InVivoMAb anti-mouse MAdCAM-1
Product Details
The MECA-367 monoclonal antibody reacts with mouse MAdCAM-1 (mucosal addressin cell adhesion molecule-1) a 50-60 kDa member of the Ig superfamily. MAdCAM-1 is primarily expressed on high endothelial venules in Peyer’s patches, mesenteric lymph nodes and gut lamina propria. MAdCAM-1 interacts with LPAM-1 and CD62L to facilitate lymphocyte tethering, rolling, and homing. The MECA-367 antibody has been shown to block the interaction of MAdCAM-1 with its receptor in vivo and in vitro.Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Endothelial cells isolated from BALB/c mouse |
| Reported Applications |
in vivo MAdCAM-1 neutralization Immunofluorescence |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107725 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Recommended Products
Immunofluorescence
Gillespie, A. L., et al. (2016). "Genomic Modifiers of Natural Killer Cells, Immune Responsiveness and Lymphoid Tissue Remodeling Together Increase Host Resistance to Viral Infection" PLoS Pathog 12(2): e1005419. PubMed
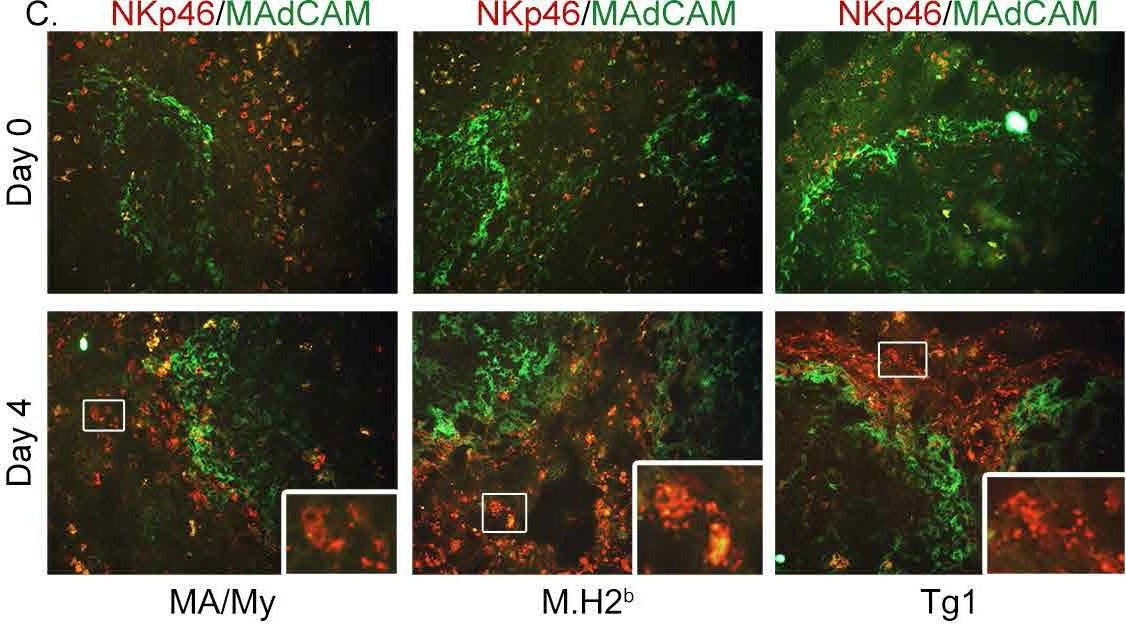
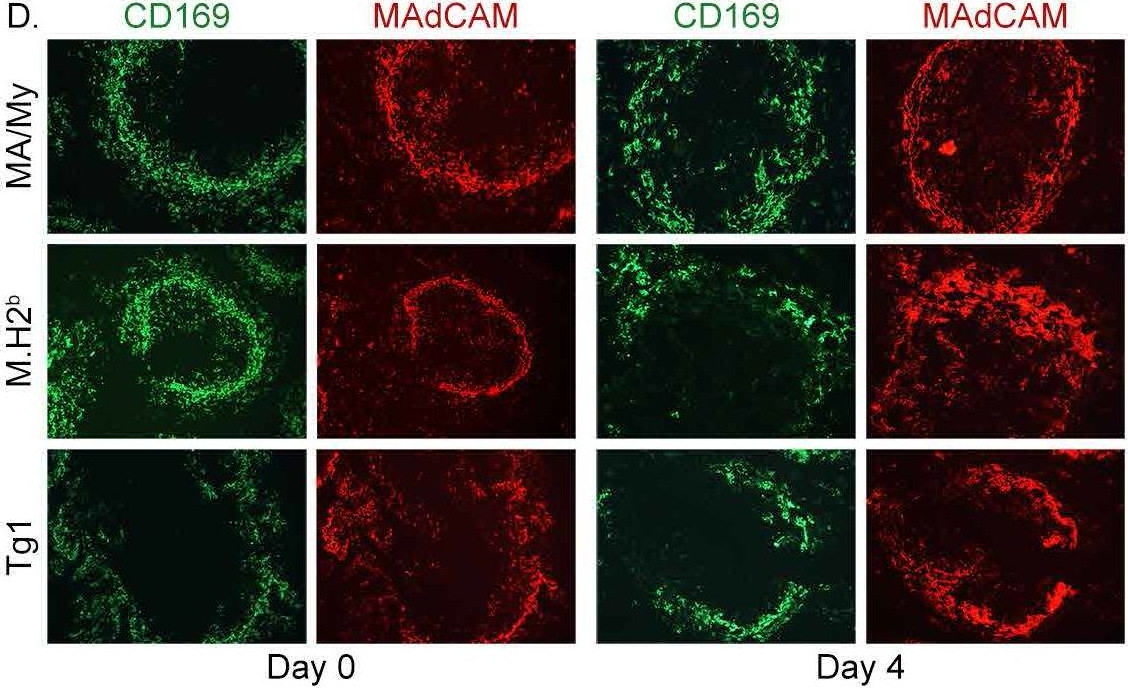
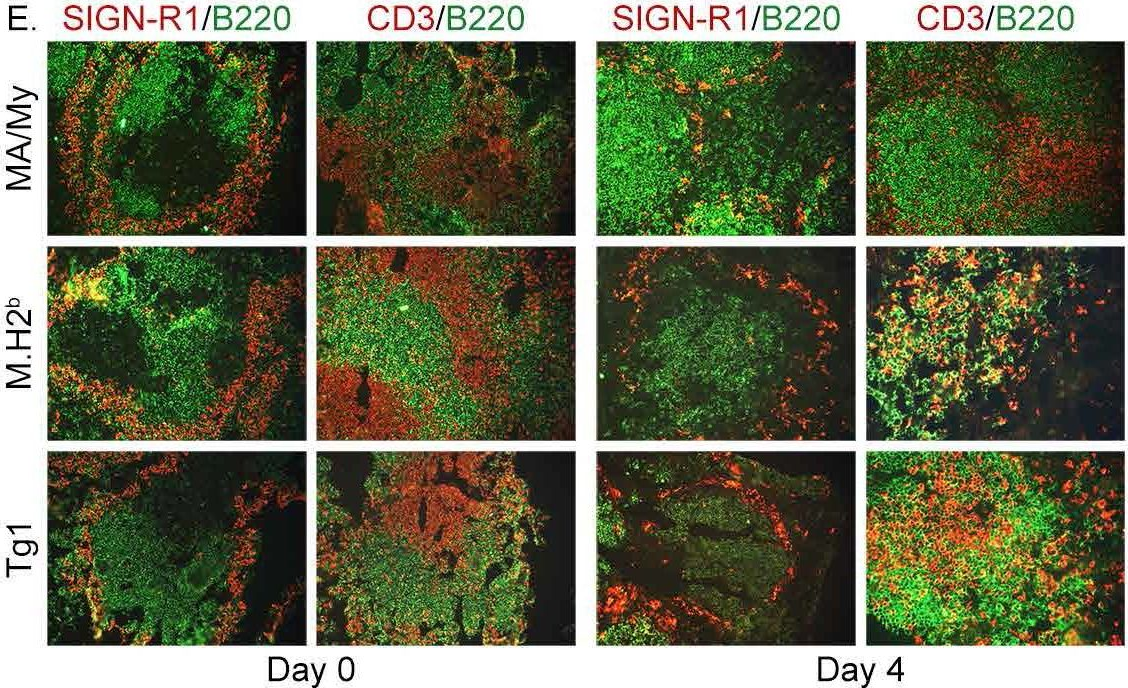
The MHC class I D(k) molecule supplies vital host resistance during murine cytomegalovirus (MCMV) infection. Natural killer (NK) cells expressing the Ly49G2 inhibitory receptor, which specifically binds D(k), are required to control viral spread. The extent of D(k)-dependent host resistance, however, differs significantly amongst related strains of mice, C57L and MA/My. As a result, we predicted that relatively small-effect modifier genetic loci might together shape immune cell features, NK cell reactivity, and the host immune response to MCMV. A robust D(k)-dependent genetic effect, however, has so far hindered attempts to identify additional host resistance factors. Thus, we applied genomic mapping strategies and multicolor flow cytometric analysis of immune cells in naive and virus-infected hosts to identify genetic modifiers of the host immune response to MCMV. We discovered and validated many quantitative trait loci (QTL); these were mapped to at least 19 positions on 16 chromosomes. Intriguingly, one newly discovered non-MHC locus (Cmv5) controlled splenic NK cell accrual, secondary lymphoid organ structure, and lymphoid follicle development during MCMV infection. We infer that Cmv5 aids host resistance to MCMV infection by expanding NK cells needed to preserve and protect essential tissue structural elements, to enhance lymphoid remodeling and to increase viral clearance in spleen.
in vivo MAdCAM-1 neutralization, Immunofluorescence
Peske, J. D., et al. (2015). "Effector lymphocyte-induced lymph node-like vasculature enables naive T-cell entry into tumours and enhanced anti-tumour immunity" Nat Commun 6: 7114. PubMed
The presence of lymph node (LN)-like vasculature in tumours, characterized by expression of peripheral node addressin and chemokine CCL21, is correlated with T-cell infiltration and positive prognosis in breast cancer and melanoma patients. However, mechanisms controlling the development of LN-like vasculature and how it might contribute to a beneficial outcome for cancer patients are unknown. Here we demonstrate that LN-like vasculature is present in murine models of melanoma and lung carcinoma. It enables infiltration by naive T cells that significantly delay tumour outgrowth after intratumoral activation. Development of this vasculature is controlled by a mechanism involving effector CD8 T cells and NK cells that secrete LTalpha3 and IFNgamma. LN-like vasculature is also associated with organized aggregates of B lymphocytes and gp38(+) fibroblasts, which resemble tertiary lymphoid organs that develop in models of chronic inflammation. These results establish LN-like vasculature as both a consequence of and key contributor to anti-tumour immunity.
in vivo MAdCAM-1 neutralization, Immunofluorescence
Wang, X., et al. (2014). "Integrin-mediated interactions between B cells and follicular dendritic cells influence germinal center B cell fitness" J Immunol 192(10): 4601-4609. PubMed
Integrin-ligand interactions between germinal center (GC) B cells and Ag-presenting follicular dendritic cells (FDCs) have been suggested to play central roles during GC responses, but their in vivo requirement has not been directly tested. In this study, we show that, whereas integrins alphaLbeta2 and alpha4beta1 are highly expressed and functional on mouse GC B cells, removal of single integrins or their ligands had little effect on B cell participation in the GC response. Combined beta2 integrin deficiency and alpha4 integrin blockade also did not affect the GC response against a particulate Ag. However, the combined integrin deficiency did cause B cells to be outcompeted in splenic GC responses against a soluble protein Ag and in mesenteric lymph node GC responses against gut-derived Ags. Similar findings were made for beta2-deficient B cells in mice lacking VCAM1 on FDCs. The reduced fitness of the GC B cells did not appear to be due to decreased Ag acquisition, proliferation rates, or pAKT levels. In summary, our findings provide evidence that alphaLbeta2 and alpha4beta1 play overlapping and context-dependent roles in supporting interactions with FDCs that can augment the fitness of responding GC B cells. We also find that mouse GC B cells upregulate alphavbeta3 and adhere to vitronectin and milk-fat globule epidermal growth factor VIII protein. Integrin beta3-deficient B cells contributed in a slightly exaggerated manner to GC responses, suggesting this integrin has a regulatory function in GC B cells.
in vivo MAdCAM-1 neutralization, Immunofluorescence
Perez, J., et al. (2011). "Accumulation of CD4+ T cells in the colon of CsA-treated mice following myeloablative conditioning and bone marrow transplantation" Am J Physiol Gastrointest Liver Physiol 300(5): G843-852. PubMed
Syngeneic graft vs. host disease (SGVHD) was first described as a graft vs. host disease-like syndrome that developed in rats following syngeneic bone marrow transplantation (BMT) and cyclosporin A (CsA) treatment. SGVHD can be induced by reconstitution of lethally irradiated mice with syngeneic bone marrow cells followed by 21 days of treatment with the immunosuppressive agent CsA. Clinical symptoms of the disease appear 2-3 wk following cessation of CsA therapy, and disease-associated inflammation occurs primarily in the colon and liver. CD4(+) T cells have been shown to play an important role in the inflammatory response observed in the gut of SGVHD mice. Time-course studies revealed a significant increase in migration of CD4(+) T cells into the colon during CsA therapy, as well as significantly elevated mRNA levels of TNF-alpha, proinflammatory chemokines, and cell adhesion molecules in colonic tissue of CsA-treated animals compared with BMT controls, as early as day 14 post-BMT. Homing studies revealed a greater migration of labeled CD4(+) T cells into the gut of CsA-treated mice at day 21 post-BMT than control animals via CsA-induced upregulation of mucosal addressin cell adhesion molecule. This study demonstrates that, during the 21 days of immunosuppressive therapy, functional mechanisms are in place that result in increased homing of CD4(+) T effector cells to colons of CsA-treated mice.
- Immu-depl,
- In Vivo,
- Mus musculus (House mouse),
- Immunology and Microbiology
Recruitment of α4β7 monocytes and neutrophils to the brain in experimental colitis is associated with elevated cytokines and anxiety-like behavior.
In Journal of Neuroinflammation on 4 April 2022 by Cluny, N. L., Nyuyki, K. D., et al.
PubMed
Behavioral comorbidities, such as anxiety and depression, are a prominent feature of IBD. The signals from the inflamed gut that cause changes in the brain leading to these behavioral comorbidities remain to be fully elucidated. We tested the hypothesis that enhanced leukocyte-cerebral endothelial cell interactions occur in the brain in experimental colitis, mediated by α4β7 integrin, to initiate neuroimmune activation and anxiety-like behavior. Female mice treated with dextran sodium sulfate were studied at the peak of acute colitis. Circulating leukocyte populations were determined using flow cytometry. Leukocyte-cerebral endothelial cell interactions were examined using intravital microscopy in mice treated with anti-integrin antibodies. Brain cytokine and chemokines were assessed using a multiplex assay in animals treated with anti-α4β7 integrin. Anxiety-like behavior was assessed using an elevated plus maze in animals after treatment with an intracerebroventricular injection of interleukin 1 receptor antagonist. The proportion of classical monocytes expressing α4β7 integrin was increased in peripheral blood of mice with colitis. An increase in the number of rolling and adherent leukocytes on cerebral endothelial cells was observed, the majority of which were neutrophils. Treatment with anti-α4β7 integrin significantly reduced the number of rolling leukocytes. After anti-Ly6C treatment to deplete monocytes, the number of rolling and adhering neutrophils was significantly reduced in mice with colitis. Interleukin-1β and CCL2 levels were elevated in the brain and treatment with anti-α4β7 significantly reduced them. Enhanced anxiety-like behavior in mice with colitis was reversed by treatment with interleukin 1 receptor antagonist. In experimental colitis, α4β7 integrin-expressing monocytes direct the recruitment of neutrophils to the cerebral vasculature, leading to elevated cytokine levels. Increased interleukin-1β mediates anxiety-like behavior. © 2022. The Author(s).
- Neuroscience
Leukocyte - Cerebral Endothelial Cell Interactions in the Brain Lead to Anxiety-like Behaviour in Experimental Colitis
Preprint on Research Square on 3 December 2021 by Cluny, N. L., Nyuyki, K. D., et al.
PubMed
BACKGROUND Behavioral comorbidities, such as anxiety and depression, are a prominent feature of IBD. The signals from the inflamed gut that cause changes in the brain leading to these behavioral comorbidities remain to be fully elucidated. We tested the hypothesis that enhanced leukocyte - cerebral endothelial cell interactions in experimental colitis initiate neuroimmune activation leading to anxiety-like behaviour. METHODS Male and female mice treated with dextran sodium sulfate were studied at the peak of acute colitis. Circulating leukocyte populations were determined using flow cytometry. Leukocyte - cerebral endothelial cell interactions were examined using intravital microscopy in mice treated with anti-integrin antibodies. Brain cytokine and chemokines were assessed using a multiplex assay in animals treated with anti-α4β7 integrin. Anxiety-like behavior was assessed using an elevated plus maze in animals after treatment with an intracerebroventricular injection of interleukin 1 receptor antagonist. RESULTS The proportion of classical monocytes expressing α4β7 integrin was increased in peripheral blood of mice with colitis. An increase in the number of rolling and adherent leukocytes on cerebral endothelial cells was observed, the majority of which were neutrophils. Treatment with anti-α4β7 integrin significantly reduced the number of rolling leukocytes. After anti-Ly6C treatment to deplete monocytes, the number of rolling and adhering neutrophils were significantly reduced in mice with colitis. Interleukin-1β levels were elevated in the brain and treatment with anti-α4β7 significantly reduced them. Enhanced anxiety-like behaviour in mice with colitis was reversed by treatment with interleukin 1 receptor antagonist. CONCLUSIONS α4β7 integrin expressing monocytes direct the recruitment of neutrophils to the brain vasculature, leading to elevated cytokine levels that mediate anxiety-like behaviour in experimental colitis.
- Mus musculus (House mouse),
- Immunology and Microbiology
Optogenetic activation of local colonic sympathetic innervations attenuates colitis by limiting immune cell extravasation.
In Immunity on 11 May 2021 by Schiller, M., Azulay-Debby, H., et al.
PubMed
The sympathetic nervous system is composed of an endocrine arm, regulating blood adrenaline and noradrenaline, and a local arm, a network of fibers innervating immune organs. Here, we investigated the impact of the local arm of the SNS in an inflammatory response in the colon. Intra-rectal insertion of an optogenetic probe in mice engineered to express channelrhodopsin-2 in tyrosine hydroxylase cells activated colonic sympathetic fibers. In contrast to systemic application of noradrenaline, local activation of sympathetic fibers attenuated experimental colitis and reduced immune cell abundance. Gene expression profiling showed decreased endothelial expression of the adhesion molecule MAdCAM-1 upon optogenetic stimulation; this decrease was sensitive to adrenergic blockers and 6-hydroxydopamine. Antibody blockade of MAdCAM-1 abrogated the optogenetic effect on immune cell extravasation into the colon and the pathology. Thus, sympathetic fibers control colonic inflammation by regulating immune cell extravasation from circulation, a mechanism likely relevant in multiple organs.Copyright © 2021 The Authors. Published by Elsevier Inc. All rights reserved.
- Immunology and Microbiology,
- Stem Cells and Developmental Biology
T Cell Recruitment to the Intestinal Stem Cell Compartment Drives Immune-Mediated Intestinal Damage after Allogeneic Transplantation.
In Immunity on 16 July 2019 by Fu, Y. Y., Egorova, A., et al.
PubMed
The key sites within the gastrointestinal (GI) tract where T cells mediate effector responses and the impact of these responses on intestinal stem cells (ISCs) remain unclear. Using experimental bone marrow transplantation to model immune-mediated GI damage and 3D imaging to analyze T cell localization, we found that the ISC compartment is the primary intestinal site targeted by T cells after transplantation. Recruitment to the crypt base region resulted in direct T cell engagement with the stem cell compartment and loss of crypt base columnar ISCs, which expressed both MHC classes I and II. Vasculature expressing the adhesion molecule MAdCAM-1 clustered near the crypt base, preferentially regulating crypt compartment invasion and ISC reduction without affecting T cell migration to villi. These findings indicate that allogeneic T cells rapidly access the stem cell niche after transplantation, and this targeted recruitment to the stem cell compartment results in ISC loss during immune-mediated GI damage. Copyright © 2019 Elsevier Inc. All rights reserved.
- IHC-IF,
- Mus musculus (House mouse),
- Immunology and Microbiology
Genomic Modifiers of Natural Killer Cells, Immune Responsiveness and Lymphoid Tissue Remodeling Together Increase Host Resistance to Viral Infection.
In PLoS Pathogens on 1 February 2016 by Gillespie, A. L., Teoh, J., et al.
PubMed
The MHC class I D(k) molecule supplies vital host resistance during murine cytomegalovirus (MCMV) infection. Natural killer (NK) cells expressing the Ly49G2 inhibitory receptor, which specifically binds D(k), are required to control viral spread. The extent of D(k)-dependent host resistance, however, differs significantly amongst related strains of mice, C57L and MA/My. As a result, we predicted that relatively small-effect modifier genetic loci might together shape immune cell features, NK cell reactivity, and the host immune response to MCMV. A robust D(k)-dependent genetic effect, however, has so far hindered attempts to identify additional host resistance factors. Thus, we applied genomic mapping strategies and multicolor flow cytometric analysis of immune cells in naive and virus-infected hosts to identify genetic modifiers of the host immune response to MCMV. We discovered and validated many quantitative trait loci (QTL); these were mapped to at least 19 positions on 16 chromosomes. Intriguingly, one newly discovered non-MHC locus (Cmv5) controlled splenic NK cell accrual, secondary lymphoid organ structure, and lymphoid follicle development during MCMV infection. We infer that Cmv5 aids host resistance to MCMV infection by expanding NK cells needed to preserve and protect essential tissue structural elements, to enhance lymphoid remodeling and to increase viral clearance in spleen.
- In Vivo,
- IHC-IF,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Effector lymphocyte-induced lymph node-like vasculature enables naive T-cell entry into tumours and enhanced anti-tumour immunity.
In Nature Communications on 13 May 2015 by Peske, J. D., Thompson, E. D., et al.
PubMed
The presence of lymph node (LN)-like vasculature in tumours, characterized by expression of peripheral node addressin and chemokine CCL21, is correlated with T-cell infiltration and positive prognosis in breast cancer and melanoma patients. However, mechanisms controlling the development of LN-like vasculature and how it might contribute to a beneficial outcome for cancer patients are unknown. Here we demonstrate that LN-like vasculature is present in murine models of melanoma and lung carcinoma. It enables infiltration by naive T cells that significantly delay tumour outgrowth after intratumoral activation. Development of this vasculature is controlled by a mechanism involving effector CD8 T cells and NK cells that secrete LTα3 and IFNγ. LN-like vasculature is also associated with organized aggregates of B lymphocytes and gp38(+) fibroblasts, which resemble tertiary lymphoid organs that develop in models of chronic inflammation. These results establish LN-like vasculature as both a consequence of and key contributor to anti-tumour immunity.



