InVivoMAb anti-mouse CD19
Product Details
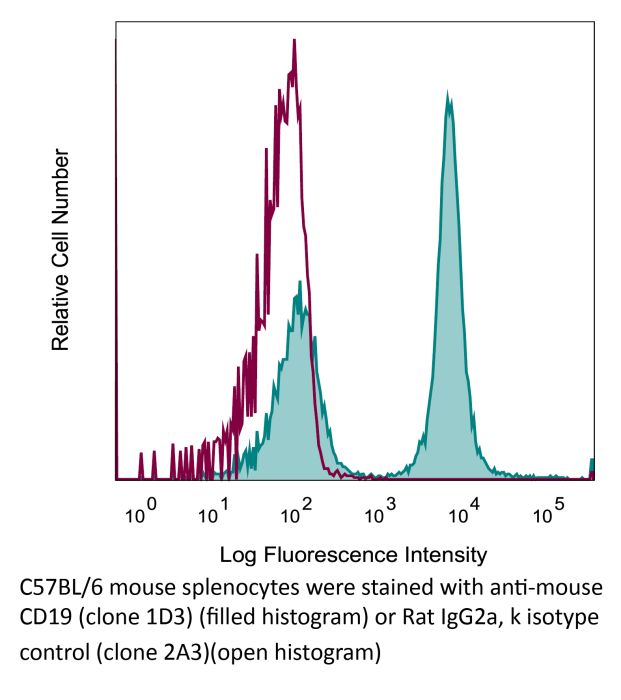
The 1D3 monoclonal antibody reacts with mouse CD19, a B cell-specific 95 kDa transmembrane glycoprotein of the immunoglobulin superfamily. CD19 contains two extracellular immunoglobulin-like domains and an extensive cytoplasmic tail. It functions as a positive regulator of B-cell receptor signaling in conjunction with CD21 and CD81. CD19 is highly expressed in most lymphomas and leukemias including some early B-cell malignancies that do not express CD20. For these reasons CD19 is quickly becoming an attractive alternative target for the immunotherapy of lymphoproliferative disorders. The 1D3 antibody has been reported to deplete B cells however, B cell depletion often requires treatment with a combination of 1D3, anti-mouse B220 (clone RA3.3A1/6.1), anti-mouse CD22 (clone Cy34.1), and anti-rat κ light chain (clone MAR 18.5) antibodies. Please see the provided references for protocol details.Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | K562 cells expressing the extracellular domain of mouse CD19 |
| Reported Applications |
in vivo B cell depletion in vivo CD19 neutralization in vitro B cell negative selection Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_10949187 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
in vivo B cell depletion
Sawen, P., et al. (2016). "Mitotic History Reveals Distinct Stem Cell Populations and Their Contributions to Hematopoiesis" Cell Rep 14(12): 2809-2818. PubMed
Homeostasis of short-lived blood cells is dependent on rapid proliferation of immature precursors. Using a conditional histone 2B-mCherry-labeling mouse model, we characterize hematopoietic stem cell (HSC) and progenitor proliferation dynamics in steady state and following several types of induced stress. HSC proliferation following HSC transplantation into lethally irradiated mice is fundamentally different not only from native hematopoiesis but also from other stress contexts. Whereas transplantation promoted sustained, long-term proliferation of HSCs, both cytokine-induced mobilization and acute depletion of selected blood cell lineages elicited very limited recruitment of HSCs to the proliferative pool. By coupling mCherry-based analysis of proliferation history with multiplex gene expression analyses on single cells, we have found that HSCs can be stratified into four distinct subtypes. These subtypes have distinct molecular signatures and differ significantly in their reconstitution potentials, showcasing the power of tracking proliferation history when resolving functional heterogeneity of HSCs.
Flow Cytometry
Becker, A. M., et al. (2015). "ADAM17 limits the expression of CSF1R on murine hematopoietic progenitors" Exp Hematol 43(1): 44-52 e41-43. PubMed
All-lymphoid progenitors (ALPs) yield few myeloid cells in vivo, but readily generate such cells in vitro. The basis for this difference remains unknown. We hypothesized that ALPs limit responsiveness to in vivo concentrations of myeloid-promoting cytokines by reducing expression of the corresponding receptors, potentially through posttranscriptional mechanisms. Consistent with such a mechanism, ALPs express higher levels of CSF1R transcripts than their upstream precursors, yet show limited cell-surface protein expression of colony-stimulating factor 1 receptor (CSF1R). All-lymphoid progenitors and other hematopoietic progenitors deficient in A disintegrin and metalloproteinase domain 17 (ADAM17), display elevated cell surface CSF1R expression. ADAM17(-/-) ALPs, however, fail to yield myeloid cells upon transplantation into irradiated recipients. Moreover, ADAM17(-/-) ALPs yield fewer macrophages in vitro than control ALPs at high concentrations of macrophage colony stimulating factor. Mice with hematopoietic-specific deletion of ADAM17 have normal numbers of myeloid and lymphoid progenitors and mature cells in vivo. These data demonstrate that ADAM17 limits CSF1R protein expression on hematopoietic progenitors, but that compensatory mechanisms prevent elevated CSF1R levels from altering lymphoid progenitor potential.
in vivo B cell depletion
Carmi, Y., et al. (2015). "Allogeneic IgG combined with dendritic cell stimuli induce antitumour T-cell immunity" Nature 521(7550): 99-104. PubMed
Whereas cancers grow within host tissues and evade host immunity through immune-editing and immunosuppression, tumours are rarely transmissible between individuals. Much like transplanted allogeneic organs, allogeneic tumours are reliably rejected by host T cells, even when the tumour and host share the same major histocompatibility complex alleles, the most potent determinants of transplant rejection. How such tumour-eradicating immunity is initiated remains unknown, although elucidating this process could provide the basis for inducing similar responses against naturally arising tumours. Here we find that allogeneic tumour rejection is initiated in mice by naturally occurring tumour-binding IgG antibodies, which enable dendritic cells (DCs) to internalize tumour antigens and subsequently activate tumour-reactive T cells. We exploited this mechanism to treat autologous and autochthonous tumours successfully. Either systemic administration of DCs loaded with allogeneic-IgG-coated tumour cells or intratumoral injection of allogeneic IgG in combination with DC stimuli induced potent T-cell-mediated antitumour immune responses, resulting in tumour eradication in mouse models of melanoma, pancreas, lung and breast cancer. Moreover, this strategy led to eradication of distant tumours and metastases, as well as the injected primary tumours. To assess the clinical relevance of these findings, we studied antibodies and cells from patients with lung cancer. T cells from these patients responded vigorously to autologous tumour antigens after culture with allogeneic-IgG-loaded DCs, recapitulating our findings in mice. These results reveal that tumour-binding allogeneic IgG can induce powerful antitumour immunity that can be exploited for cancer immunotherapy.
in vitro B cell negative selection
Liu, B., et al. (2015). "Collaborative interactions between type 2 innate lymphoid cells and antigen-specific CD4+ Th2 cells exacerbate murine allergic airway diseases with prominent eosinophilia" J Immunol 194(8): 3583-3593. PubMed
Type-2 innate lymphoid cells (ILC2s) and the acquired CD4(+) Th2 and Th17 cells contribute to the pathogenesis of experimental asthma; however, their roles in Ag-driven exacerbation of chronic murine allergic airway diseases remain elusive. In this study, we report that repeated intranasal rechallenges with only OVA Ag were sufficient to trigger airway hyperresponsiveness, prominent eosinophilic inflammation, and significantly increased serum OVA-specific IgG1 and IgE in rested mice that previously developed murine allergic airway diseases. The recall response to repeated OVA inoculation preferentially triggered a further increase of lung OVA-specific CD4(+) Th2 cells, whereas CD4(+) Th17 and ILC2 cell numbers remained constant. Furthermore, the acquired CD4(+) Th17 cells in Stat6(-/-)/IL-17-GFP mice, or innate ILC2s in CD4(+) T cell-ablated mice, failed to mount an allergic recall response to OVA Ag. After repeated OVA rechallenge or CD4(+) T cell ablation, the increase or loss of CD4(+) Th2 cells resulted in an enhanced or reduced IL-13 production by lung ILC2s in response to IL-25 and IL-33 stimulation, respectively. In return, ILC2s enhanced Ag-mediated proliferation of cocultured CD4(+) Th2 cells and their cytokine production, and promoted eosinophilic airway inflammation and goblet cell hyperplasia driven by adoptively transferred Ag-specific CD4(+) Th2 cells. Thus, these results suggest that an allergic recall response to recurring Ag exposures preferentially triggers an increase of Ag-specific CD4(+) Th2 cells, which facilitates the collaborative interactions between acquired CD4(+) Th2 cells and innate ILC2s to drive the exacerbation of a murine allergic airway diseases with an eosinophilic phenotype.
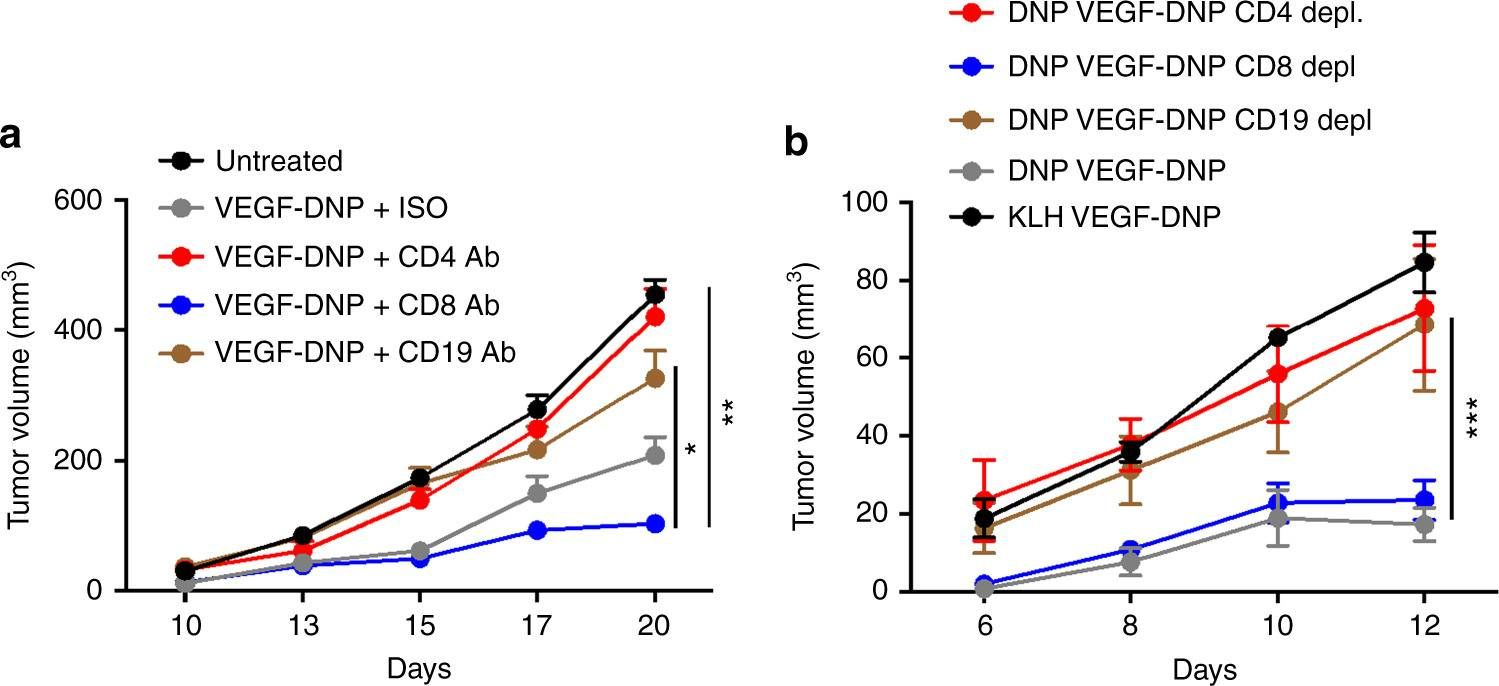
in vivo CD19 neutralization, Flow Cytometry
Dai, M., et al. (2015). "Curing mice with large tumors by locally delivering combinations of immunomodulatory antibodies" Clin Cancer Res 21(5): 1127-1138. PubMed
PURPOSE: Immunomodulatory mAbs can treat cancer, but cures are rare except for small tumors. Our objective was to explore whether the therapeutic window increases by combining mAbs with different modes of action and injecting them into tumors. EXPERIMENTAL DESIGN: Combinations of mAbs to CD137/PD-1/CTLA-4 or CD137/PD-1/CTLA-4/CD19 were administrated intratumorally to mice with syngeneic tumors (B16 and SW1 melanoma, TC1 lung carcinoma), including tumors with a mean surface of approximately 80 mm(2). Survival and tumor growth were assessed. Immunologic responses were evaluated using flow cytometry and qRT-PCR. RESULTS: More than 50% of tumor-bearing mice had complete regression and long-term survival after tumor injection with mAbs recognizing CD137/PD-1/CTLA-4/CD19 with similar responses in three models. Intratumoral injection was more efficacious than intraperitoneal injection in causing rejection also of untreated tumors in the same mice. The three-mAb combination could also induce regression, but was less efficacious. There were few side effects, and therapy-resistant tumors were not observed. Transplanted tumor cells rapidly caused a Th2 response with increased CD19 cells. Successful therapy shifted this response to the Th1 phenotype with decreased CD19 cells and increased numbers of long-term memory CD8 effector cells and T cells making IFNgamma and TNFalpha. CONCLUSIONS: Intratumoral injection of mAbs recognizing CD137/PD-1/CTLA-4/CD19 can eradicate established tumors and reverse a Th2 response with tumor-associated CD19 cells to Th1 immunity, whereas a combination lacking anti-CD19 is less effective. There are several human cancers for which a similar approach may provide clinical benefit.
in vitro B cell negative selection
Bouffi, C., et al. (2015). "Transcription Factor Repertoire of Homeostatic Eosinophilopoiesis" J Immunol 195(6): 2683-2695. PubMed
The production of mature eosinophils (Eos) is a tightly orchestrated process with the aim to sustain normal Eos levels in tissues while also maintaining low numbers of these complex and sensitive cells in the blood. To identify regulators of homeostatic eosinophilopoiesis in mice, we took a global approach to identify genome-wide transcriptome and epigenome changes that occur during homeostasis at critical developmental stages, including Eos-lineage commitment and lineage maturation. Our analyses revealed a markedly greater number of transcriptome alterations associated with Eos maturation (1199 genes) than with Eos-lineage commitment (490 genes), highlighting the greater transcriptional investment necessary for differentiation. Eos-lineage-committed progenitors (EoPs) were noted to express high levels of granule proteins and contain granules with an ultrastructure distinct from that of mature resting Eos. Our analyses also delineated a 976-gene Eos-lineage transcriptome that included a repertoire of 56 transcription factors, many of which have never previously been associated with Eos. EoPs and Eos, but not granulocyte-monocyte progenitors or neutrophils, expressed Helios and Aiolos, members of the Ikaros family of transcription factors, which regulate gene expression via modulation of chromatin structure and DNA accessibility. Epigenetic studies revealed a distinct distribution of active chromatin marks between genes induced with lineage commitment and genes induced with cell maturation during Eos development. In addition, Aiolos and Helios binding sites were significantly enriched in genes expressed by EoPs and Eos with active chromatin, highlighting a potential novel role for Helios and Aiolos in regulating gene expression during Eos development.
in vivo B cell depletion
Guo, Z., et al. (2013). "Combined TIM-3 blockade and CD137 activation affords the long-term protection in a murine model of ovarian cancer" J Transl Med 11: 215. PubMed
BACKGROUND: T-cell immunoglobulin and mucin domain 3 (TIM-3) is known as a negative immune regulator and emerging data have implicated TIM-3 a pivotal role in suppressing antitumor immunity. The co-stimulatory receptor CD137 is transiently upregulated on T-cells following activation and increases their proliferation and survival when engaged. Although antagonistic anti-TIM-3 or agonistic anti-CD137 antibodies can promote the rejection of several murine tumors, some poorly immunogenic tumors were refractory to this treatment. In this study, we sought to evaluate whether combined TIM-3 blockade and CD137 activation would significantly improve the immunotherapy in the murine ID8 ovarian cancer model. METHODS: Mice with established ID8 tumor were intraperitoneally injected with single or combined anti-TIM-3/CD137 monoclonal antibody (mAb); mice survival was recorded, the composition and gene expression of tumor-infiltrating immune cells in these mice was analyzed by flow cytometry and quantitative RT-PCR respectively, and the function of CD8(+) cells was evaluated by ELISA and cytotoxicity assay. RESULTS: Either anti-TIM-3 or CD137 mAb alone, although effective in 3 days established tumor, was unable to prevent tumor progression in mice bearing 10 days established tumor, however, combined anti-TIM-3/CD137 mAb significantly inhibited the growth of these tumors with 60% of mice tumor free 90 days after tumor inoculation. Therapeutic efficacy was associated with a systemic immune response with memory and antigen specificity, required CD4(+) cells and CD8(+) cells. The 2 mAb combination increased CD4(+) and CD8(+) cells and decreased immunosuppressive CD4(+)FoxP3(+) regulatory T (Treg) cells and CD11b(+)Gr-1(+) myeloid suppressor cells (MDSC) at tumor sites, giving rise to significantly elevated ratios of CD4(+) and CD8(+) cells to Treg and MDSC; This is consistent with biasing local immune response towards an immunostimulatory Th1 type and is further supported by quantitative RT-PCR data showing the increased Th1-associated genes by anti-TIM-3/CD137 treatment. The increased CD8(+) T cells produced high level of IFN-gamma upon tumor antigen stimulation and displayed antigen-specific cytotoxic activity. CONCLUSIONS: To our knowledge, this is the first report investigating the effects of anti-TIM-3/CD137 combined mAb in a murine ovarian cancer model, and our results may aid the design of future trials for ovarian cancer immunotherapy.
in vivo CD19 neutralization, Flow Cytometry
Dai, M., et al. (2013). "Long-lasting complete regression of established mouse tumors by counteracting Th2 inflammation" J Immunother 36(4): 248-257. PubMed
40% of mice with SW1 tumors remained healthy >150 days after last treatment and are probably cured. Therapeutic efficacy was associated with a systemic immune response with memory and antigen specificity, required CD4 cells and involved CD8 cells and NK cells to a less extent. The 3 mAb combination significantly decreased CD19 cells at tumor sites, increased IFN-gamma and TNF-alpha producing CD4 and CD8 T cells and mature CD86 dendritic cells (DC), and it increased the ratios of effector CD4 and CD8 T cells to CD4Foxp3 regulatory T (Treg) cells and to CD11bGr-1 myeloid suppressor cells (MDSC). This is consistent with shifting the tumor microenvironment from an immunosuppressive Th2 to an immunostimulatory Th1 type and is further supported by PCR data. Adding an anti-CD19 mAb to the 3 mAb combination in the SW1 model further increased therapeutic efficacy. Data from ongoing experiments show that intratumoral injection of a combination of mAbs to CD137PD-1CTLA4CD19 can induce complete regression and dramatically prolong survival also in the TC1 carcinoma and B16 melanoma models, suggesting that the approach has general validity.”}” data-sheets-userformat=”{“2″:14851,”3”:{“1″:0},”4”:{“1″:2,”2″:16777215},”12″:0,”14”:{“1″:2,”2″:1521491},”15″:”Roboto, sans-serif”,”16″:12}”>Mice with intraperitoneal ID8 ovarian carcinoma or subcutaneous SW1 melanoma were injected with monoclonal antibodies (mAbs) to CD137PD-1CTLA4 7-15 days after tumor initiation. Survival of mice with ID8 tumors tripled and >40% of mice with SW1 tumors remained healthy >150 days after last treatment and are probably cured. Therapeutic efficacy was associated with a systemic immune response with memory and antigen specificity, required CD4 cells and involved CD8 cells and NK cells to a less extent. The 3 mAb combination significantly decreased CD19 cells at tumor sites, increased IFN-gamma and TNF-alpha producing CD4 and CD8 T cells and mature CD86 dendritic cells (DC), and it increased the ratios of effector CD4 and CD8 T cells to CD4Foxp3 regulatory T (Treg) cells and to CD11bGr-1 myeloid suppressor cells (MDSC). This is consistent with shifting the tumor microenvironment from an immunosuppressive Th2 to an immunostimulatory Th1 type and is further supported by PCR data. Adding an anti-CD19 mAb to the 3 mAb combination in the SW1 model further increased therapeutic efficacy. Data from ongoing experiments show that intratumoral injection of a combination of mAbs to CD137PD-1CTLA4CD19 can induce complete regression and dramatically prolong survival also in the TC1 carcinoma and B16 melanoma models, suggesting that the approach has general validity.
in vitro B cell negative selection, Flow Cytometry
De Obaldia, M. E., et al. (2013). "T cell development requires constraint of the myeloid regulator C/EBP-alpha by the Notch target and transcriptional repressor Hes1" Nat Immunol 14(12): 1277-1284. PubMed
Notch signaling induces gene expression of the T cell lineage and discourages alternative fate outcomes. Hematopoietic deficiency in the Notch target Hes1 results in severe T cell lineage defects; however, the underlying mechanism is unknown. We found here that Hes1 constrained myeloid gene-expression programs in T cell progenitor cells, as deletion of the myeloid regulator C/EBP-alpha restored the development of T cells from Hes1-deficient progenitor cells. Repression of Cebpa by Hes1 required its DNA-binding and Groucho-recruitment domains. Hes1-deficient multipotent progenitor cells showed a developmental bias toward myeloid cells and dendritic cells after Notch signaling, whereas Hes1-deficient lymphoid progenitor cells required additional cytokine signaling for diversion into the myeloid lineage. Our findings establish the importance of constraining developmental programs of the myeloid lineage early in T cell development.
Flow Cytometry
Purtha, W. E., et al. (2012). "Spontaneous mutation of the Dock2 gene in Irf5-/- mice complicates interpretation of type I interferon production and antibody responses" Proc Natl Acad Sci U S A 109(15): E898-904. PubMed
Genome-wide studies have identified associations between polymorphisms in the IFN regulatory factor-5 (Irf5) gene and a variety of human autoimmune diseases. Its functional role in disease pathogenesis, however, remains unclear, as studies in Irf5(-/-) mice have reached disparate conclusions regarding the importance of this transcription factor in type I IFN production and antibody responses. We identified a spontaneous genomic duplication and frameshift mutation in the guanine exchange factor dedicator of cytokinesis 2 (Dock2) that has arisen in at least a subset of circulating Irf5(-/-) mice and inadvertently been bred to homozygosity. Retroviral expression of DOCK2, but not IRF-5, rescued defects in plasmacytoid dendritic cell and B-cell development, and Irf5(-/-) mice lacking the mutation in Dock2 exhibited normal plasmacytoid dendritic cell and B-cell development, largely intact type I IFN responses, and relatively normal antibody responses to viral infection. Thus, confirmation of the normal Dock2 genotype in circulating Irf5(-/-) mice is warranted, and our data may partly explain conflicting results in this field.
in vivo B cell depletion
Keren, Z., et al. (2011). "B-cell depletion reactivates B lymphopoiesis in the BM and rejuvenates the B lineage in aging" Blood 117(11): 3104-3112. PubMed
Aging is associated with a decline in B-lymphopoiesis in the bone marrow and accumulation of long-lived B cells in the periphery. These changes decrease the body’s ability to mount protective antibody responses. We show here that age-related changes in the B lineage are mediated by the accumulating long-lived B cells. Thus, depletion of B cells in old mice was followed by expansion of multipotent primitive progenitors and common lymphoid progenitors, a revival of B-lymphopoiesis in the bone marrow, and generation of a rejuvenated peripheral compartment that enhanced the animal’s immune responsiveness to antigenic stimulation. Collectively, our results suggest that immunosenescence in the B-lineage is not irreversible and that depletion of the long-lived B cells in old mice rejuvenates the B-lineage and enhances immune competence.
Flow Cytometry
Purtha, W. E., et al. (2011). "Memory B cells, but not long-lived plasma cells, possess antigen specificities for viral escape mutants" J Exp Med 208(13): 2599-2606. PubMed
Memory B cells (MBCs) and long-lived plasma cells (LLPCs) persist after clearance of infection, yet the specific and nonredundant role MBCs play in subsequent protection is unclear. After resolution of West Nile virus infection in mice, we demonstrate that LLPCs were specific for a single dominant neutralizing epitope, such that immune serum poorly inhibited a variant virus that encoded a mutation at this critical epitope. In contrast, a large fraction of MBC produced antibody that recognized both wild-type (WT) and mutant viral epitopes. Accordingly, antibody produced by the polyclonal pool of MBC neutralized WT and variant viruses equivalently. Remarkably, we also identified MBC clones that recognized the mutant epitope better than the WT protein, despite never having been exposed to the variant virus. The ability of MBCs to respond to variant viruses in vivo was confirmed by experiments in which MBCs were adoptively transferred or depleted before secondary challenge. Our data demonstrate that class-switched MBC can respond to variants of the original pathogen that escape neutralization of antibody produced by LLPC without a requirement for accumulating additional somatic mutations.
- Genetics,
- Immunology and Microbiology
Immune profiling of adeno-associated virus response identifies B cell-specific targets that enable vector re-administration in mice.
In Gene Therapy on 1 May 2023 by Chen, M., Kim, B., et al.
PubMed
Adeno-associated virus (AAV) vector-based gene therapies can be applied to a wide range of diseases. AAV expression can last for months to years, but vector re-administration may be necessary to achieve life-long treatment. Unfortunately, immune responses against these vectors are potentiated after the first administration, preventing the clinical use of repeated administration of AAVs. Reducing the immune response against AAVs while minimizing broad immunosuppression would improve gene delivery efficiency and long-term safety. In this study, we quantified the contributions of multiple immune system components of the anti-AAV response in mice. We identified B-cell-mediated immunity as a critical component preventing vector re-administration. Additionally, we found that IgG depletion alone was insufficient to enable re-administration, suggesting IgM antibodies play an important role in the immune response against AAV. Further, we found that AAV-mediated transduction is improved in µMT mice that lack functional IgM heavy chains and cannot form mature B-cells relative to wild-type mice. Combined, our results suggest that B-cells, including non-class switched B-cells, are a potential target for therapeutics enabling AAV re-administration. Our results also suggest that the µMT mice are a potentially useful experimental model for gene delivery studies since they allow repeated dosing for more efficient gene delivery from AAVs. © 2022. The Author(s), under exclusive licence to Springer Nature Limited.
- Immunology and Microbiology
GPR55 in B cells limits atherosclerosis development and regulates plasma cell maturation.
In Nat Cardiovasc Res on 1 November 2022 by Guillamat-Prats, R., Hering, D., et al.
PubMed
Dissecting the pathways regulating the adaptive immune response in atherosclerosis is of particular therapeutic interest. Here we report that the lipid G-protein coupled receptor GPR55 is highly expressed by splenic plasma cells (PC), upregulated in mouse spleens during atherogenesis and human unstable or ruptured compared to stable plaques. Gpr55-deficient mice developed larger atherosclerotic plaques with increased necrotic core size compared to their corresponding controls. Lack of GPR55 hyperactivated B cells, disturbed PC maturation and resulted in immunoglobulin (Ig)G overproduction. B cell-specific Gpr55 depletion or adoptive transfer of Gpr55-deficient B cells was sufficient to promote plaque development and elevated IgG titers. In vitro, the endogenous GPR55 ligand lysophsophatidylinositol (LPI) enhanced PC proliferation, whereas GPR55 antagonism blocked PC maturation and increased their mitochondrial content. Collectively, these discoveries provide previously undefined evidence for GPR55 in B cells as a key modulator of the adaptive immune response in atherosclerosis.
- Cancer Research,
- Immunology and Microbiology
Tumor-infiltrated activated B cells suppress liver metastasis of colorectal cancers.
In Cell Reports on 30 August 2022 by Xu, Y., Wei, Z., et al.
PubMed
More than 40% of patients with late-stage colorectal cancer (CRC) develop liver metastasis (LM). Which immune cells play important roles in CRC-LM and contribute to the difference between left-sided CRC (LCC) and right-sided CRC (RCC) remain unclear. By single-cell RNA sequencing (scRNA-seq), we not only find that activated B cells are significantly depleted in CRC with LM, but also find a subtype of B cells developed from activated B cells, namely immature plasma cell population alpha (iMPA), highly correlated with metastasis. Mechanistically, inhibition of the Wnt and transforming growth factor β (TGF-β) pathways in cancer cell promotes activated B cell migration via the SDF-1-CXCR4 axis. This study reveals that B cell subpopulations in the tumor immune microenvironment (TIME) play a key role in CRC-LM as well as in LCC and RCC. The preventive effects of modulating B cell subpopulations in CRC may provide a rationale for subsequent drug development and CRC-LM management. Copyright © 2022 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
B Cells Are Required to Generate Optimal Anti-Melanoma Immunity in Response to Checkpoint Blockade.
In Frontiers in Immunology on 21 June 2022 by Singh, S., Roszik, J., et al.
PubMed
Immunotherapies such as checkpoint blockade therapies are known to enhance anti-melanoma CD8+ T cell immunity, but only a fraction of patients treated with these therapies achieve durable immune response and disease control. It may be that CD8+ T cells need help from other immune cells to generate effective and long-lasting anti-tumor immunity or that CD8+ T cells alone are insufficient for complete tumor regression and cure. Melanoma contains significant numbers of B cells; however, the role of B cells in anti-melanoma immunity is controversial. In this study, B16 melanoma mouse models were used to determine the role of B cells in anti-melanoma immunity. C57BL/6 mice, B cell knockout (KO) C57BL/6 mice, anti-CD19, and anti-CXCL13 antibody-treated C57BL/6 mice were used to determine treatment efficacy and generation of tumor-specific CD8+ T cells in response to PD-L1 blockade alone or combination with TLR-7/8 activation. Whole transcriptome analysis was performed on the tumors from B cell depleted and WT mice, untreated or treated with anti-PD-L1. Both CD40-positive and CD40-negative B cells were isolated from tumors of TLR-7/8 agonist-treated wild-type mice and adoptively transferred into tumor-bearing B cell KO mice, which were treated with anti-PD-L1 and TLR-7/8 agonist. Therapeutic efficacy was determined in the presence of activated or inactivated B cells. Microarray analysis was performed on TLR-7/8-treated tumors to look for the B cell signatures. We found B cells were required to enhance the therapeutic efficacy of monotherapy with anti-PD-L1 antibody and combination therapy with anti-PD-L1 antibody plus TLR-7/8 agonist. However, B cells were not essential for anti-CTLA-4 antibody activity. Interestingly, CD40-positive but not CD40-negative B cells contributed to anti-melanoma immunity. In addition, melanoma patients' TCGA data showed that the presence of B cell chemokine CXCL13 and B cells together with CD8+ T cells in tumors were strongly associated with improved overall survival. Our transcriptome data suggest that the absence of B cells enhances immune checkpoints expression in the tumors microenvironment. These results revealed the importance of B cells in the generation of effective anti-melanoma immunity in response to PD-1-PD-L1 blockade immunotherapy. Our findings may facilitate the design of more effective anti-melanoma immunotherapy. Copyright © 2022 Singh, Roszik, Saini, Singh, Bavisi, Wang, Vien, Yang, Kundu, Davis, Bover, Diab, Neelapu, Overwijk, Rai and Singh.
Targeted immunosuppression enhances repeated gene delivery
Preprint on Research Square on 1 March 2022 by Chen, M., Kim, B., et al.
PubMed
Adeno-associated virus (AAV) vector-based gene therapies can be applied to a wide range of diseases. AAV expression can last for months to years, but vector re-administration may be necessary to achieve life-long treatment. Unfortunately, immune system response against these vectors is potentiated after the first administration, which prevents the clinical use of repeated administration of AAVs. Reducing immune response against AAVs while minimizing immunosuppression would improve gene delivery efficiency and long-term safety. In this study, we quantified the contributions of multiple immune system components towards AAV response in mice. We identified B-cell-mediated immunity as a critical component preventing vector re-administration. Specifically, we found that IgG depletion was insufficient to enhance re-administration, suggesting the key role of B-cell mediated IgM antibodies in the immune response against AAV. Further, we also found that AAV-mediated transduction is improved compared to wild-type mice in µMT mice that lack functional IgM heavy chains and cannot form mature B-cells. Combined, our results suggest that IgM production in B cells is a potential target for therapeutics enabling AAV re-administration. Our results also suggest that the µMT mice are a potentially useful experimental model for gene delivery studies since they allow for up to 15-fold more efficient gene delivery.
- Immunology and Microbiology
GPR55 in B cells limits atherosclerosis development and regulates plasma cell maturation
Preprint on Research Square on 12 January 2022 by Guillamat-Prats, R., Hering, D., et al.
PubMed
Identifying novel pathways regulating the adaptive immune response in chronic inflammatory diseases such as atherosclerosis is of particular interest in view of developing new therapeutic drugs. Here we report that the lipid receptor GPR55 is highly expressed by splenic B cells and inversely correlates with atheroma plaque size in mice. In human carotid endarterectomy specimen, GPR55 transcript levels were significantly lower in unstable compared to stable carotid plaques. To study the impact of GPR55 deficiency in atherosclerosis, we crossed Gpr55 knockout mice with apolipoprotein E (ApoE) knockout mice and subjected the mice to Western diet for 4 to 16 weeks. Compared to ApoE-/- controls, ApoE-/-Gpr55-/- mice developed larger plaques with increased necrotic core size, associated with elevated circulating and aortic leukocyte counts. Flow cytometry, immunofluorescence and RNA-sequencing analysis of splenic B cells in these mice revealed a hyperactivated B cell phenotype with disturbed plasma cell maturation and immunoglobulin (Ig)G antibody overproduction. The specific contribution of B cell GPR55 in atherosclerosis was further studied in mixed Gpr55-/-/µMT bone marrow chimeras on low density receptor deficiency (Ldlr-/-) background, revealing that B-cell specific depletion of Gpr55 was sufficient to promote plaque development. Conversely, adoptive transfer of wildtype B cells into ApoE-/-Gpr55-/- mice blunted the proatherogenic phenotype. In vitro stimulation of splenocytes with the endogenous GPR55 ligand LPI promoted plasma cell proliferation and enhanced B cell activation marker expression, which was inhibited by the GPR55 antagonist CID16020046. Collectively, these discoveries provide new evidence for GPR55 as key modulator of the adaptive immune response in atherosclerosis. Targeting GPR55 could be useful to limit inflammation and plaque progression in patients suffering from atherosclerosis.
- Immunology and Microbiology
GPR55 in B cells limits atherosclerosis development and regulates plasma cell maturation
Preprint on BioRxiv : the Preprint Server for Biology on 21 December 2021 by Guillamat-Prats, R., Hering, D., et al.
PubMed
Identifying novel pathways regulating the adaptive immune response in chronic inflammatory diseases such as atherosclerosis is of particular interest in view of developing new therapeutic drugs. Here we report that the lipid receptor GPR55 is highly expressed by splenic B cells and inversely correlates with atheroma plaque size in mice. In human carotid endarterectomy specimen, GPR55 transcript levels were significantly lower in unstable compared to stable carotid plaques. To study the impact of GPR55 deficiency in atherosclerosis, we crossed Gpr55 knockout mice with apolipoprotein E ( ApoE ) knockout mice and subjected the mice to Western diet for 4 to 16 weeks. Compared to ApoE -/- controls, ApoE -/- Gpr55 -/- mice developed larger plaques with increased necrotic core size, associated with elevated circulating and aortic leukocyte counts. Flow cytometry, immunofluorescence and RNA-sequencing analysis of splenic B cells in these mice revealed a hyperactivated B cell phenotype with disturbed plasma cell maturation and immunoglobulin (Ig)G antibody overproduction. The specific contribution of B cell GPR55 in atherosclerosis was further studied in mixed Gpr55 -/- / µMT bone marrow chimeras on low density receptor deficiency ( Ldlr -/- ) background, revealing that B-cell specific depletion of Gpr55 was sufficient to promote plaque development. Conversely, adoptive transfer of wildtype B cells into ApoE -/- Gpr55 -/- mice blunted the proatherogenic phenotype. In vitro stimulation of splenocytes with the endogenous GPR55 ligand LPI promoted plasma cell proliferation and enhanced B cell activation marker expression, which was inhibited by the GPR55 antagonist CID16020046. Collectively, these discoveries provide new evidence for GPR55 as key modulator of the adaptive immune response in atherosclerosis. Targeting GPR55 could be useful to limit inflammation and plaque progression in patients suffering from atherosclerosis.
- Biochemistry and Molecular biology,
- Genetics,
- Immunology and Microbiology,
- Neuroscience
Single-cell RNA sequencing reveals B cell-related molecular biomarkers for Alzheimer's disease.
In Experimental & Molecular Medicine on 1 December 2021 by Xiong, L. L., Xue, L. L., et al.
PubMed
In recent years, biomarkers have been integrated into the diagnostic process and have become increasingly indispensable for obtaining knowledge of the neurodegenerative processes in Alzheimer's disease (AD). Peripheral blood mononuclear cells (PBMCs) in human blood have been reported to participate in a variety of neurodegenerative activities. Here, a single-cell RNA sequencing analysis of PBMCs from 4 AD patients (2 in the early stage, 2 in the late stage) and 2 normal controls was performed to explore the differential cell subpopulations in PBMCs of AD patients. A significant decrease in B cells was detected in the blood of AD patients. Furthermore, we further examined PBMCs from 43 AD patients and 41 normal subjects by fluorescence activated cell sorting (FACS), and combined with correlation analysis, we found that the reduction in B cells was closely correlated with the patients' Clinical Dementia Rating (CDR) scores. To confirm the role of B cells in AD progression, functional experiments were performed in early-stage AD mice in which fibrous plaques were beginning to appear; the results demonstrated that B cell depletion in the early stage of AD markedly accelerated and aggravated cognitive dysfunction and augmented the Aβ burden in AD mice. Importantly, the experiments revealed 18 genes that were specifically upregulated and 7 genes that were specifically downregulated in B cells as the disease progressed, and several of these genes exhibited close correlation with AD. These findings identified possible B cell-based AD severity, which are anticipated to be conducive to the clinical identification of AD progression. © 2021. The Author(s).
- Immunology and Microbiology
Statins act as transient type I interferon inhibitors to enable the antitumor activity of modified vaccinia Ankara viral vectors.
In Journal for Immunotherapy of Cancer on 1 July 2021 by Tenesaca, S., Vásquez, M., et al.
PubMed
Modified vaccinia virus Ankara (MVA) are genetically engineered non-replicating viral vectors. Intratumoral administration of MVA induces a cyclic GMP-AMP synthase-mediated type I interferon (IFN) response and the production of high levels of the transgenes engineered into the viral genome such as tumor antigens to construct cancer vaccines. Although type I IFNs are essential for establishing CD8-mediated antitumor responses, this cytokine family may also give rise to immunosuppressive mechanisms. In vitro assays were performed to evaluate the activity of simvastatin and atorvastatin on type I IFN signaling and on antigen presentation. Surface levels of IFN α/β receptor 1, endocytosis of bovine serum albumin-fluorescein 5 (6)-isothiocyanate, signal transducer and activator of transcription (STAT) phosphorylation, and real-time PCR of IFN-stimulated genes were assessed in the murine fibroblast cell line L929. In vivo experiments were performed to characterize the effect of simvastatin on the MVA-induced innate immune response and on the antitumor effect of MVA-based antitumor vaccines in B16 melanoma expressing ovalbumin (OVA) and Lewis lung carcinoma (LLC)-OVA tumor models. RNAseq analysis, depleting monoclonal antibodies, and flow cytometry were used to evaluate the MVA-mediated immune response. In this work, we identified commonly prescribed statins as potent IFNα pharmacological inhibitors due to their ability to reduce surface expression levels of IFN-α/β receptor 1 and to reduce clathrin-mediated endocytosis. Simvastatin and atorvastatin efficiently abrogated for 8 hours the transcriptomic response to IFNα and enhanced the number of dendritic cells presenting an OVA-derived peptide bound to major histocompatibility complex (MHC) class I. In vivo, intraperitoneal or intramuscular administration of simvastatin reduced the inflammatory response mediated by peritumoral administration of MVA and enhanced the antitumor activity of MVA encoding tumor-associated antigens. The synergistic antitumor effects critically depend on CD8+ cells, whereas they were markedly improved by depletion of CD4+ lymphocytes, T regulatory cells, or NK cells. Either MVA-OVA alone or combined with simvastatin augmented B cells, CD4+ lymphocytes, CD8+ lymphocytes, and tumor-specific CD8+ in the tumor-draining lymph nodes. However, only the treatment combination increased the numbers of these lymphocyte populations in the tumor microenvironment and in the spleen. In conclusion, blockade of IFNα functions by simvastatin markedly enhances lymphocyte infiltration and the antitumor activity of MVA, prompting a feasible drug repurposing. © Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- In Vitro,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Lactate dehydrogenase A-dependent aerobic glycolysis promotes natural killer cell anti-viral and anti-tumor function.
In Cell Reports on 1 June 2021 by Sheppard, S., Santosa, E. K., et al.
PubMed
Natural killer (NK) cells are cytotoxic lymphocytes capable of rapid cytotoxicity, cytokine secretion, and clonal expansion. To sustain such energetically demanding processes, NK cells must increase their metabolic capacity upon activation. However, little is known about the metabolic requirements specific to NK cells in vivo. To gain greater insight, we investigated the role of aerobic glycolysis in NK cell function and demonstrate that their glycolytic rate increases rapidly following viral infection and inflammation, prior to that of CD8+ T cells. NK cell-specific deletion of lactate dehydrogenase A (LDHA) reveals that activated NK cells rely on this enzyme for both effector function and clonal proliferation, with the latter being shared with T cells. As a result, LDHA-deficient NK cells are defective in their anti-viral and anti-tumor protection. These findings suggest that aerobic glycolysis is a hallmark of NK cell activation that is key to their function. Copyright © 2021 The Author(s). Published by Elsevier Inc. All rights reserved.
- Immunology and Microbiology
Follicular helper-T cells restore CD8+-dependent antitumor immunity and anti-PD-L1/PD-1 efficacy.
In Journal for Immunotherapy of Cancer on 1 June 2021 by Niogret, J., Berger, H., et al.
PubMed
T follicular helper cells (Tfh) are essential to shape B cell response during germinal center formation. Tfh accumulation has been reported in various human cancers, with positive or negative prognostic roles. However, the mechanisms explaining the accumulation of Tfh and their role in cancer remain obscure. In vitro differentiated and mouse cell sorted Tfh phenotype was evaluated by flow cytometry and quantitative PCR (qPCR). Antitumor effect of Tfh was evaluated by adoptive transfer in different tumor-bearing mice models. The involvement of immune cells, cytokines and chemokines was evaluated, using depleting antibodies. Chemokines and cytokines expression and production were evaluated by qPCR and ELISA. In human, the impact of immune cells and chemokines on survival was evaluated by analyzing transcriptomic data from public databases and from our own patient cohorts. In this study, we show that Tfh exert an antitumor immune effect in a CD8+-dependent manner. Tfh produce interleukin-21, which sustains proliferation, viability, cytokine production and cytotoxic functions of exhausted T cells. The presence of Tfh is required for efficacy of antiprogrammed cell death ligand-1 therapy. Tfh accumulate in the tumor bed and draining lymph nodes in different mouse cancer models. This recruitment is due to the capacity of transforming growth factor β to drive Chemokine (C-X-C motif) Ligand 13 expression, a chemoattractant of Tfh, by intratumor CD8+ T cells. Accumulation of Tfh and exhausted CD8+ T cells predicts cancer outcome in various cancer types. In patients treated with anti-programmed cell death-1 mAb, accumulation of Tfh and CD8+ at the tumor site is associated with outcome. This study provides evidence that CD8+/Tfh crosstalk is important in shaping antitumor immune response generated by immunotherapy. © Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
- FC/FACS,
- Mus musculus (House mouse)
Divergent Role for STAT5 in the Adaptive Responses of Natural Killer Cells.
In Cell Reports on 15 December 2020 by Wiedemann, G. M., Grassmann, S., et al.
PubMed
Natural killer (NK) cells are innate lymphocytes with the capacity to elicit adaptive features, including clonal expansion and immunological memory. Because signal transducer and activator of transcription 5 (STAT5) is essential for NK cell development, the roles of this transcription factor and its upstream cytokines interleukin-2 (IL-2) and IL-15 during infection have not been carefully investigated. In this study, we investigate how STAT5 regulates transcription during viral infection. We demonstrate that STAT5 is induced in NK cells by IL-12 and STAT4 early after infection and that partial STAT5 deficiency results in a defective capacity of NK cells to generate long-lived memory cells. Furthermore, we find a functional dichotomy of IL-2 and IL-15 signaling outputs during viral infection, whereby both cytokines drive clonal expansion, but only IL-15 is required for memory NK cell survival. We thus highlight a role for STAT5 signaling in promoting an optimal anti-viral NK cell response. Copyright © 2020 The Author(s). Published by Elsevier Inc. All rights reserved.
- In Vivo,
- FC/FACS,
- Mus musculus (House mouse),
- Immunology and Microbiology
Coordinated Viral Control by Cytotoxic Lymphocytes Ensures Optimal Adaptive NK Cell Responses.
In Cell Reports on 22 September 2020 by Diaz-Salazar, C. & Sun, J. C.
PubMed
Natural killer (NK) cells play a critical role in controlling viral infections, coordinating the response of innate and adaptive immune systems. They also possess certain features of adaptive lymphocytes, such as undergoing clonal proliferation. However, it is not known whether this adaptive NK cell response can be modulated by other lymphocytes during viral exposure. Here, we show that the clonal expansion of NK cells during mouse cytomegalovirus infection is severely blunted in the absence of cytotoxic CD8+ T cells. This correlates with higher viral burden and an increased pro-inflammatory milieu, which maintains NK cells in a hyper-activated state. Antiviral therapy rescues NK cell expansion in the absence of CD8+ T cells, suggesting that high viral loads have detrimental effects on adaptive NK cell responses. Altogether, our data support a mechanism whereby cytotoxic innate and adaptive lymphocytes cooperate to ensure viral clearance and the establishment of robust clonal NK cell responses. Copyright © 2020 The Author(s). Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology
B-Cell-Targeted 3DNA Nanotherapy Against Indoleamine 2,3-Dioxygenase 2 (IDO2) Ameliorates Autoimmune Arthritis in a Preclinical Model.
In Clinical Pathology (Thousand Oaks, Ventura County, Calif.) on 15 September 2020 by Merlo, L. M., Bowers, J., et al.
PubMed
The tryptophan catabolizing enzyme indoleamine 2,3-dioxygenase 2 (IDO2) has been identified as an immunomodulatory agent promoting autoimmunity in preclinical models. As such, finding ways to target the expression of IDO2 in B cells promises a new avenue for therapy for debilitating autoimmune disorders such as rheumatoid arthritis. IDO2, like many drivers of disease, is an intracellular protein expressed in a range of cells, and thus therapeutic inhibition of IDO2 requires a mechanism for targeting this intracellular protein in specific cell types. DNA nanostructures are a promising novel way of delivering small molecule drugs, antibodies, or siRNAs to the cytoplasm of a cell. These soluble, branched structures can carry cell-specific targeting moieties along with their therapeutic deliverable. Here, we examined a 3DNA nanocarrier specifically targeted to B cells with an anti-CD19 antibody. We find that this 3DNA is successfully delivered to and internalized in B cells. To test whether these nanostructures can deliver an efficacious therapeutic dose to alter autoimmune responses, a modified anti-IDO2 siRNA was attached to B-cell-directed 3DNA nanocarriers and tested in an established preclinical model of autoimmune arthritis, KRN.g7. The anti-IDO2 3DNA formulation ameliorates arthritis in this system, delaying the onset of joint swelling and reducing total arthritis severity. As such, a 3DNA nanocarrier system shows promise for delivery of targeted, specific, low-dose therapy for autoimmune disease. © The Author(s) 2020.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology,
- Neuroscience
In situ Vaccine Plus Checkpoint Blockade Induces Memory Humoral Response.
In Frontiers in Immunology on 28 August 2020 by Baniel, C. C., Heinze, C. M., et al.
PubMed
In a syngeneic murine melanoma (MEL) model, we recently reported an in situ vaccination response to combined radiation (RT) and intra-tumoral (IT) injection of anti-GD2 hu14. 18-IL2 immunocytokine (IC). This combined treatment resulted in 71% complete and durable regression of 5-week tumors, a tumor-specific memory T cell response, and augmented response to systemic anti-CTLA-4 antibody checkpoint blockade. While the ability of radiation to diversify anti-tumor T cell response has been reported, we hypothesize that mice rendered disease-free (DF) by a RT-based ISV might also exhibit a heightened B cell response. C57BL/6 mice were engrafted with 2 × 106 GD2+ B78 MEL and treated at a target tumor size of ~200 mm3 with 12 Gy RT, IT-IC on day (D)6-D10, and anti-CTLA-4 on D3, 6, and 9. Serum was collected via facial vein before tumor injection, before treatment, during treatment, after becoming DF, and following rejection of subcutaneous 2 × 106 B78 MEL re-challenge on D90. Flow cytometry demonstrated the presence of tumor-specific IgG in sera from mice rendered DF and rejecting re-challenge with B78 MEL at D90 after starting treatment. Consistent with an adaptive endogenous anti-tumor humoral memory response, these anti-tumor antibodies bound to B78 cells and parental B16 cells (GD2-), but not to the unrelated syngeneic Panc02 or Panc02 GD2+ cell lines. We evaluated the kinetics of this response and observed that tumor-specific IgG was consistently detected by D22 after initiation of treatment, corresponding to a time of rapid tumor regression. The amount of tumor-specific antibody binding to tumor cells (as measured by flow MFI) did not correlate with host animal prognosis. Incubation of B16 MEL cells in DF serum, vs. naïve serum, prior to IV injection, did not delay engraftment of B16 metastases and showed similar overall survival rates. B cell depletion using anti-CD20 or anti-CD19 and anti-B220 did not impact the efficacy of ISV treatment. Thus, treatment with RT + IC + anti-CTLA-4 results in adaptive anti-tumor humoral memory response. This endogenous tumor-specific antibody response does not appear to have therapeutic efficacy but may serve as a biomarker for an anti-tumor T cell response. Copyright © 2020 Baniel, Heinze, Hoefges, Sumiec, Hank, Carlson, Jin, Patel, Sriramaneni, Gillies, Erbe, Schwarz, Pieper, Rakhmilevich, Sondel and Morris.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Complement Signals Determine Opposite Effects of B Cells in Chemotherapy-Induced Immunity.
In Cell on 19 March 2020 by Lu, Y., Zhao, Q., et al.
PubMed
Understanding molecular mechanisms that dictate B cell diversity is important for targeting B cells as anti-cancer treatment. Through the single-cell dissection of B cell heterogeneity in longitudinal samples of patients with breast cancer before and after neoadjuvant chemotherapy, we revealed that an ICOSL+ B cell subset emerges after chemotherapy. Using three immunocompetent mouse models, we recapitulated the subset switch of human tumor-infiltrating B cells during chemotherapy. By employing B-cell-specific deletion mice, we showed that ICOSL in B cells boosts anti-tumor immunity by enhancing the effector to regulatory T cell ratio. The signature of ICOSL+ B cells is imprinted by complement-CR2 signaling, which is triggered by immunogenic cell death. Moreover, we identified that CD55, a complement inhibitory protein, determines the opposite roles of B cells in chemotherapy. Collectively, we demonstrated a critical role of the B cell subset switch in chemotherapy response, which has implications in designing novel anti-cancer therapies. VIDEO ABSTRACT.Copyright © 2020 Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
Dendritic Cell Paucity Leads to Dysfunctional Immune Surveillance in Pancreatic Cancer.
In Cancer Cell on 16 March 2020 by Hegde, S., Krisnawan, V. E., et al.
PubMed
Here, we utilized spontaneous models of pancreatic and lung cancer to examine how neoantigenicity shapes tumor immunity and progression. As expected, neoantigen expression during lung adenocarcinoma development leads to T cell-mediated immunity and disease restraint. By contrast, neoantigen expression in pancreatic ductal adenocarcinoma (PDAC) results in exacerbation of a fibro-inflammatory microenvironment that drives disease progression and metastasis. Pathogenic TH17 responses are responsible for this neoantigen-induced tumor progression in PDAC. Underlying these divergent T cell responses in pancreas and lung cancer are differences in infiltrating conventional dendritic cells (cDCs). Overcoming cDC deficiency in early-stage PDAC leads to disease restraint, while restoration of cDC function in advanced PDAC restores tumor-restraining immunity and enhances responsiveness to radiation therapy. Copyright © 2020 Elsevier Inc. All rights reserved.
- Immunology and Microbiology
Toxoplasma gondii tkl1 Deletion Mutant Is a Promising Vaccine against Acute, Chronic, and Congenital Toxoplasmosis in Mice.
In The Journal of Immunology on 15 March 2020 by Wang, J. L., Liang, Q. L., et al.
PubMed
In this study, we generated a tkl1 deletion mutant in the Toxoplasma gondii type 1 RH (RHΔtkl1) strain and tested the protective efficacies of vaccination using RHΔtkl1 tachyzoites against acute, chronic, and congenital T. gondii infections in Kunming mice. Mice vaccinated with RHΔtkl1 mounted a strong humoral and cellular response as shown by elevated levels of anti-T. gondii-specific IgG, IL-2, IL-12, IFN-γ, and IL-10. All RHΔtkl1-vaccinated mice survived a lethal challenge with 1 × 103 tachyzoites of type 1 RH or ToxoDB#9 (PYS or TgC7) strain as well as 100 cysts or oocysts of Prugniuad strain. All mock-vaccinated plus infected mice have died. Vaccination also protected against cyst- or oocyst-caused chronic infection, reduced vertical transmission caused by oocysts, increased litter size, and maintained body weight of pups born to dams challenged with 10 oocysts on day 5 of gestation. In contrast, all mock-vaccinated plus oocysts-infected dams had aborted, and no fetus has survived. Vaccinated dams remained healthy postinfection, and their brain cyst burden was significantly reduced compared with mock-vaccinated dams infected with oocysts. In vivo depletion of CD4+ T cells, CD8+ T cells, and B cells revealed that CD8+ T cells are involved in the protection of mice against T. gondii infection. Additionally, adoptive transfer of CD8+ T cells from RHΔtkl1-vaccinated mice significantly enhanced the survival of naive mice infected with the pathogenic strain. Together, these data reaffirm the importance of CD8+ T cell responses in future vaccine design for toxoplasmosis and present T. gondii tkl1 gene as a promising vaccine candidate. Copyright © 2020 by The American Association of Immunologists, Inc.
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Immunotherapy with Monoclonal Antibodies in Lung Cancer of Mice: Oxidative Stress and Other Biological Events.
In Cancers on 4 September 2019 by Tang, J., Ramis-Cabrer, D., et al.
PubMed
Background: Lung cancer (LC) is a major leading cause of death worldwide. Immunomodulators that target several immune mechanisms have proven to reduce tumor burden in experimental models through induction of the immune microenvironment. We hypothesized that other biological mechanisms may also favor tumor burden reduction in lung cancer-bearing mice treated with immunomodulators. Methods: Tumor weight, area, T cells and tumor growth (immunohistochemistry), oxidative stress, apoptosis, autophagy, and signaling (NF-κB and sirtuin-1) markers were analyzed (immunoblotting) in subcutaneous tumor of BALB/c mice injected with LP07 adenocarcinoma cells treated with monoclonal antibodies (CD-137, CTLA-4, PD-1, and CD-19, N = 9/group) and non-treated control animals. Results: Compared to non-treated cancer mice, in tumors of monoclonal-treated animals, tumor area and weight and ki-67 were significantly reduced, while T cell counts, oxidative stress, apoptosis, autophagy, activated p65, and sirtuin-1 markers were increased. Conclusions: Immunomodulators elicited a reduction in tumor burden (reduced tumor size and weight) through decreased tumor proliferation and increased oxidative stress, apoptosis, autophagy, and signaling markers, which may have interfered with the immune profile of the tumor microenvironment. Future research should be devoted to the elucidation of the specific contribution of each biological mechanism to the reduced tumor burden.
- Immunology and Microbiology
TLR9 signaling in fibroblastic reticular cells regulates peritoneal immunity.
In The Journal of Clinical Investigation on 5 August 2019 by Xu, L., Li, Y., et al.
PubMed
Fibroblastic reticular cells (FRCs), a subpopulation of stromal cells in lymphoid organs and fat-associated lymphoid clusters (FALCs) in adipose tissue, play immune-regulatory roles in the host response to infection and may be useful as a form of cell therapy in sepsis. Here, we found an unexpected major role of TLR9 in controlling peritoneal immune cell recruitment and FALC formation at baseline and after sepsis induced by cecal ligation and puncture (CLP). TLR9 regulated peritoneal immunity via suppression of chemokine production by FRCs. Adoptive transfer of TLR9-deficient FRCs more effectively decreased mortality, bacterial load, and systemic inflammation after CLP than WT FRCs. Importantly, we found that activation of TLR9 signaling suppressed chemokine production by human adipose tissue-derived FRCs. Together, our results indicate that TLR9 plays critical roles in regulating peritoneal immunity via suppression of chemokine production by FRCs. These data form a knowledge basis upon which to design new therapeutic strategies to improve the therapeutic efficacy of FRC-based treatments for sepsis and immune dysregulation diseases.