InVivoMAb anti-mouse CD80 (B7-1)
Product Description
Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Dibutyryl cAMP-Activated 5C2 cells |
| Reported Applications |
in vivo CD80 blockade Affinity chromatography |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
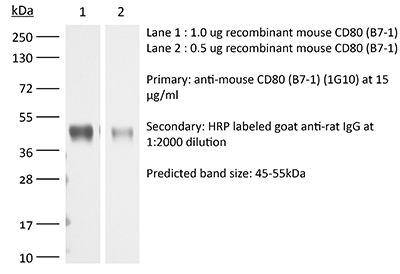
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10950113 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
Affinity chromatography
Patel, J. M., et al (2015). "Plasma membrane vesicles decorated with glycolipid-anchored antigens and adjuvants via protein transfer as an antigen delivery platform for inhibition of tumor growth" Biomaterials 74: 231-244.
PubMed
Antigen delivered within particulate materials leads to enhanced antigen-specific immunity compared to soluble administration of antigen. However, current delivery approaches for antigen encapsulated in synthetic particulate materials are limited by the complexity of particle production that affects stability and immunogenicity of the antigen. Herein, we describe a protein delivery system that utilizes plasma membrane vesicles (PMVs) derived from biological materials such as cultured cells or isolated tissues and a simple protein transfer technology. We show that these particulate PMVs can be easily modified within 4 h by a protein transfer process to stably incorporate a glycosylphosphatidylinositol (GPI)-anchored form of the breast cancer antigen HER-2 onto the PMV surface. Immunization of mice with GPI-HER-2-modified-PMVs induced strong HER-2-specific antibody responses and protection from tumor challenge in two different breast cancer models. Further incorporation of the immunostimulatory molecules IL-12 and B7-1 onto the PMVs by protein transfer enhanced tumor protection and induced beneficial Th1 and Th2-type HER-2-specific immune responses. Since protein antigens can be easily converted to GPI-anchored forms, these results demonstrate that isolated plasma membrane vesicles can be modified with desired antigens along with immunostimulatory molecules by protein transfer and used as a vaccine delivery vehicle to elicit potent antigen-specific immunity.
in vivo B7-1 blockade
Fankhauser, S. C. and M. N. Starnbach (2014). "PD-L1 limits the mucosal CD8+ T cell response to Chlamydia trachomatis" J Immunol 192(3): 1079-1090.
PubMed
Chlamydia trachomatis infection is the most common bacterial sexually transmitted disease in the United States. Repeated infections with C. trachomatis lead to serious sequelae, such as infertility. It is unclear why the adaptive immune system, specifically the CD8(+) T cell response, is unable to protect against subsequent C. trachomatis infections. In this article, we characterize the mucosal CD8(+) T cell response to C. trachomatis in the murine genital tract. We demonstrate that the immunoinhibitory ligand, PD-L1, contributes to the defective CD8(+) T cell response. Deletion or inhibition of PD-L1 restores the CD8(+) T cell response and enhances C. trachomatis clearance.
in vivo B7-1 blockade
Bagenstose, L. M., et al (2002). "B7-1 and B7-2 co-stimulatory molecules are required for mercury-induced autoimmunity" Clin Exp Immunol 127(1): 12-19.
PubMed
B7-1 (CD80) and B7-2 (CD86) molecules on antigen presenting cells play important roles in providing co-stimulatory signals required for activation and expansion of autoreactive T cells. Moreover, some reports have suggested that these molecules may have distinct functions in the differentiation of Th1 and Th2 cells. Mercury-induced autoimmunity in H-2s mice is characterized by lymphoproliferation of T and B cells, serum increases in IgG1 and IgE and production of antinucleolar antibodies (ANoA). The mechanisms responsible for the various manifestations of this syndrome have yet to be elucidated. To examine the contributions of B7 co-stimulatory molecules to this model, susceptible mice were treated with antibodies to B7-1, B7-2, or both during the development of mercury-induced autoimmunity. The combination of anti-B7-1 and anti-B7-2 antibodies prevented Hg-induced disease in H-2s mice. Additionally, single anti-B7-1 antibody treatment was sufficient to prevent Hg-induced ANoA production, but not IgG1 and IgE hypergammaglobulinaemia. Further, single antibody treatment with anti-B7-2 resulted in a partial reduction of ANoA titres but had no significant effect on total serum IgG1 and IgE levels. Taken together, these results indicate that B7-1 and B7-2 molecules are critical for the development of Hg-induced autoimmunity and suggest that the different manifestations of the syndrome are regulated by independent mechanisms.
Product Citations
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Post-immunotherapy CTLA-4 Ig treatment improves antitumor efficacy.
In Proc Natl Acad Sci U S A on 2 July 2024 by Mok, S., Ağaç Çobanoğlu, D., et al.
PubMed
Immune checkpoint therapies (ICT) improve overall survival of patients with cancer but may cause immune-related adverse events (irAEs) such as myocarditis. Cytotoxic T lymphocyte-associated antigen 4 immunoglobulin fusion protein (CTLA-4 Ig), an inhibitor of T cell costimulation through CD28, reverses irAEs in animal models. However, concerns exist about potentially compromising antitumor response of ICT. In mouse tumor models, we administered CTLA-4 Ig 1) concomitantly with ICT or 2) after ICT completion. Concomitant treatment reduced antitumor efficacy, while post-ICT administration improved efficacy without affecting frequency and function of CD8 T cells. The improved response was independent of the ICT used, whether CTLA-4 or PD-1 blockade. The frequency of Tregs was significantly decreased with CTLA-4 Ig. The resulting increased CD8/Treg ratio potentially underlies the enhanced efficacy of ICT followed by CTLA-4 Ig. This paradoxical mechanism shows that a CTLA-4 Ig regimen shown to reduce irAE severity does not compromise antitumor efficacy.
-
-
-
Immunology and Microbiology
PD-L1 signaling selectively regulates T cell lymphatic transendothelial migration.
In Nat Commun on 21 April 2022 by Piao, W., Li, L., et al.
PubMed
Programmed death-1 (PD-1) and its ligand PD-L1 are checkpoint molecules which regulate immune responses. Little is known about their functions in T cell migration and there are contradictory data about their roles in regulatory T cell (Treg) function. Here we show activated Tregs and CD4 effector T cells (Teffs) use PD-1/PD-L1 and CD80/PD-L1, respectively, to regulate transendothelial migration across lymphatic endothelial cells (LECs). Antibody blockade of Treg PD-1, Teff CD80 (the alternative ligand for PD-L1), or LEC PD-L1 impairs Treg or Teff migration in vitro and in vivo. PD-1/PD-L1 signals through PI3K/Akt and ERK to regulate zipper junctional VE-cadherin, and through NFκB-p65 to up-regulate VCAM-1 expression on LECs. CD80/PD-L1 signaling up-regulates VCAM-1 through ERK and NFκB-p65. PD-1 and CD80 blockade reduces tumor egress of PD-1high fragile Tregs and Teffs into draining lymph nodes, respectively, and promotes tumor regression. These data provide roles for PD-L1 in cell migration and immune regulation.
-
-
-
Blocking experiments
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Unregulated antigen-presenting cell activation by T cells breaks self tolerance.
In Proc Natl Acad Sci U S A on 15 January 2019 by Yi, J., Jung, J., et al.
PubMed
T cells proliferate vigorously following acute depletion of CD4+ Foxp3+ T regulatory cells [natural Tregs (nTregs)] and also when naive T cells are transferred to syngeneic, nTreg-deficient Rag1-/- hosts. Here, using mice raised in an antigen-free (AF) environment, we show that proliferation in these two situations is directed to self ligands rather than food or commensal antigens. In both situations, the absence of nTregs elevates B7 expression on host dendritic cells (DCs) and enables a small subset of naive CD4 T cells with high self affinity to respond overtly to host DCs: bidirectional T/DC interaction ensues, leading to progressive DC activation and reciprocal strong proliferation of T cells accompanied by peripheral Treg (pTreg) formation. Likewise, high-affinity CD4 T cells proliferate vigorously and form pTregs when cultured with autologous DCs in vitro in the absence of nTregs: this anti-self response is MHCII/peptide dependent and elicited by the raised level of B7 on cultured DCs. The data support a model in which self tolerance is imposed via modulation of CD28 signaling and explains the pathological effects of superagonistic CD28 antibodies.
-
-
-
Affinity chromatography
-
Cricetulus griseus (Chinese hamster)
-
Cancer Research
-
Immunology and Microbiology
Plasma membrane vesicles decorated with glycolipid-anchored antigens and adjuvants via protein transfer as an antigen delivery platform for inhibition of tumor growth.
In Biomaterials on 1 January 2016 by Patel, J. M., Vartabedian, V. F., et al.
PubMed
Antigen delivered within particulate materials leads to enhanced antigen-specific immunity compared to soluble administration of antigen. However, current delivery approaches for antigen encapsulated in synthetic particulate materials are limited by the complexity of particle production that affects stability and immunogenicity of the antigen. Herein, we describe a protein delivery system that utilizes plasma membrane vesicles (PMVs) derived from biological materials such as cultured cells or isolated tissues and a simple protein transfer technology. We show that these particulate PMVs can be easily modified within 4 h by a protein transfer process to stably incorporate a glycosylphosphatidylinositol (GPI)-anchored form of the breast cancer antigen HER-2 onto the PMV surface. Immunization of mice with GPI-HER-2-modified-PMVs induced strong HER-2-specific antibody responses and protection from tumor challenge in two different breast cancer models. Further incorporation of the immunostimulatory molecules IL-12 and B7-1 onto the PMVs by protein transfer enhanced tumor protection and induced beneficial Th1 and Th2-type HER-2-specific immune responses. Since protein antigens can be easily converted to GPI-anchored forms, these results demonstrate that isolated plasma membrane vesicles can be modified with desired antigens along with immunostimulatory molecules by protein transfer and used as a vaccine delivery vehicle to elicit potent antigen-specific immunity.
-