF, CXCL1, and CXCL2 via NF-κB signaling, supporting immunosuppressive neutrophil accumulation in tumor. Perturbation of this inflammatory resistance circuit sensitized tumors to ICIs. Paradoxically, T cells drove this resistance circuit via TNFα both in vitro and in vivo. Evidence of this inflammatory resistance circuit and its impact also translated to human cancers. These data support a mechanism of ICI resistance, wherein treatment-induced T-cell activity can drive resistance in tumors responsive to IL1 and TNFα, with important therapeutic implications.
-
-
-
Immunology and Microbiology
-
Neuroscience
MrgprA3 neurons drive cutaneous immunity against helminths through selective control of myeloid-derived IL-33.
In Nat Immunol on 1 November 2024 by Inclan-Rico, J. M., Napuri, C. M., et al.
PubMed
Skin uses interdependent cellular networks for barrier integrity and host immunity, but most underlying mechanisms remain obscure. Herein, we demonstrate that the human parasitic helminth Schistosoma mansoni inhibited pruritus evoked by itch-sensing afferents bearing the Mas-related G-protein-coupled receptor A3 (MrgprA3) in mice. MrgprA3 neurons controlled interleukin (IL)-17+ γδ T cell expansion, epidermal hyperplasia and host resistance against S. mansoni through shaping cytokine expression in cutaneous antigen-presenting cells. MrgprA3 neuron activation downregulated IL-33 but induced IL-1β and tumor necrosis factor in macrophages and type 2 conventional dendritic cells partially through the neuropeptide calcitonin gene-related peptide. Macrophages exposed to MrgprA3-derived secretions or bearing cell-intrinsic IL-33 deletion showed increased chromatin accessibility at multiple inflammatory cytokine loci, promoting IL-17/IL-23-dependent changes to the epidermis and anti-helminth resistance. This study reveals a previously unrecognized intercellular communication mechanism wherein itch-inducing MrgprA3 neurons initiate host immunity against skin-invasive parasites by directing cytokine expression patterns in myeloid antigen-presenting cell subsets.
-
-
-
Immunology and Microbiology
NLRP3-mediated IL-1β in regulating the imbalance between Th17 and Treg in experimental autoimmune prostatitis.
In Sci Rep on 13 August 2024 by Liu, X., Chen, J., et al.
PubMed
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a urinary disorder that affects youthful to middle-aged men most frequently. It has been revealed that Th17/Treg imbalance is a crucial factor in the pathophysiological mechanisms behind this disease. However, this imbalance's mechanisms are unknown. In the experimental autoimmune prostatitis (EAP) mouse model, the NLRP3 inflammasome was turned on, IL-1β levels went up. Moreover, there exists a discernible positive association between the upsurge in IL-1β and the perturbation of Th17/Treg equilibrium. Additionally, we have revealed that IL-1β plays a vital role in promoting the differentiation of Naïve CD4+ T cells into the Th17 cells and enhances the conversion of Treg cells into Th17 cells. Further studies revealed that IL-1β promotes STAT3 phosphorylation, which is what causes Treg cells to become Th17 cells. All data strongly suggest that the NLRP3 inflammatory influence Th17 cell development and the conversion of Treg cells into Th17 cells through IL-1β, disrupting the Th17/Treg balance and exacerbating EAP inflammation. In this article, we provide new theories for the pathogenesis of CP/CPPS and propose new prevention and therapy methods.
-
-
An AhR-Ovol1-Id1 regulatory axis in keratinocytes promotes skin homeostasis against atopic dermatitis
In bioRxiv on 31 January 2024 by Chen, Z., Dragan, M., et al.
-
Multiomic profiling of cutaneous leishmaniasis infections reveals microbiota-driven mechanisms underlying disease severity.
In Sci Transl Med on 18 October 2023 by Amorim, C. F., Lovins, V. M., et al.
PubMed
Leishmania braziliensis is a parasitic infection that can result in inflammation and skin injury with highly variable and unpredictable clinical outcomes. Here, we investigated the potential impact of microbiota on infection-induced inflammatory responses and disease resolution by conducting an integrated analysis of the skin microbiome and host transcriptome on a cohort of 62 patients infected with L. braziliensis. We found that overall bacterial burden and microbiome configurations dominated with Staphylococcus spp. were associated with delayed healing and enhanced inflammatory responses, especially by IL-1 family members. Quantification of host and bacterial transcripts on human lesions revealed that high lesional S. aureus transcript abundance was associated with delayed healing and increased expression of IL-1β. This cytokine was critical for modulating disease outcomes in L. braziliensis-infected mice colonized with S. aureus, given that its neutralization reduced pathology and inflammation. These results highlight how the human microbiome can shape disease outcomes in cutaneous leishmaniasis and suggest pathways toward host-directed therapies to mitigate the inflammatory consequences.
-
-
Cancer Research
-
Immunology and Microbiology
Context-dependent activation of STING-interferon signaling by CD11b agonists enhances anti-tumor immunity.
In Cancer Cell on 12 June 2023 by Liu, X., Hogg, G. D., et al.
PubMed
Chronic activation of inflammatory pathways and suppressed interferon are hallmarks of immunosuppressive tumors. Previous studies have shown that CD11b integrin agonists could enhance anti-tumor immunity through myeloid reprograming, but the underlying mechanisms remain unclear. Herein we find that CD11b agonists alter tumor-associated macrophage (TAM) phenotypes by repressing NF-κB signaling and activating interferon gene expression simultaneously. Repression of NF-κB signaling involves degradation of p65 protein and is context independent. In contrast, CD11b agonism induces STING/STAT1 pathway-mediated interferon gene expression through FAK-mediated mitochondrial dysfunction, with the magnitude of induction dependent on the tumor microenvironment and amplified by cytotoxic therapies. Using tissues from phase I clinical studies, we demonstrate that GB1275 treatment activates STING and STAT1 signaling in TAMs in human tumors. These findings suggest potential mechanism-based therapeutic strategies for CD11b agonists and identify patient populations more likely to benefit.
-
-
-
In vivo experiments
-
Immunology and Microbiology
Early alveolar macrophage response and IL-1R-dependent T cell priming determine transmissibility of Mycobacterium tuberculosis strains.
In Nat Commun on 16 February 2022 by Lovey, A., Verma, S., et al.
PubMed
Mechanisms underlying variability in transmission of Mycobacterium tuberculosis strains remain undefined. By characterizing high and low transmission strains of M.tuberculosis in mice, we show here that high transmission M.tuberculosis strain induce rapid IL-1R-dependent alveolar macrophage migration from the alveolar space into the interstitium and that this action is key to subsequent temporal events of early dissemination of bacteria to the lymph nodes, Th1 priming, granulomatous response and bacterial control. In contrast, IL-1R-dependent alveolar macrophage migration and early dissemination of bacteria to lymph nodes is significantly impeded in infection with low transmission M.tuberculosis strain; these events promote the development of Th17 immunity, fostering neutrophilic inflammation and increased bacterial replication. Our results suggest that by inducing granulomas with the potential to develop into cavitary lesions that aids bacterial escape into the airways, high transmission M.tuberculosis strain is poised for greater transmissibility. These findings implicate bacterial heterogeneity as an important modifier of TB disease manifestations and transmission.
-
-
-
Cardiovascular biology
-
Immunology and Microbiology
Viral coinfection promotes tuberculosis immunopathogenesis by type I IFN signaling-dependent impediment of Th1 pulmonary influx
In Research Square on 23 June 2021 by Shin, S. J., Kang, T. G., et al.
-
-
-
In vitro experiments
-
In vitro experiments
-
Immunology and Microbiology
Naïve CD8 T cell IFNγ responses to a vacuolar antigen are regulated by an inflammasome-independent NLRP3 pathway and Toxoplasma gondii ROP5.
In PLoS Pathog on 1 August 2020 by Kongsomboonvech, A. K., Rodríguez, F., et al.
PubMed
Host resistance to Toxoplasma gondii relies on CD8 T cell IFNγ responses, which if modulated by the host or parasite could influence chronic infection and parasite transmission between hosts. Since host-parasite interactions that govern this response are not fully elucidated, we investigated requirements for eliciting naïve CD8 T cell IFNγ responses to a vacuolar resident antigen of T. gondii, TGD057. Naïve TGD057 antigen-specific CD8 T cells (T57) were isolated from transnuclear mice and responded to parasite-infected bone marrow-derived macrophages (BMDMs) in an antigen-dependent manner, first by producing IL-2 and then IFNγ. T57 IFNγ responses to TGD057 were independent of the parasite's protein export machinery ASP5 and MYR1. Instead, host immunity pathways downstream of the regulatory Immunity-Related GTPases (IRG), including partial dependence on Guanylate-Binding Proteins, are required. Multiple T. gondii ROP5 isoforms and allele types, including 'avirulent' ROP5A from clade A and D parasite strains, were able to suppress CD8 T cell IFNγ responses to parasite-infected BMDMs. Phenotypic variance between clades B, C, D, F, and A strains suggest T57 IFNγ differentiation occurs independently of parasite virulence or any known IRG-ROP5 interaction. Consistent with this, removal of ROP5 is not enough to elicit maximal CD8 T cell IFNγ production to parasite-infected cells. Instead, macrophage expression of the pathogen sensors, NLRP3 and to a large extent NLRP1, were absolute requirements. Other members of the conventional inflammasome cascade are only partially required, as revealed by decreased but not abrogated T57 IFNγ responses to parasite-infected ASC, caspase-1/11, and gasdermin D deficient cells. Moreover, IFNγ production was only partially reduced in the absence of IL-12, IL-18 or IL-1R signaling. In summary, T. gondii effectors and host machinery that modulate parasitophorous vacuolar membranes, as well as NLR-dependent but inflammasome-independent pathways, determine the full commitment of CD8 T cells IFNγ responses to a vacuolar antigen.
-
-
-
In vivo experiments
-
Cancer Research
-
Immunology and Microbiology
Systemic dysfunction and plasticity of the immune macroenvironment in cancer models.
In Nat Med on 1 July 2020 by Allen, B. M., Hiam, K. J., et al.
PubMed
Understanding of the factors governing immune responses in cancer remains incomplete, limiting patient benefit. In this study, we used mass cytometry to define the systemic immune landscape in response to tumor development across five tissues in eight mouse tumor models. Systemic immunity was dramatically altered across models and time, with consistent findings in the peripheral blood of patients with breast cancer. Changes in peripheral tissues differed from those in the tumor microenvironment. Mice with tumor-experienced immune systems mounted dampened responses to orthogonal challenges, including reduced T cell activation during viral or bacterial infection. Antigen-presenting cells (APCs) mounted weaker responses in this context, whereas promoting APC activation rescued T cell activity. Systemic immune changes were reversed with surgical tumor resection, and many were prevented by interleukin-1 or granulocyte colony-stimulating factor blockade, revealing remarkable plasticity in the systemic immune state. These results demonstrate that tumor development dynamically reshapes the composition and function of the immune macroenvironment.
-
-
-
Immunology and Microbiology
Neonatal-derived IL-17 producing dermal γδ T cells are required to prevent spontaneous atopic dermatitis
In bioRxiv on 28 June 2019 by Spidale, N., Malhotra, N., et al.
-
-
-
In vivo experiments
-
Immunology and Microbiology
Anti-commensal IgG Drives Intestinal Inflammation and Type 17 Immunity in Ulcerative Colitis.
In Immunity on 16 April 2019 by Castro-Dopico, T., Dennison, T. W., et al.
PubMed
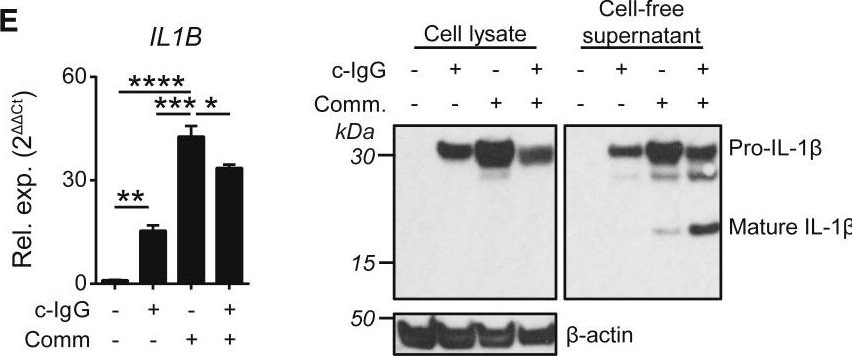
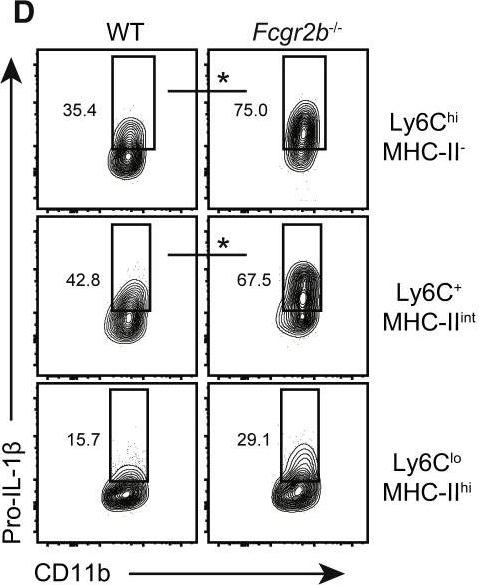
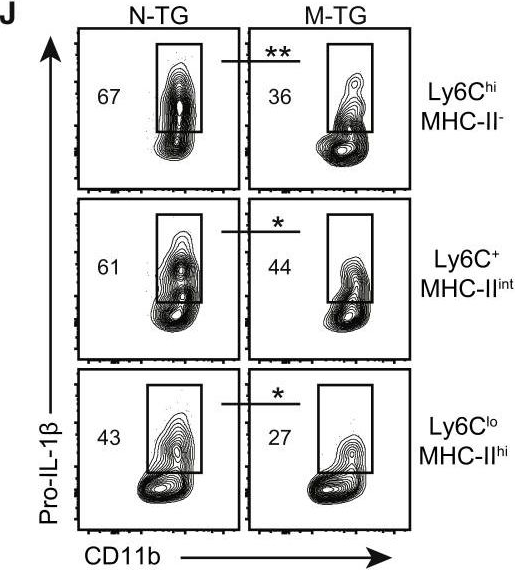
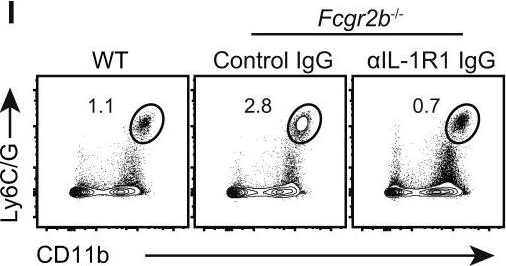
Inflammatory bowel disease is a chronic, relapsing condition with two subtypes, Crohn's disease (CD) and ulcerative colitis (UC). Genome-wide association studies (GWASs) in UC implicate a FCGR2A variant that alters the binding affinity of the antibody receptor it encodes, FcγRIIA, for immunoglobulin G (IgG). Here, we aimed to understand the mechanisms whereby changes in FcγRIIA affinity would affect inflammation in an IgA-dominated organ. We found a profound induction of anti-commensal IgG and a concomitant increase in activating FcγR signaling in the colonic mucosa of UC patients. Commensal-IgG immune complexes engaged gut-resident FcγR-expressing macrophages, inducing NLRP3- and reactive-oxygen-species-dependent production of interleukin-1β (IL-1β) and neutrophil-recruiting chemokines. These responses were modulated by the FCGR2A genotype. In vivo manipulation of macrophage FcγR signal strength in a mouse model of UC determined the magnitude of intestinal inflammation and IL-1β-dependent type 17 immunity. The identification of an important contribution of IgG-FcγR-dependent inflammation to UC has therapeutic implications.
-
-
-
Inhibition experiments
-
Immunology and Microbiology
IL-6 receptor blockade corrects defects of XIAP-deficient regulatory T cells.
In Nat Commun on 31 January 2018 by Hsieh, W. C., Hsu, T. S., et al.
PubMed
X-linked lymphoproliferative syndrome type-2 (XLP-2) is a primary immunodeficiency disease attributed to XIAP mutation and is triggered by infection. Here, we show that mouse Xiap-/- regulatory T (Treg) cells and human XIAP-deficient Treg cells are defective in suppressive function. The Xiap-/- Treg cell defect is linked partly to decreased SOCS1 expression. XIAP binds SOCS1 and promotes SOCS1 stabilization. Foxp3 stability is reduced in Xiap-/- Treg cells. In addition, Xiap-/- Treg cells are prone to IFN-γ secretion. Transfer of wild-type Treg cells partly rescues infection-induced inflammation in Xiap-/- mice. Notably, inflammation-induced reprogramming of Xiap-/- Treg cells can be prevented by blockade of the IL-6 receptor (IL-6R), and a combination of anti-IL-6R and Xiap-/- Treg cells confers survival to inflammatory infection in Xiap-/- mice. Our results suggest that XLP-2 can be corrected by combination treatment with autologous iTreg (induced Treg) cells and anti-IL-6R antibody, bypassing the necessity to transduce Treg cells with XIAP.
-
-
-
In vivo experiments
-
Immunology and Microbiology
Cutaneous Leishmaniasis Induces a Transmissible Dysbiotic Skin Microbiota that Promotes Skin Inflammation.
In Cell Host Microbe on 12 July 2017 by Gimblet, C., Meisel, J. S., et al.
PubMed
Skin microbiota can impact allergic and autoimmune responses, wound healing, and anti-microbial defense. We investigated the role of skin microbiota in cutaneous leishmaniasis and found that human patients infected with Leishmania braziliensis develop dysbiotic skin microbiota, characterized by increases in the abundance of Staphylococcus and/or Streptococcus. Mice infected with L. major exhibit similar changes depending upon disease severity. Importantly, this dysbiosis is not limited to the lesion site, but is transmissible to normal skin distant from the infection site and to skin from co-housed naive mice. This observation allowed us to test whether a pre-existing dysbiotic skin microbiota influences disease, and we found that challenging dysbiotic naive mice with L. major or testing for contact hypersensitivity results in exacerbated skin inflammatory responses. These findings demonstrate that a dysbiotic skin microbiota is not only a consequence of tissue stress, but also enhances inflammation, which has implications for many inflammatory cutaneous diseases.
-