InVivoMAb anti-mouse IL-12 p40
Product Details
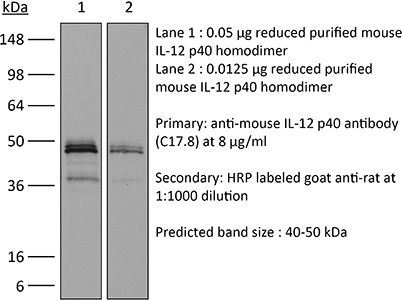
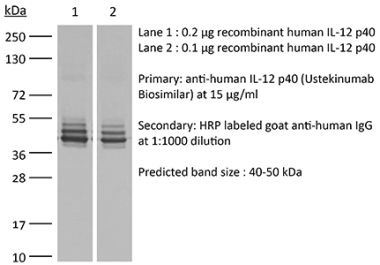
The C17.8 antibody reacts with mouse p40 also known as IL-12β. p40 is a 40 kDa subunit of IL-12 and IL-23. IL-12 is a heterodimeric cytokine composed of subunits IL-12α p35 and IL-12β p40. The p40 subunit of IL-12 also combines with p19, a protein that shows no biological activity by itself, to form IL-23. IL-12 is secreted by activated monocytes, macrophages, and dendritic cells while IL-23 is secreted by activated dendritic cells and epithelial cells. IL-12 plays roles in T lymphocyte differentiation, IFNγ production, and NK cell cytotoxicity. The C17.8 antibody has been shown to neutralize both IL-12 and IL-23 bioactivity.Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse IL-12 p70 |
| Reported Applications |
in vivo IL-12p40 neutralization p40 affinity chromatography Immunoprecipitation ELISA Flow cytometry Western blot |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107698 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo IL-12 neutralization
Dann, S. M., et al. (2018). "Giardia Infection of the Small Intestine Induces Chronic Colitis in Genetically Susceptible Hosts" J Immunol 201(2): 548-559. PubMed
Chemokines are small chemotactic proteins that have a crucial role in leukocyte recruitment into tissue. Targeting these mediators has been suggested as a potential therapeutic option in inflammatory skin diseases such as psoriasis. Using quantitative RT-PCR, we found CCL7, a chemokine ligand known to interact with multiple C-C chemokine receptors, to be markedly increased in lesional psoriasis as opposed to atopic dermatitis, lichen planus, non-lesional psoriatic and normal control skin. Surprisingly, this increase in CCL7 mRNA expression exceeded that of all other chemokines investigated, and keratinocytes and dermal blood endothelial cells were identified as its likely cellular sources. In an imiquimod-induced psoriasis-like mouse model, CCL7 had a profound impact on myeloid cell inflammation as well as on the upregulation of key pro-psoriatic cytokines such as CCL20, IL-12p40 and IL-17C, while its blockade led to an increase in the antipsoriatic cytokine IL-4. In humans receiving the TNF-alpha-blocker infliximab, CCL7 was downregulated in lesional psoriatic skin already within 16 hours after a single intravenous infusion. These data suggest that CCL7 acts as a driver of TNF-alpha-dependent Th1/Th17-mediated inflammation in lesional psoriatic skin.
in vivo IL-12 neutralization, Flow Cytometry
Deligne, C., et al. (2015). "Anti-CD20 therapy induces a memory Th1 response through the IFN-gamma/IL-12 axis and prevents protumor regulatory T-cell expansion in mice" Leukemia 29(4): 947-957. PubMed
The long-lasting clinical response by lymphoma patients to anti-CD20 therapy has been attributed to the induction of an anti-tumor adaptive immunity. We previously demonstrated that a CD4-dependent mechanism is responsible for the long-term protection of CD20(+) tumor-bearing mice by anti-CD20 treatment. Here, we compare tumor immunity in tumor-bearing animals that did or did not receive anti-CD20 treatment. Splenic CD4(+)FoxP3(+) regulatory T cells (Tregs) expanded substantially in untreated mice that exhibited then a reduced survival, whereas Tregs depletion led to long-term survival of the animals, suggesting the establishment of a Treg-dependent immunosuppressive environment after tumor injection. Strikingly, anti-CD20 therapy reversed the initial expansion of Tregs, and was accompanied by a marked increase in the number of Th1 cells, with no detectable change in Th2 and Th17 cell numbers. Interleukin-12 serum level was also increased by the anti-CD20 treatment, and activated myeloid dendritic cells producing interleukin-12 could be detected in lymph nodes of treated animals, while interferon-gamma blockade strongly reduced survival. Also, CD4(+) effector memory T cells were evidenced in surviving animals, and the transfer of CD4(+) T cells induced long-term protection. Thus, anti-CD20 therapy promotes strong anti-tumor adaptive immunity, opposes Treg expansion and inhibits tumor cells from maintaining an immunosuppressive environment.
in vivo IL-12 neutralization
Brunner, P. M., et al. (2015). "CCL7 contributes to the TNF-alpha-dependent inflammation of lesional psoriatic skin" Exp Dermatol 24(7): 522-528. PubMed
Chemokines are small chemotactic proteins that have a crucial role in leukocyte recruitment into tissue. Targeting these mediators has been suggested as a potential therapeutic option in inflammatory skin diseases such as psoriasis. Using quantitative RT-PCR, we found CCL7, a chemokine ligand known to interact with multiple C-C chemokine receptors, to be markedly increased in lesional psoriasis as opposed to atopic dermatitis, lichen planus, non-lesional psoriatic and normal control skin. Surprisingly, this increase in CCL7 mRNA expression exceeded that of all other chemokines investigated, and keratinocytes and dermal blood endothelial cells were identified as its likely cellular sources. In an imiquimod-induced psoriasis-like mouse model, CCL7 had a profound impact on myeloid cell inflammation as well as on the upregulation of key pro-psoriatic cytokines such as CCL20, IL-12p40 and IL-17C, while its blockade led to an increase in the antipsoriatic cytokine IL-4. In humans receiving the TNF-alpha-blocker infliximab, CCL7 was downregulated in lesional psoriatic skin already within 16 hours after a single intravenous infusion. These data suggest that CCL7 acts as a driver of TNF-alpha-dependent Th1/Th17-mediated inflammation in lesional psoriatic skin.
in vivo IL-12 neutralization
Villegas-Mendez, A., et al. (2015). "Parasite-specific CD4+IFN-gamma+IL-10+ T cells distribute within both lymphoid and non-lymphoid compartments and are controlled systemically by IL-27 and ICOS during blood-stage malaria infection" Infect Immun. pii : IAI.01100-15. PubMed
Immune-mediated pathology in IL-10 deficient mice during blood-stage malaria infection typically manifests in non-lymphoid organs, such as the liver and lung. Thus, it is critical to define the cellular sources of IL-10 in these sensitive non-lymphoid compartments during infection. Moreover, it is important to determine if IL-10 production is controlled through conserved or disparate molecular programmes in distinct anatomical locations during malaria infection, as this may enable spatiotemporal tuning of the regulatory immune response. In this study, using dual IFN-gamma-YFP and IL-10-GFP reporter mice we show that CD4+YFP+ T cells are the major source of IL-10 in both lymphoid and non-lymphoid compartments throughout the course of blood-stage P. yoelii infection. Mature splenic CD4+YFP+GFP+ T cells, which preferentially expressed high levels of CCR5, were capable of migrating to and seeding the non-lymphoid tissues, indicating that the systemically distributed host-protective cells have a common developmental history. Despite exhibiting comparable phenotypes, CD4+YFP+GFP+ T cells from the liver and lung produced significantly higher quantities of IL-10 than their splenic counterparts, showing that the CD4+YFP+GFP+ T cells exert graded functions in distinct tissue locations during infection. Unexpectedly, given the unique environmental conditions within discrete non-lymphoid and lymphoid organs, we show that IL-10 production by CD4+YFP+ T cells is controlled systemically during malaria infection through IL-27R signalling that is supported post-CD4+ T cell priming by ICOS signalling. The results in this study substantially improve our understanding of the systemic IL-10 response to malaria infection, particularly within sensitive non-lymphoid organs.
Immunoprecipitation, p40 affinity chromatography
Abdi, K., et al. (2014). "Free IL-12p40 monomer is a polyfunctional adaptor for generating novel IL-12-like heterodimers extracellularly" J Immunol 192(12): 6028-6036. PubMed
IL-12p40 partners with the p35 and p19 polypeptides to generate the heterodimeric cytokines IL-12 and IL-23, respectively. These cytokines play critical and distinct roles in host defense. The assembly of these heterodimers is thought to take place within the cell, resulting in the secretion of fully functional cytokines. Although the p40 subunit alone can also be rapidly secreted in response to inflammatory signals, its biological significance remains unclear. In this article, we show that the secreted p40 monomer can generate de novo IL-12-like activities by combining extracellularly with p35 released from other cells. Surprisingly, an unbiased proteomic analysis reveals multiple such extracellular binding partners for p40 in the serum of mice after an endotoxin challenge. We biochemically validate the binding of one of these novel partners, the CD5 Ag-like glycoprotein, to the p40 monomer. Nevertheless, the assembled p40-CD5L heterodimer does not recapitulate the biological activity of IL-12. These findings underscore the plasticity of secreted free p40 monomer, suggesting that p40 functions as an adaptor that is able to generate multiple de novo composites in combination with other locally available polypeptide partners after secretion.
in vivo IL-12p40 neutralization
Ruffell, B., et al. (2014). "Macrophage IL-10 blocks CD8+ T cell-dependent responses to chemotherapy by suppressing IL-12 expression in intratumoral dendritic cells" Cancer Cell 26(5): 623-637. PubMed
Blockade of colony-stimulating factor-1 (CSF-1) limits macrophage infiltration and improves response of mammary carcinomas to chemotherapy. Herein we identify interleukin (IL)-10 expression by macrophages as the critical mediator of this phenotype. Infiltrating macrophages were the primary source of IL-10 within tumors, and therapeutic blockade of IL-10 receptor (IL-10R) was equivalent to CSF-1 neutralization in enhancing primary tumor response to paclitaxel and carboplatin. Improved response to chemotherapy was CD8(+) T cell-dependent, but IL-10 did not directly suppress CD8(+) T cells or alter macrophage polarization. Instead, IL-10R blockade increased intratumoral dendritic cell expression of IL-12, which was necessary for improved outcomes. In human breast cancer, expression of IL12A and cytotoxic effector molecules were predictive of pathological complete response rates to paclitaxel.
in vivo IL-12p40 neutralization
Tarrio, M. L., et al. (2014). "Proliferation conditions promote intrinsic changes in NK cells for an IL-10 response" J Immunol 193(1): 354-363. PubMed
Constitutively found at high frequencies, the role for NK cell proliferation remains unclear. In this study, a shift in NK cell function from predominantly producing IFN-gamma, a cytokine with proinflammatory and antimicrobial functions, to producing the immunoregulatory cytokine IL-10 was defined during extended murine CMV infection. The response occurred at times subsequent to IL-12 production, but the NK cells elicited acquired responsiveness to IL-12 and IL-21 for IL-10 production. Because neither IL-12 nor IL-21 was required in vivo, however, additional pathways appeared to be available to promote NK cell IL-10 expression. In vitro studies with IL-2 to support proliferation and in vivo adoptive transfers into murine CMV-infected mice demonstrated that NK cell proliferation and further division enhanced the change. In contrast to the sustained open profile of the IFN-gamma gene, NK cells responding to infection acquired histone modifications in the IL-10 gene indicative of changing from a closed to an open state. The IL-10 response to IL-12 was proliferation dependent ex vivo if the NK cells had not yet expanded in vivo but independent if they had. Thus, a novel role for proliferation in supporting changing innate cell function is reported.
in vivo IL-12p40 neutralization
Tang, W., et al. (2014). "The oncoprotein and transcriptional regulator Bcl-3 governs plasticity and pathogenicity of autoimmune T cells" Immunity 41(4): 555-566. PubMed
Bcl-3 is an atypical member of the IkappaB family that modulates transcription in the nucleus via association with p50 (NF-kappaB1) or p52 (NF-kappaB2) homodimers. Despite evidence attesting to the overall physiologic importance of Bcl-3, little is known about its cell-specific functions or mechanisms. Here we demonstrate a T-cell-intrinsic function of Bcl-3 in autoimmunity. Bcl-3-deficient T cells failed to induce disease in T cell transfer-induced colitis and experimental autoimmune encephalomyelitis. The protection against disease correlated with a decrease in Th1 cells that produced the cytokines IFN-gamma and GM-CSF and an increase in Th17 cells. Although differentiation into Th1 cells was not impaired in the absence of Bcl-3, differentiated Th1 cells converted to less-pathogenic Th17-like cells, in part via mechanisms involving expression of the RORgammat transcription factor. Thus, Bcl-3 constrained Th1 cell plasticity and promoted pathogenicity by blocking conversion to Th17-like cells, revealing a unique type of regulation that shapes adaptive immunity.
in vivo IL-12p40 neutralization
Yu, X., et al. (2013). "A multifunctional chimeric chaperone serves as a novel immune modulator inducing therapeutic antitumor immunity" Cancer Res 73(7): 2093-2103. PubMed
Converting the immunosuppressive tumor environment into one that is favorable to the induction of antitumor immunity is indispensable for effective cancer immunotherapy. Here, we strategically incorporate a pathogen (i.e., flagellin)-derived, NF-kappaB-stimulating “danger” signal into the large stress protein or chaperone Grp170 (HYOU1/ORP150) that was previously shown to facilitate antigen crosspresentation. This engineered chimeric molecule (i.e., Flagrp170) is capable of transporting tumor antigens and concurrently inducing functional activation of dendritic cells (DC). Intratumoral administration of adenoviruses expressing Flagrp170 induces a superior antitumor response against B16 melanoma and its distant lung metastasis compared with unmodified Grp170 and flagellin. The enhanced tumor destruction is accompanied with significantly increased tumor infiltration by CD8(+) cells as well as elevation of IFN-gamma and interleukin (IL)-12 levels in the tumor sites. In situ Ad.Flagrp170 therapy provokes systemic activation of CTLs that recognize several antigens naturally expressing in melanoma (e.g., gp100/PMEL and TRP2/DCT). The mechanistic studies using CD11c-DTR transgenic mice and Batf3-deficient mice reveal that CD8alpha(+) DCs are required for the improved T-cell crosspriming. Antibody neutralization assays show that IL-12 and IFN-gamma are essential for the Flagrp170-elicited antitumor response, which also involves CD8(+) T cells and natural killer cells. The therapeutic efficacy of Flagrp170 and its immunostimulating activity are also confirmed in mouse prostate cancer and colon carcinoma. Together, targeting the tumor microenvironment with this chimeric chaperone is highly effective in mobilizing or restoring antitumor immunity, supporting the potential therapeutic use of this novel immunomodulator in the treatment of metastatic diseases.
in vivo IL-12p40 neutralization
Gwyer Findlay, E., et al. (2013). "IL-27 receptor signaling regulates CD4+ T cell chemotactic responses during infection" J Immunol 190(9): 4553-4561. PubMed
IL-27 exerts pleiotropic suppressive effects on naive and effector T cell populations during infection and inflammation. Surprisingly, however, the role of IL-27 in restricting or shaping effector CD4(+) T cell chemotactic responses, as a mechanism to reduce T cell-dependent tissue inflammation, is unknown. In this study, using Plasmodium berghei NK65 as a model of a systemic, proinflammatory infection, we demonstrate that IL-27R signaling represses chemotaxis of infection-derived splenic CD4(+) T cells in response to the CCR5 ligands, CCL4 and CCL5. Consistent with these observations, CCR5 was expressed on significantly higher frequencies of splenic CD4(+) T cells from malaria-infected, IL-27R-deficient (WSX-1(-/-)) mice than from infected wild-type mice. We find that IL-27 signaling suppresses splenic CD4(+) T cell CCR5-dependent chemotactic responses during infection by restricting CCR5 expression on CD4(+) T cell subtypes, including Th1 cells, and also by controlling the overall composition of the CD4(+) T cell compartment. Diminution of the Th1 response in infected WSX-1(-/-) mice in vivo by neutralization of IL-12p40 attenuated CCR5 expression by infection-derived CD4(+) T cells and also reduced splenic CD4(+) T cell chemotaxis toward CCL4 and CCL5. These data reveal a previously unappreciated role for IL-27 in modulating CD4(+) T cell chemotactic pathways during infection, which is related to its capacity to repress Th1 effector cell development. Thus, IL-27 appears to be a key cytokine that limits the CCR5-CCL4/CCL5 axis during inflammatory settings.
in vivo IL-12p40 neutralization
Villegas-Mendez, A., et al. (2013). "IL-27 receptor signalling restricts the formation of pathogenic, terminally differentiated Th1 cells during malaria infection by repressing IL-12 dependent signals" PLoS Pathog 9(4): e1003293. PubMed
The IL-27R, WSX-1, is required to limit IFN-gamma production by effector CD4(+) T cells in a number of different inflammatory conditions but the molecular basis of WSX-1-mediated regulation of Th1 responses in vivo during infection has not been investigated in detail. In this study we demonstrate that WSX-1 signalling suppresses the development of pathogenic, terminally differentiated (KLRG-1(+)) Th1 cells during malaria infection and establishes a restrictive threshold to constrain the emergent Th1 response. Importantly, we show that WSX-1 regulates cell-intrinsic responsiveness to IL-12 and IL-2, but the fate of the effector CD4(+) T cell pool during malaria infection is controlled primarily through IL-12 dependent signals. Finally, we show that WSX-1 regulates Th1 cell terminal differentiation during malaria infection through IL-10 and Foxp3 independent mechanisms; the kinetics and magnitude of the Th1 response, and the degree of Th1 cell terminal differentiation, were comparable in WT, IL-10R1(-)/(-) and IL-10(-)/(-) mice and the numbers and phenotype of Foxp3(+) cells were largely unaltered in WSX-1(-)/(-) mice during infection. As expected, depletion of Foxp3(+) cells did not enhance Th1 cell polarisation or terminal differentiation during malaria infection. Our results significantly expand our understanding of how IL-27 regulates Th1 responses in vivo during inflammatory conditions and establishes WSX-1 as a critical and non-redundant regulator of the emergent Th1 effector response during malaria infection.
in vivo IL-12p40 neutralization
Chappert, P., et al. (2013). "Specific gut commensal flora locally alters T cell tuning to endogenous ligands" Immunity 38(6): 1198-1210. PubMed
Differences in gut commensal flora can dramatically influence autoimmune responses, but the mechanisms behind this are still unclear. We report, in a Th1-cell-driven murine model of autoimmune arthritis, that specific gut commensals, such as segmented filamentous bacteria, have the ability to modulate the activation threshold of self-reactive T cells. In the local microenvironment of gut-associated lymphoid tissues, inflammatory cytokines elicited by the commensal flora dynamically enhanced the antigen responsiveness of T cells that were otherwise tuned down to a systemic self-antigen. Together with subtle differences in early lineage differentiation, this ultimately led to an enhanced recruitment of pathogenic Th1 cells and the development of a more severe form of autoimmune arthritis. These findings define a key role for the gut commensal flora in sustaining ongoing autoimmune responses through the local fine tuning of T-cell-receptor-proximal activation events in autoreactive T cells.
in vivo IL-12p40 neutralization
Prabhakara, R., et al. (2011). "Suppression of the inflammatory immune response prevents the development of chronic biofilm infection due to methicillin-resistant Staphylococcus aureus" Infect Immun 79(12): 5010-5018. PubMed
Staphylococcus aureus is a common cause of prosthetic implant infections, which can become chronic due to the ability of S. aureus to grow as a biofilm. Little is known about adaptive immune responses to these infections in vivo. We hypothesized that S. aureus elicits inflammatory Th1/Th17 responses, associated with biofilm formation, instead of protective Th2/Treg responses. We used an adapted mouse model of biofilm-mediated prosthetic implant infection to determine chronic infection rates, Treg cell frequencies, and local cytokine levels in Th1-biased C57BL/6 and Th2-biased BALB/c mice. All C57BL/6 mice developed chronic S. aureus implant infection at all time points tested. However, over 75% of BALB/c mice spontaneously cleared the infection without adjunctive therapy and demonstrated higher levels of Th2 cytokines and anti-inflammatory Treg cells. When chronic infection rates in mice deficient in the Th2 cytokine interleukin-4 (IL-4) via STAT6 mutation in a BALB/c background were assessed, the mice were unable to clear the S. aureus implant infection. Additionally, BALB/c mice depleted of Treg cells via an anti-CD25 monoclonal antibody (MAb) were also unable to clear the infection. In contrast, the C57BL/6 mice that were susceptible to infection were able to eliminate S. aureus biofilm populations on infected intramedullary pins once the Th1 and Th17 responses were diminished by MAb treatment with anti-IL-12 p40. Together, these results indicate that Th2/Treg responses are mechanisms of protection against chronic S. aureus implant infection, as opposed to Th1/Th17 responses, which may play a role in the development of chronic infection.
in vivo IL-12p40 neutralization
Mack, E. A., et al. (2011). "Type 1 interferon induction of natural killer cell gamma interferon production for defense during lymphocytic choriomeningitis virus infection" MBio 2(4). PubMed
Natural killer (NK) cells are equipped to innately produce the cytokine gamma interferon (IFN-gamma) in part because they basally express high levels of the signal transducer and activator of transcription 4 (STAT4). Type 1 interferons (IFNs) have the potential to activate STAT4 and promote IFN-gamma expression, but concurrent induction of elevated STAT1 negatively regulates access to the pathway. As a consequence, it has been difficult to detect type 1 IFN stimulation of NK cell IFN-gamma during viral infections in the presence of STAT1 and to understand the evolutionary advantage for maintaining the pathway. The studies reported here evaluated NK cell responses following infections with lymphocytic choriomeningitis virus (LCMV) in the compartment handling the earliest events after infection, the peritoneal cavity. The production of type 1 IFNs, both IFN-alpha and IFN-beta, was shown to be early and of short duration, peaking at 30 h after challenge. NK cell IFN-gamma expression was detected with overlapping kinetics and required activating signals delivered through type 1 IFN receptors and STAT4. It took place under conditions of high STAT4 levels but preceded elevated STAT1 expression in NK cells. The IFN-gamma response reduced viral burdens. Interestingly, increases in STAT1 were delayed in NK cells compared to other peritoneal exudate cell (PEC) populations. Taken together, the studies demonstrate a novel mechanism for stimulating IFN-gamma production and elucidate a biological role for type 1 IFN access to STAT4 in NK cells.
in vivo IL-12p40 neutralization, ELISA
Massacand, J. C., et al. (2009). "Helminth products bypass the need for TSLP in Th2 immune responses by directly modulating dendritic cell function" Proc Natl Acad Sci U S A 106(33): 13968-13973. PubMed
Thymic stromal lymphopoietin (TSLP) is an interleukin (IL)-7-like cytokine, mainly expressed by epithelial cells, and key to the development of allergic responses. The well-documented involvement of TSLP in allergy has led to the conviction that TSLP promotes the development of inflammatory Th2 cell responses. However, we now report that the interaction of TSLP with its receptor (TSLPR) has no functional impact on the development of protective Th2 immune responses after infection with 2 helminth pathogens, Heligmosomoides polygyrus and Nippostrongylus brasiliensis. Mice deficient in the TSLP binding chain of the TSLPR (TSLPR(-/-)) exhibited normal Th2 cell differentiation, protective immunity and memory responses against these two distinct rodent helminths. In contrast TSLP was found to be necessary for the development of protective Th2 responses upon infection with the helminth Trichuris muris (T. muris). TSLP inhibited IL-12p40 production in response to T. muris infection, and treatment of TSLPR(-/-) animals with neutralizing anti-IL-12p40 monoclonal antibody (mAb) was able to reverse susceptibility and attenuate IFN-gamma production. We additionally demonstrated that excretory-secretory (ES) products from H. polygyrus and N. brasiliensis, but not T. muris, were capable of directly suppressing dendritic cell (DC) production of IL-12p40, thus bypassing the need for TSLP. Taken together, our data show that the primary function of TSLP is to directly suppress IL-12 secretion, thus supporting Th2 immune responses.
- Mus musculus (House mouse),
- Immunology and Microbiology
MEK inhibitors increase the mortality rate in mice with LPS-induced inflammation through IL-12-NO signaling.
In Cell Death Discovery on 13 October 2023 by Hashimoto, R., Koide, H., et al.
PubMed
Lipopolysaccharide (LPS) is an endotoxin that can cause an acute inflammatory response. Nitric oxide (NO) is one of the most important innate immune system components and is synthesized by inducible NOS (iNOS) in macrophages in response to stimulation with LPS. LPS activates the RAS-RAF-mitogen-activated protein kinase/ERK kinase (MEK)-extracellular-signal-regulated kinase (ERK) signaling cascade in macrophages. The purpose of this study was to examine how the combination of LPS and MEK inhibitors, which have been used as anticancer agents in recent years, affects inflammation. We showed that MEK inhibitors enhanced iNOS expression and NO production in LPS-stimulated mouse bone marrow-derived macrophages. A MEK inhibitor increased the mortality rate in mice with LPS-induced inflammation. The expression of the cytokine interleukin-12 (IL-12) in macrophages was enhanced by the MEK inhibitor, as shown by a cytokine array and ELISA. IL-12 enhanced iNOS expression and NO production in response to LPS. We also showed that tumor necrosis factor (TNF-α) was secreted by macrophage after stimulation with LPS and that TNF-α and IL-12 synergistically induced iNOS expression and NO production. An anti-IL-12 neutralizing antibody prevented NO production and mortality in an LPS-induced inflammation mouse model in the presence of a MEK inhibitor. These results suggest that the MEK inhibitor increases the mortality rate in mice with LPS-induced inflammation through IL-12-NO signaling. © 2023. Cell Death Differentiation Association (ADMC).
- WB,
- Mus musculus (House mouse),
- Cancer Research,
- Genetics
Intratumoral injection of IL-12-encoding mRNA targeted to CSFR1 and PD-L1 exerts potent anti-tumor effects without substantial systemic exposure.
In Molecular Therapy. Nucleic Acids on 12 September 2023 by Di Trani, C. A., Cirella, A., et al.
PubMed
IL-12 is a potent cytokine for cancer immunotherapy. However, its systemic delivery as a recombinant protein has shown unacceptable toxicity in the clinic. Currently, the intratumoral injection of IL-12-encoding mRNA or DNA to avoid such side effects is being evaluated in clinical trials. In this study, we aimed to improve this strategy by further favoring IL-12 tethering to the tumor. We generated in vitro transcribed mRNAs encoding murine single-chain IL-12 fused to diabodies binding to CSF1R and/or PD-L1. These targeted molecules are expressed in the tumor microenvironment, especially on myeloid cells. The binding capacity of chimeric constructs and the bioactivity of IL-12 were demonstrated in vitro and in vivo. Doses as low as 0.5 μg IL-12-encoding mRNA achieved potent antitumor effects in subcutaneously injected B16-OVA and MC38 tumors. Treatment delivery was associated with increases in IL-12p70 and IFN-γ levels in circulation. Fusion of IL-12 to the diabodies exerted comparable efficacy against bilateral tumor models. However, it achieved tethering to myeloid cells infiltrating the tumor, resulting in nearly undetectable systemic levels of IL-12 and IFN-γ. Overall, tethering IL-12 to intratumoral myeloid cells in the mRNA-transferred tumors achieves similar efficacy while reducing the dangerous systemic bioavailability of IL-12. © 2023 The Author(s).
- Mus musculus (House mouse)
pH Dependence of a GPR4 Selective Antagonist Hampers Its Therapeutic Potential.
In The Journal of Pharmacology and Experimental Therapeutics on 1 July 2023 by Stalewski, J., Shih, A. Y., et al.
PubMed
Inflammatory bowel disease (IBD) is characterized by chronic mucosal inflammation of the gastrointestinal tract and is associated with extracellular acidification of mucosal tissue. Several extracellular pH-sensing receptors, including G protein-coupled receptor 4 (GPR4), play an important role in the regulation of inflammatory and immune responses, and GPR4 deficiency has been shown to be protective in IBD animal models. To confirm the therapeutic potential of GPR4 antagonism in IBD, we tested Compound 13, a selective GPR4 antagonist, in the interleukin 10-/- mouse model of colitis. Despite good exposures and albeit there was a trend toward improvement for a few readouts, Compound 13 treatment did not improve colitis in this model, and there were no signs of target engagement. Interestingly, Compound 13 behaved as an "orthosteric" antagonist, i.e., its potency was pH dependent and mostly inactive at pH levels lower than 6.8 with preferential binding to the inactive conformation of GPR4. Mutagenesis studies confirmed Compound 13 likely binds to the conserved orthosteric binding site in G protein-coupled receptors, where a histidine sits in GPR4 likely preventing Compound 13 binding when protonated in acidic conditions. While the exact mucosal pH in the human disease and relevant IBD mice models is unknown, it is well established that the degree of acidosis is positively correlated with the degree of inflammation, suggesting Compound 13 is not an ideal tool to study the role of GPR4 in moderate to severe inflammatory conditions. SIGNIFICANCE STATEMENT: Compound 13, a reported selective GPR4 antagonist, has been widely used to assess the therapeutic potential of GPR4, a pH-sensing receptor, for numerous indications. Its pH dependence and mechanism of inhibition identified in this study clearly highlights the limitations of this chemotype for target validation. Copyright © 2023 by The Author(s).
- Mus musculus (House mouse)
Sterile liver injury induces a protective tissue-resident cDC1-ILC1 circuit through cDC1-intrinsic cGAS-STING-dependent IL-12 production.
In Cell Reports on 28 February 2023 by Hildreth, A. D., Padilla, E. T., et al.
PubMed
Tissue-resident immune cells are critical to the initiation and potentiation of inflammation. However, the tissue-protective cellular communication networks initiated by resident immunity during sterile inflammation are not well understood. Using single-cell transcriptomic analysis, we show the liver-resident cell connectome and signalome during acute liver injury. These analyses identify Il12b as a central regulator of liver injury-associated changes in gene expression. Interleukin (IL)-12 produced by conventional type 1 dendritic cells (cDC1s) is required for protection during acute injury through activation of interferon (IFN)-γ production by liver-resident type 1 innate lymphoid cells (ILC1s). Using a targeted in vivo CRISPR-Cas9 screen of innate immune sensing pathways, we find that cDC1-intrinsic cGAS-STING signaling acts upstream of IL-12 production to initiate early protective immune responses. Our study identifies the core communication hubs initiated by tissue-resident innate immune cells during sterile inflammation in vivo and implicates cDC1-derived IL-12 as an important regulator of this process. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Immunology and Microbiology,
- Mus musculus (House mouse)
T-cell activation Rho GTPase-activating protein maintains intestinal homeostasis by regulating intestinal T helper cells differentiation through the gut microbiota.
In Frontiers in Microbiology on 28 January 2023 by He, R., Chen, J., et al.
PubMed
Common variants of the T-cell activation Rho GTPase-activating protein (TAGAP) are associated with the susceptibility to human inflammatory bowel diseases (IBDs); however, the underlying mechanisms are still unknown. Here, we show that TAGAP deficiency or TAGAP expression downregulation caused by TAGAP gene polymorphism leads to decreased production of antimicrobial peptides (AMPs), such as reg3g, which subsequently causes dysregulation of the gut microbiota, which includes Akkermansia muciniphila and Bacteroides acidifaciens strains. These two strains can polarize T helper cell differentiation in the gut, and aggravate systemic disease associated with the dextran sodium sulfate-induced (DSS) disease's phenotype in mice. More importantly, we demonstrated that recombinant reg3g protein or anti-p40 monoclonal antibody exerted therapeutic effects for the treatment of DSS-induced colitis in wild-type and TAGAP-deficient mice, suggesting that they are potential medicines for human IBD treatment, and they may also have a therapeutic effect for the patients who carry the common variant of TAGAP rs212388. Copyright © 2023 He, Chen, Zhao, Shi, Du, Yi, Feng, Peng, Cui, Gao, Wang, Huang, Liu and Wang.
- Cancer Research
Agonistic anti-CD40 converts Tregs into Type 1 effectors within the tumor micro-environment
Preprint on BioRxiv : the Preprint Server for Biology on 20 October 2022 by Maltez, V., Arora, C., et al.
PubMed
Multiple cell types, molecules, and processes contribute to inhibition of anti-tumor effector responses, often frustrating effective immunotherapy. Among these, Foxp3+ CD4+ cells (Tregs) are well-recognized to play an immunosuppressive role in the tumor microenvironment. The first clinically successful checkpoint inhibitor, anti-CTLA-4 antibody, may deplete Tregs at least in part by antibody-dependent cellular cytotoxicity (ADCC), but this effect is unreliable in mice, including in a genetically engineered mouse model of pancreatic ductal adenocarcinoma (PDAC). In contrast, agonistic CD40 antibody, which serves as an effective therapy, is associated with notable Treg disappearance in the PDAC model. The mechanism of CD40-mediated Treg loss is poorly understood, as Tregs are CD40-negative. Here we have explored the mechanistic basis for the loss of Foxp3 T cells upon anti-CD40 treatment and find, using tissue-level multiplex immunostaining and orthogonal dissociated cell analyses, that Tregs are not depleted but converted into interferon- γ (IFN- γ ) producing, Type I CD4+ T effector cells. This process depends on IL-12 and IFN- γ signaling evoked by action of the anti-CD40 antibody on dendritic cells (DCs), especially BATF3-dependent cDC1s. These findings provide insight into a previously unappreciated mechanism of CD40 agonism as a potent anti-tumor intervention that promotes the re-programming of Tregs into tumor-reactive CD4+ effector T cells, markedly augmenting the anti-tumor response.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Impact of MyD88, Microbiota, and Location on Type 1 and Type 3 Innate Lymphoid Cells during Toxoplasma gondii Infection.
In ImmunoHorizons on 12 September 2022 by Snyder, L. M., Belmares-Ortega, J., et al.
PubMed
Toxoplasma gondii induces strong IFN-γ-based immunity. Innate lymphoid cells (ILC), in particular ILC1, are an important innate source of this protective cytokine during infection. Our objective was to determine how MyD88-dependent signaling influences ILC function during peroral compared with i.p. infection with T. gondii. MyD88 +/+ and MyD88 -/- mice were orally inoculated with ME49 cysts, and small intestinal lamina propria ILC were assessed using flow cytometry. We observed T-bet+ ILC1, retinoic acid-related orphan receptor γt+ ILC3, and a population of T-bet+retinoic acid-related orphan receptor γt+ double-positive ILC. In MyD88 -/- mice, IFN-γ-producing T-bet+ ILC1 frequencies were reduced compared with wild-type. Treatment of MyD88 -/- mice with an antibiotic mixture to deplete microflora reduced IFN-γ+ ILC1 frequencies. To examine ILC responses outside of the mucosal immune system, peritoneal exudate cells were collected from wild-type and knockout mice after i.p. inoculation with ME49 cysts. In this compartment, ILC were highly polarized to the ILC1 subset that increased significantly and became highly positive for IFN-γ over the course of infection. Increased ILC1 was associated with expression of the Ki67 cell proliferation marker, and the response was driven by IL-12p40. In the absence of MyD88, IFN-γ expression by ILC1 was not maintained, but proliferation remained normal. Collectively, these data reveal new aspects of ILC function that are influenced by location of infection and shaped further by MyD88-dependent signaling.Copyright © 2022 The Authors.
- Cancer Research
Platelets control liver tumor growth through P2Y12-dependent CD40L release in NAFLD.
In Cancer Cell on 12 September 2022 by Ma, C., Fu, Q., et al.
PubMed
Platelets, the often-overlooked component of the immune system, have been shown to promote tumor growth. Non-alcoholic fatty liver disease (NAFLD) is a common disease in the Western world and rising risk for hepatocellular carcinoma (HCC). Unexpectedly, we observed that platelets can inhibit the growth of established HCC in NAFLD mice. Through pharmacological inhibition and genetic depletion of P2Y12 as well as in vivo transfusion of wild-type (WT) or CD40L-/- platelets, we demonstrate that the anti-tumor function of platelets is mediated through P2Y12-dependent CD40L release, which leads to CD8+ T cell activation by the CD40 receptor. Unlike P2Y12 inhibition, blocking platelets with aspirin does not prevent platelet CD40L release nor accelerate HCC in NAFLD mice. Similar findings were observed in liver metastasis models. All together, our study reveals a complex role of platelets in tumor regulation. Anti-platelet treatment without inhibiting CD40L release could be considered for liver cancer patients with NAFLD. Published by Elsevier Inc.
- Immunology and Microbiology
Evaluation of Glutaminolysis in T Cells.
In Current Protocols on 1 September 2022 by Tajima, M. & Strober, W.
PubMed
The activity of living cells is necessarily dependent on the amount of available bioenergy. In T cells, the latter is mainly derived from ATP, a molecular energy "coin" generated by one of several metabolic processes that differ in their ability to satisfy energy demand. Thus, whereas naïve or quiescent T cells efficiently utilize oxidative phosphorylation to generate ATP, T cells subjected to antigenic stimulation followed by clonal expansion and cytokine production meet their increased need for energy by supplementing ATP generation by oxidative phosphorylation with ATP generation by glycolysis. Yet additional need for ATP can be met by other basic biologic sources of energy such as glutamine, an amino acid that is metabolized through a process called glutaminolysis to result in end products that flows into the TCA cycle and augment ATP generation by oxidative phosphorylation. It is now possible to track the dominant energy supplying processes (i.e., the ATP generation process) in differentiating or activated T cells in a real-time manner. Here, we provide one element of such tracking by describing protocols for the assessment of the contribution of glutaminolysis to overall ATP production within different T cell subsets. © 2022 Wiley Periodicals LLC. This article has been contributed to by US Government employees and their work is in the public domain in the USA. Basic Protocol 1: Evaluation of the role of glutaminolysis during T cell activation/differentiation Basic Protocol 2: Evaluation of the role of glutaminolysis in T cell responses utilizing glutaminolysis inhibitors Basic Protocol 3: Evaluation of the effect of glutaminolysis on cellular oxidative phosphorylation/glycolysis. © 2022 Wiley Periodicals LLC. This article has been contributed to by US Government employees and their work is in the public domain in the USA.
- Immunology and Microbiology,
- Mus musculus (House mouse)
Intestinal Inflammation Reversibly Alters the Microbiota to Drive Susceptibility to Clostridioides difficile Colonization in a Mouse Model of Colitis.
In mBio on 30 August 2022 by Barron, M. R., Sovacool, K. L., et al.
PubMed
Susceptibility to Clostridioides difficile infection (CDI) typically follows the administration of antibiotics. Patients with inflammatory bowel disease (IBD) have increased incidence of CDI, even in the absence of antibiotic treatment. However, the mechanisms underlying this susceptibility are not well understood. To explore the intersection between CDI and IBD, we recently described a mouse model where colitis triggered by the murine gut bacterium, Helicobacter hepaticus, in IL-10-/- mice led to susceptibility to C. difficile colonization without antibiotic administration. The current work disentangles the relative contributions of inflammation and gut microbiota in colonization resistance to C. difficile in this model. We show that inflammation drives changes in microbiota composition, which leads to CDI susceptibility. Decreasing inflammation with an anti-p40 monoclonal antibody promotes a shift of the microbiota back toward a colonization-resistant state. Transferring microbiota from susceptible and resistant mice to germfree animals transfers the susceptibility phenotype, supporting the primacy of the microbiota in colonization resistance. These findings shine light on the complex interactions between the host, microbiota, and C. difficile in the context of intestinal inflammation, and may form a basis for the development of strategies to prevent or treat CDI in IBD patients. IMPORTANCE Patients with inflammatory bowel disease (IBD) have an increased risk of developing C. difficile infection (CDI), even in the absence of antibiotic treatment. Yet, mechanisms regulating C. difficile colonization in IBD patients remain unclear. Here, we use an antibiotic-independent mouse model to demonstrate that intestinal inflammation alters microbiota composition to permit C. difficile colonization in mice with colitis. Notably, treating inflammation with an anti-p40 monoclonal antibody, a clinically relevant IBD therapeutic, restores microbiota-mediated colonization resistance to the pathogen. Through microbiota transfer experiments in germfree mice, we confirm that the microbiota shaped in the setting of IBD is the primary driver of susceptibility to C. diffiicile colonization. Collectively, our findings provide insight into CDI pathogenesis in the context of intestinal inflammation, which may inform methods to manage infection in IBD patients. More broadly, this work advances our understanding of mechanisms by which the host-microbiota interface modulates colonization resistance to C. difficile.
IL-24 intrinsically regulates Th17 cell pathogenicity in mice.
In The Journal of Experimental Medicine on 1 August 2022 by Sie, C., Kant, R., et al.
PubMed
In certain instances, Th17 responses are associated with severe immunopathology. T cell-intrinsic mechanisms that restrict pathogenic effector functions have been described for type 1 and 2 responses but are less well studied for Th17 cells. Here, we report a cell-intrinsic feedback mechanism that controls the pathogenicity of Th17 cells. Th17 cells produce IL-24, which prompts them to secrete IL-10. The IL-10-inducing function of IL-24 is independent of the cell surface receptor of IL-24 on Th17 cells. Rather, IL-24 is recruited to the inner mitochondrial membrane, where it interacts with the NADH dehydrogenase (ubiquinone) 1 α subcomplex subunit 13 (also known as Grim19), a constituent of complex I of the respiratory chain. Together, Grim19 and IL-24 promote the accumulation of STAT3 in the mitochondrial compartment. We propose that IL-24-guided mitochondrial STAT3 constitutes a rheostat to blunt extensive STAT3 deflections in the nucleus, which might then contribute to a robust IL-10 response in Th17 cells and a restriction of immunopathology in experimental autoimmune encephalomyelitis. © 2022 Sie et al.
- COVID-19,
- Immunology and Microbiology
Influenza Virus-like Particle-Based Hybrid Vaccine Containing RBD Induces Immunity against Influenza and SARS-CoV-2 Viruses.
In Vaccines on 14 June 2022 by Bommireddy, R., Stone, S., et al.
PubMed
Several approaches have produced an effective vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Since millions of people are exposed to influenza virus and SARS-CoV-2, it is of great interest to develop a two-in-one vaccine that will be able to protect against infection of both viruses. We have developed a hybrid vaccine for SARS-CoV-2 and influenza viruses using influenza virus-like particles (VLP) incorporated by protein transfer with glycosylphosphatidylinositol (GPI)-anchored SARS-CoV-2 RBD fused to GM-CSF as an adjuvant. GPI-RBD-GM-CSF fusion protein was expressed in CHO-S cells, purified and incorporated onto influenza VLPs to develop the hybrid vaccine. Our results show that the hybrid vaccine induced a strong antibody response and protected mice from both influenza virus and mouse-adapted SARS-CoV-2 challenges, with vaccinated mice having significantly lower lung viral titers compared to naive mice. These results suggest that a hybrid vaccine strategy is a promising approach for developing multivalent vaccines to prevent influenza A and SARS-CoV-2 infections.
- In Vivo,
- Mus musculus (House mouse),
- Biochemistry and Molecular biology,
- Immunology and Microbiology
Differential regulation of transcription factor T-bet induction during NK cell development and T helper-1 cell differentiation.
In Immunity on 12 April 2022 by Fang, D., Cui, K., et al.
PubMed
Adaptive CD4+ T helper cells and their innate counterparts, innate lymphoid cells, utilize an identical set of transcription factors (TFs) for their differentiation and functions. However, similarities and differences in the induction of these TFs in related lymphocytes are still elusive. Here, we show that T helper-1 (Th1) cells and natural killer (NK) cells displayed distinct epigenomes at the Tbx21 locus, which encodes T-bet, a critical TF for regulating type 1 immune responses. The initial induction of T-bet in NK precursors was dependent on the NK-specific DNase I hypersensitive site Tbx21-CNS-3, and the expression of the interleukin-18 (IL-18) receptor; IL-18 induced T-bet expression through the transcription factor RUNX3, which bound to Tbx21-CNS-3. By contrast, signal transducer and activator of transcription (STAT)-binding motifs within Tbx21-CNS-12 were critical for IL-12-induced T-bet expression during Th1 cell differentiation both in vitro and in vivo. Thus, type 1 innate and adaptive lymphocytes utilize distinct enhancer elements for their development and differentiation. Published by Elsevier Inc.
- Immunology and Microbiology
Intestinal inflammation reversibly alters the microbiota to drive susceptibility to i>Clostridioides difficile/i> colonization in a mouse model of colitis
Preprint on BioRxiv : the Preprint Server for Biology on 8 April 2022 by Barron, M. R., Sovacool, K. L., et al.
PubMed
Susceptibility to Clostridioides difficile infection (CDI) typically follows the administration of antibiotics. Patients with inflammatory bowel disease (IBD) have increased incidence of CDI, even in the absence of antibiotic treatment. However, the mechanisms underlying this susceptibility are not well understood. To explore the intersection between CDI and IBD, we recently described a mouse model where colitis triggered by the murine gut bacterium, Helicobacter hepaticus, in IL-10 -/- mice led to susceptibility to C. difficile colonization without antibiotic administration. The current work disentangles the relative contributions of inflammation and gut microbiota in colonization resistance to C. difficile in this model. We show that inflammation drives changes in microbiota composition, which leads to CDI susceptibility. Decreasing inflammation with an anti-p40 monoclonal antibody promotes a shift of the microbiota back toward a colonization-resistant state. Transferring microbiota from susceptible and resistant mice to germ-free animals transfers the susceptibility phenotype, supporting the primacy of the microbiota in colonization resistance. These findings shine light on the complex interactions between the host, microbiota, and C. difficile in the context of intestinal inflammation, and may form a basis for the development of strategies to prevent or treat CDI in IBD patients. h4>Importance/h4> Patients with inflammatory bowel disease (IBD) have an increased risk of developing C. difficile infection (CDI), even in the absence of antibiotic treatment. Yet, mechanisms regulating C. difficile colonization in IBD patients remain unclear. Here, we use an antibiotic-independent mouse model to demonstrate that intestinal inflammation alters microbiota composition to permit C. difficile colonization in mice with colitis. Notably, treating inflammation with an anti-p40 monoclonal antibody, a clinically relevant IBD therapeutic, restores microbiota-mediated colonization resistance to the pathogen. Through microbiota transfer experiments in germ-free mice, we confirm that the microbiota shaped in the setting of IBD is the primary driver of susceptibility to C. diffiicile colonization. Collectively, our findings provide insight into CDI pathogenesis in the context of intestinal inflammation, which may inform methods to manage infection in IBD patients. More broadly, this work advances our understanding of mechanisms by which the host-microbiota interface modulates colonization resistance to C. difficile .
- Cancer Research,
- Immunology and Microbiology
Lin28B-high breast cancer cells promote immune suppression in the lung pre-metastatic niche via exosomes and support cancer progression.
In Nature Communications on 16 February 2022 by Qi, M., Xia, Y., et al.
PubMed
The formation of pre-metastatic niche is a key step in the metastatic burden. The pluripotent factor Lin28B is frequently expressed in breast tumors and is particularly upregulated in the triple negative breast cancer subtype. Here, we demonstrate that Lin28B promotes lung metastasis of breast cancer by building an immune-suppressive pre-metastatic niche. Lin28B enables neutrophil recruitment and N2 conversion. The N2 neutrophils are then essential for immune suppression in pre-metastatic lung by PD-L2 up-regulation and a dysregulated cytokine milieu. We also identify that breast cancer-released exosomes with low let-7s are a prerequisite for Lin28B-induced immune suppression. Moreover, Lin28B-induced breast cancer stem cells are the main sources of low-let-7s exosomes. Clinical data further verify that high Lin28B and low let-7s in tumors are both indicators for poor prognosis and lung metastasis in breast cancer patients. Together, these data reveal a mechanism by which Lin28B directs the formation of an immune-suppressive pre-metastatic niche. © 2022. The Author(s).
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Enterocyte-innate lymphoid cell crosstalk drives early IFN-γ-mediated control of Cryptosporidium.
In Mucosal Immunology on 1 February 2022 by Gullicksrud, J. A., Sateriale, A., et al.
PubMed
The intestinal parasite, Cryptosporidium, is a major contributor to global child mortality and causes opportunistic infection in immune deficient individuals. Innate resistance to Cryptosporidium, which specifically invades enterocytes, is dependent on the production of IFN-γ, yet whether enterocytes contribute to parasite control is poorly understood. In this study, utilizing a mouse-adapted strain of C. parvum, we show that epithelial-derived IL-18 synergized with IL-12 to stimulate innate lymphoid cell (ILC) production of IFN-γ required for early parasite control. The loss of IFN-γ-mediated STAT1 signaling in enterocytes, but not dendritic cells or macrophages, antagonized early parasite control. Transcriptional profiling of enterocytes from infected mice identified an IFN-γ signature and enrichment of the anti-microbial effectors IDO, GBP, and IRG. Deletion experiments identified a role for Irgm1/m3 in parasite control. Thus, enterocytes promote ILC production of IFN-γ that acts on enterocytes to restrict the growth of Cryptosporidium. © 2021. The Author(s), under exclusive licence to Society for Mucosal Immunology.
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Induction of IL-12p40 and type 1 immunity by Toxoplasma gondii in the absence of the TLR-MyD88 signaling cascade.
In PLoS Pathogens on 1 October 2021 by Snyder, L. M., Doherty, C. M., et al.
PubMed
Toxoplasma gondii is an orally acquired pathogen that induces strong IFN-γ based immunity conferring protection but that can also be the cause of immunopathology. The response in mice is driven in part by well-characterized MyD88-dependent signaling pathways. Here we focus on induction of less well understood immune responses that do not involve this Toll-like receptor (TLR)/IL-1 family receptor adaptor molecule, in particular as they occur in the intestinal mucosa. Using eYFP-IL-12p40 reporter mice on an MyD88-/- background, we identified dendritic cells, macrophages, and neutrophils as cellular sources of MyD88-independent IL-12 after peroral T. gondii infection. Infection-induced IL-12 was lower in the absence of MyD88, but was still clearly above noninfected levels. Overall, this carried through to the IFN-γ response, which while generally decreased was still remarkably robust in the absence of MyD88. In the latter mice, IL-12 was strictly required to induce type I immunity. Type 1 and type 3 innate lymphoid cells (ILC), CD4+ T cells, and CD8+ T cells each contributed to the IFN-γ pool. We report that ILC3 were expanded in infected MyD88-/- mice relative to their MyD88+/+ counterparts, suggesting a compensatory response triggered by loss of MyD88. Furthermore, bacterial flagellin and Toxoplasma specific CD4+ T cell populations in the lamina propria expanded in response to infection in both WT and KO mice. Finally, we show that My88-independent IL-12 and T cell mediated IFN-γ production require the presence of the intestinal microbiota. Our results identify MyD88-independent intestinal immune pathways induced by T. gondii including myeloid cell derived IL-12 production, downstream type I immunity and IFN-γ production by ILC1, ILC3, and T lymphocytes. Collectively, our data reveal an underlying network of immune responses that do not involve signaling through MyD88.
- Immunology and Microbiology
Tonic interferon restricts pathogenic IL-17-driven inflammatory disease via balancing the microbiome.
In eLife on 11 August 2021 by Marié, I. J., Brambilla, L., et al.
PubMed
Maintenance of immune homeostasis involves a synergistic relationship between the host and the microbiome. Canonical interferon (IFN) signaling controls responses to acute microbial infection, through engagement of the STAT1 transcription factor. However, the contribution of tonic levels of IFN to immune homeostasis in the absence of acute infection remains largely unexplored. We report that STAT1 KO mice spontaneously developed an inflammatory disease marked by myeloid hyperplasia and splenic accumulation of hematopoietic stem cells. Moreover, these animals developed inflammatory bowel disease. Profiling gut bacteria revealed a profound dysbiosis in the absence of tonic IFN signaling, which triggered expansion of TH17 cells and loss of splenic Treg cells. Reduction of bacterial load by antibiotic treatment averted the TH17 bias and blocking IL17 signaling prevented myeloid expansion and splenic stem cell accumulation. Thus, tonic IFNs regulate gut microbial ecology, which is crucial for maintaining physiologic immune homeostasis and preventing inflammation. © 2021, Marié et al.
- Cancer Research
A novel miR1983-TLR7-IFNβ circuit licenses NK cells to kill glioma cells, and is under the control of galectin-1.
In Oncoimmunology on 13 July 2021 by Shah, D., Comba, A., et al.
PubMed
Although pharmacological stimulation of TLRs has anti-tumor effects, it has not been determined whether endogenous stimulation of TLRs can lead to tumor rejection. Herein, we demonstrate the existence of an innate anti-glioma NK-mediated circuit initiated by glioma-released miR-1983 within exosomes, and which is under the regulation of galectin-1 (Gal-1). We demonstrate that miR-1983 is an endogenous TLR7 ligand that activates TLR7 in pDCs and cDCs through a 5'-UGUUU-3' motif at its 3' end. TLR7 activation and downstream signaling through MyD88-IRF5/IRF7 stimulates secretion of IFN-β. IFN-β then stimulates NK cells resulting in the eradication of gliomas. We propose that successful immunotherapy for glioma could exploit this endogenous innate immune circuit to activate TLR7 signaling and stimulate powerful anti-glioma NK activity, at least 10-14 days before the activation of anti-tumor adaptive immunity. © 2021 The Author(s). Published with license by Taylor Francis Group, LLC.
- Immunology and Microbiology
Two sequential activation modules control the differentiation of protective T helper-1 (Th1) cells.
In Immunity on 13 April 2021 by Krueger, P. D., Goldberg, M. F., et al.
PubMed
Interferon-γ (IFN-γ)-producing CD4+ T helper-1 (Th1) cells are critical for protection from microbes that infect the phagosomes of myeloid cells. Current understanding of Th1 cell differentiation is based largely on reductionist cell culture experiments. We assessed Th1 cell generation in vivo by studying antigen-specific CD4+ T cells during infection with the phagosomal pathogen Salmonella enterica (Se), or influenza A virus (IAV), for which CD4+ T cells are less important. Both microbes induced T follicular helper (Tfh) and interleukin-12 (IL-12)-independent Th1 cells. During Se infection, however, the Th1 cells subsequently outgrew the Tfh cells via an IL-12-dependent process and formed subsets with increased IFN-γ production, ZEB2-transcription factor-dependent cytotoxicity, and capacity to control Se infection. Our results indicate that many infections induce a module that generates Tfh and poorly differentiated Th1 cells, which is followed in phagosomal infections by an IL-12-dependent Th1 cell amplification module that is critical for pathogen control.Copyright © 2021 Elsevier Inc. All rights reserved.