InVivoMAb anti-mouse CD40
Product Details
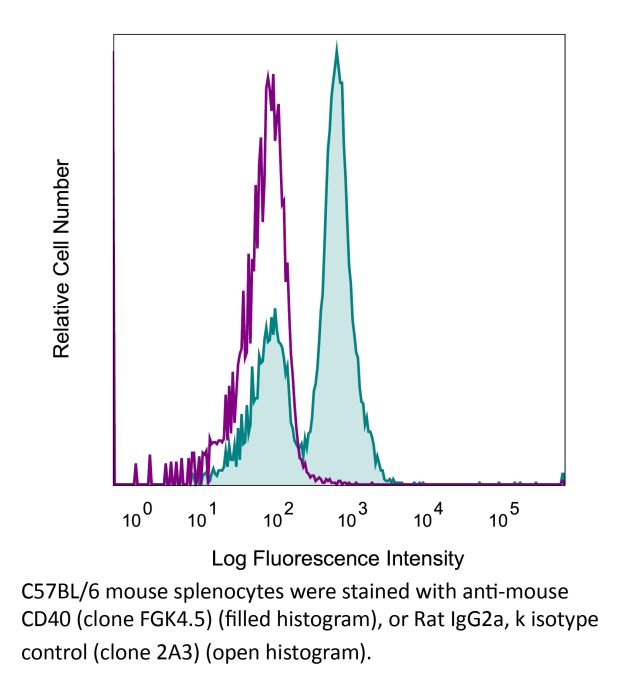
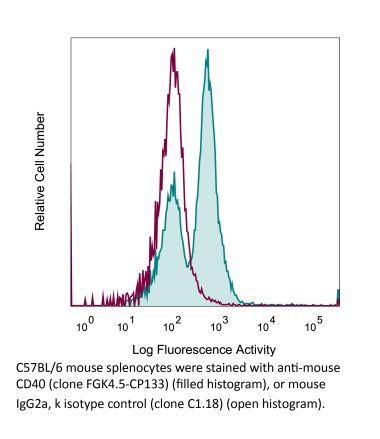
The FGK4.5 monoclonal antibody reacts with mouse CD40 also known as Bp50. CD40 is a 48 kDa type I transmembrane glycoprotein that belongs to the tumor necrosis factor receptor (TNFR) superfamily. CD40 is expressed broadly on antigen-presenting cells (APCs) such as dendritic cells, B cells, macrophages, and monocytes as well as non-immune endothelial cells, basal epithelial cells, and a range of tumors. Upon binding to its ligand CD154, CD40 acts as a costimulatory molecule for the activation of B cells, dendritic cells, monocytes, and other APCs. CD40 plays roles in B cell activation, differentiation, proliferation and Ig isotype switching as well as dendritic cell maturation. Agonistic CD40 monoclonal antibodies have been shown to activate APCs and promote anti-tumor T cell responses. The FGK4.5 antibody is an agonistic antibody that has been shown to activate CD40 expressing APCs. FGK4.5 can also be used to inhibit CD40/CD154 interaction in vitro and in vivo.Specifications
| Isotype | Rat IgG2a |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse CD40 fusion protein |
| Reported Applications |
in vivo CD40 activation in vitro B cell stimulation/activation |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
<2EU/mg (<0.002EU/μg) Determined by LAL gel clotting assay |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107601 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo CD40 activation
Bauche, D., et al. (2018). "LAG3(+) Regulatory T Cells Restrain Interleukin-23-Producing CX3CR1(+) Gut-Resident Macrophages during Group 3 Innate Lymphoid Cell-Driven Colitis" Immunity 49(2): 342-352 e345. PubMed
Interleukin-22 (IL-22)-producing group 3 innate lymphoid cells (ILC3) maintains gut homeostasis but can also promote inflammatory bowel disease (IBD). The regulation of ILC3-dependent colitis remains to be elucidated. Here we show that Foxp3(+) regulatory T cells (Treg cells) prevented ILC3-mediated colitis in an IL-10-independent manner. Treg cells inhibited IL-23 and IL-1beta production from intestinal-resident CX3CR1(+) macrophages but not CD103(+) dendritic cells. Moreover, Treg cells restrained ILC3 production of IL-22 through suppression of CX3CR1(+) macrophage production of IL-23 and IL-1beta. This suppression was contact dependent and was mediated by latent activation gene-3 (LAG-3)-an immune checkpoint receptor-expressed on Treg cells. Engagement of LAG-3 on MHC class II drove profound immunosuppression of CX3CR1(+) tissue-resident macrophages. Our study reveals that the health of the intestinal mucosa is maintained by an axis driven by Treg cells communication with resident macrophages that withhold inflammatory stimuli required for ILC3 function.
in vivo CD40 activation
Carmi, Y., et al. (2015). "Allogeneic IgG combined with dendritic cell stimuli induce antitumour T-cell immunity" Nature 521(7550): 99-104. PubMed
Whereas cancers grow within host tissues and evade host immunity through immune-editing and immunosuppression, tumours are rarely transmissible between individuals. Much like transplanted allogeneic organs, allogeneic tumours are reliably rejected by host T cells, even when the tumour and host share the same major histocompatibility complex alleles, the most potent determinants of transplant rejection. How such tumour-eradicating immunity is initiated remains unknown, although elucidating this process could provide the basis for inducing similar responses against naturally arising tumours. Here we find that allogeneic tumour rejection is initiated in mice by naturally occurring tumour-binding IgG antibodies, which enable dendritic cells (DCs) to internalize tumour antigens and subsequently activate tumour-reactive T cells. We exploited this mechanism to treat autologous and autochthonous tumours successfully. Either systemic administration of DCs loaded with allogeneic-IgG-coated tumour cells or intratumoral injection of allogeneic IgG in combination with DC stimuli induced potent T-cell-mediated antitumour immune responses, resulting in tumour eradication in mouse models of melanoma, pancreas, lung and breast cancer. Moreover, this strategy led to eradication of distant tumours and metastases, as well as the injected primary tumours. To assess the clinical relevance of these findings, we studied antibodies and cells from patients with lung cancer. T cells from these patients responded vigorously to autologous tumour antigens after culture with allogeneic-IgG-loaded DCs, recapitulating our findings in mice. These results reveal that tumour-binding allogeneic IgG can induce powerful antitumour immunity that can be exploited for cancer immunotherapy.
in vivo CD40 activation
Conde, P., et al. (2015). "DC-SIGN(+) Macrophages Control the Induction of Transplantation Tolerance" Immunity 42(6): 1143-1158. PubMed
Tissue effector cells of the monocyte lineage can differentiate into different cell types with specific cell function depending on their environment. The phenotype, developmental requirements, and functional mechanisms of immune protective macrophages that mediate the induction of transplantation tolerance remain elusive. Here, we demonstrate that costimulatory blockade favored accumulation of DC-SIGN-expressing macrophages that inhibited CD8(+) T cell immunity and promoted CD4(+)Foxp3(+) Treg cell expansion in numbers. Mechanistically, that simultaneous DC-SIGN engagement by fucosylated ligands and TLR4 signaling was required for production of immunoregulatory IL-10 associated with prolonged allograft survival. Deletion of DC-SIGN-expressing macrophages in vivo, interfering with their CSF1-dependent development, or preventing the DC-SIGN signaling pathway abrogated tolerance. Together, the results provide new insights into the tolerogenic effects of costimulatory blockade and identify DC-SIGN(+) suppressive macrophages as crucial mediators of immunological tolerance with the concomitant therapeutic implications in the clinic.
in vitro B cell stimulation/activation
Xu, H., et al. (2015). "Regulation of bifurcating B cell trajectories by mutual antagonism between transcription factors IRF4 and IRF8" Nat Immunol . PubMed
Upon recognition of antigen, B cells undertake a bifurcated response in which some cells rapidly differentiate into plasmablasts while others undergo affinity maturation in germinal centers (GCs). Here we identified a double-negative feedback loop between the transcription factors IRF4 and IRF8 that regulated the initial developmental bifurcation of activated B cells as well as the GC response. IRF8 dampened signaling via the B cell antigen receptor (BCR), facilitated antigen-specific interaction with helper T cells, and promoted antibody affinity maturation while antagonizing IRF4-driven differentiation of plasmablasts. Genomic analysis revealed concentration-dependent actions of IRF4 and IRF8 in regulating distinct gene-expression programs. Stochastic modeling suggested that the double-negative feedback was sufficient to initiate bifurcation of the B cell developmental trajectories.
in vivo CD40 activation
Bartkowiak, T., et al. (2015). "Unique potential of 4-1BB agonist antibody to promote durable regression of HPV+ tumors when combined with an E6/E7 peptide vaccine" Proc Natl Acad Sci U S A 112(38): E5290-5299. PubMed
Antibody modulation of T-cell coinhibitory (e.g., CTLA-4) or costimulatory (e.g., 4-1BB) receptors promotes clinical responses to a variety of cancers. Therapeutic cancer vaccination, in contrast, has produced limited clinical benefit and no curative therapies. The E6 and E7 oncoproteins of human papilloma virus (HPV) drive the majority of genital cancers, and many oropharyngeal tumors. We discovered 15-19 amino acid peptides from HPV-16 E6/E7 for which induction of T-cell immunity correlates with disease-free survival in patients treated for high-grade cervical neoplasia. We report here that intranasal vaccination with these peptides and the adjuvant alpha-galactosylceramide elicits systemic and mucosal T-cell responses leading to reduced HPV(+) TC-1 tumor growth and prolonged survival in mice. We hypothesized that the inability of these T cells to fully reject established tumors resulted from suppression in the tumor microenvironment which could be ameliorated through checkpoint modulation. Combining this E6/E7 peptide vaccine with checkpoint blockade produced only modest benefit; however, coadministration with a 4-1BB agonist antibody promoted durable regression of established genital TC-1 tumors. Relative to other therapies tested, this combination of vaccine and alpha4-1BB promoted the highest CD8(+) versus regulatory FoxP3(+) T-cell ratios, elicited 2- to 5-fold higher infiltration by E7-specific CTL, and evoked higher densities of highly cytotoxic TcEO (T cytotoxic Eomesodermin) CD8 (>70-fold) and ThEO (T helper Eomesodermin) CD4 (>17-fold) T cells. These findings have immediate clinical relevance both in terms of the direct clinical utility of the vaccine studied and in illustrating the potential of 4-1BB antibody to convert therapeutic E6/E7 vaccines already in clinical trials into curative therapies.
in vivo CD40 activation
Rabenstein, H., et al. (2014). "Differential kinetics of antigen dependency of CD4+ and CD8+ T cells" J Immunol 192(8): 3507-3517. PubMed
Ag recognition via the TCR is necessary for the expansion of specific T cells that then contribute to adaptive immunity as effector and memory cells. Because CD4+ and CD8+ T cells differ in terms of their priming APCs and MHC ligands we compared their requirements of Ag persistence during their expansion phase side by side. Proliferation and effector differentiation of TCR transgenic and polyclonal mouse T cells were thus analyzed after transient and continuous TCR signals. Following equally strong stimulation, CD4+ T cell proliferation depended on prolonged Ag presence, whereas CD8+ T cells were able to divide and differentiate into effector cells despite discontinued Ag presentation. CD4+ T cell proliferation was neither affected by Th lineage or memory differentiation nor blocked by coinhibitory signals or missing inflammatory stimuli. Continued CD8+ T cell proliferation was truly independent of self-peptide/MHC-derived signals. The subset divergence was also illustrated by surprisingly broad transcriptional differences supporting a stronger propensity of CD8+ T cells to programmed expansion. These T cell data indicate an intrinsic difference between CD4+ and CD8+ T cells regarding the processing of TCR signals for proliferation. We also found that the presentation of a MHC class II-restricted peptide is more efficiently prolonged by dendritic cell activation in vivo than a class I bound one. In summary, our data demonstrate that CD4+ T cells require continuous stimulation for clonal expansion, whereas CD8+ T cells can divide following a much shorter TCR signal.
in vitro B cell stimulation/activation
Muppidi, J. R., et al. (2014). "Loss of signalling via Galpha13 in germinal centre B-cell-derived lymphoma" Nature 516(7530): 254-258. PubMed
Germinal centre B-cell-like diffuse large B-cell lymphoma (GCB-DLBCL) is a common malignancy, yet the signalling pathways that are deregulated and the factors leading to its systemic dissemination are poorly defined. Work in mice showed that sphingosine-1-phosphate receptor-2 (S1PR2), a Galpha12 and Galpha13 coupled receptor, promotes growth regulation and local confinement of germinal centre B cells. Recent deep sequencing studies of GCB-DLBCL have revealed mutations in many genes in this cancer, including in GNA13 (encoding Galpha13) and S1PR2 (refs 5,6, 7). Here we show, using in vitro and in vivo assays, that GCB-DLBCL-associated mutations occurring in S1PR2 frequently disrupt the receptor’s Akt and migration inhibitory functions. Galpha13-deficient mouse germinal centre B cells and human GCB-DLBCL cells were unable to suppress pAkt and migration in response to S1P, and Galpha13-deficient mice developed germinal centre B-cell-derived lymphoma. Germinal centre B cells, unlike most lymphocytes, are tightly confined in lymphoid organs and do not recirculate. Remarkably, deficiency in Galpha13, but not S1PR2, led to germinal centre B-cell dissemination into lymph and blood. GCB-DLBCL cell lines frequently carried mutations in the Galpha13 effector ARHGEF1, and Arhgef1 deficiency also led to germinal centre B-cell dissemination. The incomplete phenocopy of Galpha13- and S1PR2 deficiency led us to discover that P2RY8, an orphan receptor that is mutated in GCB-DLBCL and another germinal centre B-cell-derived malignancy, Burkitt’s lymphoma, also represses germinal centre B-cell growth and promotes confinement via Galpha13. These findings identify a Galpha13-dependent pathway that exerts dual actions in suppressing growth and blocking dissemination of germinal centre B cells that is frequently disrupted in germinal centre B-cell-derived lymphoma.
in vivo CD40 activation
Erickson, J. J., et al. (2014). "Programmed death-1 impairs secondary effector lung CD8(+) T cells during respiratory virus reinfection" J Immunol 193(10): 5108-5117. PubMed
Reinfections with respiratory viruses are common and cause significant clinical illness, yet precise mechanisms governing this susceptibility are ill defined. Lung Ag-specific CD8(+) T cells (T(CD8)) are impaired during acute viral lower respiratory infection by the inhibitory receptor programmed death-1 (PD-1). To determine whether PD-1 contributes to recurrent infection, we first established a model of reinfection by challenging B cell-deficient mice with human metapneumovirus (HMPV) several weeks after primary infection, and found that HMPV replicated to high titers in the lungs. A robust secondary effector lung TCD8 response was generated during reinfection, but these cells were more impaired and more highly expressed the inhibitory receptors PD-1, LAG-3, and 2B4 than primary T(CD8). In vitro blockade demonstrated that PD-1 was the dominant inhibitory receptor early after reinfection. In vivo therapeutic PD-1 blockade during HMPV reinfection restored lung T(CD8) effector functions (i.e., degranulation and cytokine production) and enhanced viral clearance. PD-1 also limited the protective efficacy of HMPV epitope-specific peptide vaccination and impaired lung T(CD8) during heterotypic influenza virus challenge infection. Our results indicate that PD-1 signaling may contribute to respiratory virus reinfection and evasion of vaccine-elicited immune responses. These results have important implications for the design of effective vaccines against respiratory viruses.
in vivo CD40 activation
Hailemichael, Y., et al. (2013). "Persistent antigen at vaccination sites induces tumor-specific CD8(+) T cell sequestration, dysfunction and deletion" Nat Med 19(4): 465-472. PubMed
To understand why cancer vaccine-induced T cells often do not eradicate tumors, we studied immune responses in mice vaccinated with gp100 melanoma peptide in incomplete Freund’s adjuvant (peptide/IFA), which is commonly used in clinical cancer vaccine trials. Peptide/IFA vaccination primed tumor-specific CD8(+) T cells, which accumulated not in tumors but rather at the persisting, antigen-rich vaccination site. Once there, primed T cells became dysfunctional and underwent antigen-driven, interferon-gamma (IFN-gamma)- and Fas ligand (FasL)-mediated apoptosis, resulting in hyporesponsiveness to subsequent vaccination. Provision of CD40-specific antibody, Toll-like receptor 7 (TLR7) agonist and interleukin-2 (IL-2) reduced T cell apoptosis but did not prevent vaccination-site sequestration. A nonpersisting vaccine formulation shifted T cell localization toward tumors, inducing superior antitumor activity while reducing systemic T cell dysfunction and promoting memory formation. These data show that persisting vaccine depots can induce specific T cell sequestration, dysfunction and deletion at vaccination sites; short-lived formulations may overcome these limitations and result in greater therapeutic efficacy of peptide-based cancer vaccines.
in vivo CD40 activation
Locatelli, G., et al. (2012). "Primary oligodendrocyte death does not elicit anti-CNS immunity" Nat Neurosci 15(4): 543-550. PubMed
Anti-myelin immunity is commonly thought to drive multiple sclerosis, yet the initial trigger of this autoreactivity remains elusive. One of the proposed factors for initiating this disease is the primary death of oligodendrocytes. To specifically test such oligodendrocyte death as a trigger for anti-CNS immunity, we inducibly killed oligodendrocytes in an in vivo mouse model. Strong microglia-macrophage activation followed oligodendrocyte death, and myelin components in draining lymph nodes made CNS antigens available to lymphocytes. However, even conditions favoring autoimmunity-bystander activation, removal of regulatory T cells, presence of myelin-reactive T cells and application of demyelinating antibodies-did not result in the development of CNS inflammation after oligodendrocyte death. In addition, this lack of reactivity was not mediated by enhanced myelin-specific tolerance. Thus, in contrast with previously reported impairments of oligodendrocyte physiology, diffuse oligodendrocyte death alone or in conjunction with immune activation does not trigger anti-CNS immunity.
in vivo CD40 activation
Kurche, J. S., et al. (2012). "Type I IFN-dependent T cell activation is mediated by IFN-dependent dendritic cell OX40 ligand expression and is independent of T cell IFNR expression" J Immunol 188(2): 585-593. PubMed
Type I IFNs are important for direct control of viral infection and generation of adaptive immune responses. Recently, direct stimulation of CD4(+) T cells via type I IFNR has been shown to be necessary for the formation of functional CD4(+) T cell responses. In contrast, we find that CD4(+) T cells do not require intrinsic type I IFN signals in response to combined TLR/anti-CD40 vaccination. Rather, the CD4 response is dependent on the expression of type I IFNR (IFNalphaR) on innate cells. Further, we find that dendritic cell (DC) expression of the TNF superfamily member OX40 ligand was dependent on type I IFN signaling in the DC, resulting in a reduced CD4(+) T cell response that could be substantially rescued by an agonistic Ab to the receptor OX40. Taken together, we show that the IFNalphaR dependence of the CD4(+) T cell response is accounted for exclusively by defects in DC activation.
- Immunology and Microbiology,
Secreted IgM modulates IL-10 expression in B cells.
In Nature Communications on 5 January 2024 by McGettigan, S. E., Aira, L. E., et al.
PubMed
IL-10+ B cells are critical for immune homeostasis and restraining immune responses in infection, cancer, and inflammation; however, the signals that govern IL-10+ B cell differentiation are ill-defined. Here we find that IL-10+ B cells expand in mice lacking secreted IgM ((s)IgM-/-) up to 10-fold relative to wildtype (WT) among all major B cell and regulatory B cell subsets. The IL-10+ B cell increase is polyclonal and presents within 24 hours of birth. In WT mice, sIgM is produced prenatally and limits the expansion of IL-10+ B cells. Lack of the high affinity receptor for sIgM, FcμR, in B cells translates into an intermediate IL-10+ B cell phenotype relative to WT or sIgM-/- mice. Our study thus shows that sIgM regulates IL-10 programming in B cells in part via B cell-expressed FcμR, thereby revealing a function of sIgM in regulating immune homeostasis. © 2024. The Author(s).
- Cancer Research,
- Immunology and Microbiology
Antigen experience history directs distinct functional states of CD8+ CAR T cells during the anti-leukemia response
Preprint on Research Square on 21 December 2023 by Fry, T., DeGolier, K., et al.
PubMed
Chimeric antigen receptor T cells are an effective therapy for B-lineage malignancies. However, many patients relapse and this therapeutic has yet to show strong efficacy in other hematologic or solid tumors. One opportunity for improvement lies in the ability to generate T cells with desirable functional characteristics. Here, we dissect the biology of CD8+ CAR T cells (CAR8) by controlling whether the T cell has encountered cognate TCR antigen prior to CAR generation. We find that prior antigen experience influences multiple aspects of in vitro and in vivo CAR8 functionality, resulting in superior effector function and leukemia clearance in the setting of limiting target antigen density compared to antigen-inexperienced T cells. However, this comes at the expense of inferior proliferative capacity, susceptibility to phenotypic exhaustion and dysfunction, and inability to clear wildtype leukemia in the setting of limiting CAR+ cell dose. Epigenomic and transcriptomic comparisons of these cell populations identified overexpression of the Runx2 transcription factor as a novel strategy to enhance CAR8 function, with a differential impact depending on prior cell state. Collectively, our data demonstrate that prior antigen experience determines functional attributes of a CAR T cell, as well as amenability to functional enhancement by transcription factor modulation.
- Cancer Research,
- Immunology and Microbiology
Cancer cell plasticity and MHC-II-mediated immune tolerance promote breast cancer metastasis to lymph nodes.
In The Journal of Experimental Medicine on 4 September 2023 by Lei, P. J., Pereira, E. R., et al.
PubMed
Tumor-draining lymph nodes (TDLNs) are important for tumor antigen-specific T cell generation and effective anticancer immune responses. However, TDLNs are often the primary site of metastasis, causing immune suppression and worse outcomes. Through cross-species single-cell RNA-Seq analysis, we identified features defining cancer cell heterogeneity, plasticity, and immune evasion during breast cancer progression and lymph node metastasis (LNM). A subset of cancer cells in the lymph nodes exhibited elevated MHC class II (MHC-II) gene expression in both mice and humans. MHC-II+ cancer cells lacked costimulatory molecule expression, leading to regulatory T cell (Treg) expansion and fewer CD4+ effector T cells in TDLNs. Genetic knockout of MHC-II reduced LNM and Treg expansion, while overexpression of the MHC-II transactivator, Ciita, worsened LNM and caused excessive Treg expansion. These findings demonstrate that cancer cell MHC-II expression promotes metastasis and immune evasion in TDLNs. © 2023 Lei et al.
- Cancer Research,
- Genetics
Defining the spatial distribution of extracellular adenosine revealed a myeloid-dependent immunosuppressive microenvironment in pancreatic ductal adenocarcinoma.
In Journal for Immunotherapy of Cancer on 1 August 2023 by Graziano, V., Dannhorn, A., et al.
PubMed
The prognosis for patients with pancreatic ductal adenocarcinoma (PDAC) remains extremely poor. It has been suggested that the adenosine pathway contributes to the ability of PDAC to evade the immune system and hence, its resistance to immuno-oncology therapies (IOT), by generating extracellular adenosine (eAdo). Using genetically engineered allograft models of PDAC in syngeneic mice with defined and different immune infiltration and response to IOT and autochthonous tumors in KPC mice we investigated the impact of the adenosine pathway on the PDAC tumor microenvironment (TME). Flow cytometry and imaging mass cytometry (IMC) were used to characterize the subpopulation frequency and spatial distribution of tumor-infiltrating immune cells. Mass spectrometry imaging (MSI) was used to visualize adenosine compartmentalization in the PDAC tumors. RNA sequencing was used to evaluate the influence of the adenosine pathway on the shaping of the immune milieu and correlate our findings to published data sets in human PDAC. We demonstrated high expression of adenosine pathway components in tumor-infiltrating immune cells (particularly myeloid populations) in the murine models. MSI demonstrated that extracellular adenosine distribution is heterogeneous in tumors, with high concentrations in peri-necrotic, hypoxic regions, associated with rich myeloid infiltration, demonstrated using IMC. Protumorigenic M2 macrophages express high levels of the Adora2a receptor; particularly in the IOT resistant model. Blocking the in vivo formation and function of eAdo (Adoi), using a combination of anti-CD73 antibody and an Adora2a inhibitor slowed tumor growth and reduced metastatic burden. Additionally, blocking the adenosine pathway improved the efficacy of combinations of cytotoxic agents or immunotherapy. Adoi remodeled the TME, by reducing the infiltration of M2 macrophages and regulatory T cells. RNA sequencing analysis showed that genes related to immune modulation, hypoxia and tumor stroma were downregulated following Adoi and a specific adenosine signature derived from this is associated with a poorer prognosis in patients with PDAC. The formation of eAdo promotes the development of the immunosuppressive TME in PDAC, contributing to its resistance to conventional and novel therapies. Therefore, inhibition of the adenosine pathway may represent a strategy to modulate the PDAC immune milieu and improve therapy response in patients with PDAC. © Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY. Published by BMJ.
- WB,
- FC/FACS,
- Mus musculus (House mouse),
- Immunology and Microbiology
Deficiency of germinal center kinase TRAF2 and NCK-interacting kinase (TNIK) in B cells does not affect atherosclerosis.
In Frontiers in Cardiovascular Medicine on 22 May 2023 by van Os, B. W., Kusters, P. J. H., et al.
PubMed
Atherosclerosis is the underlying cause of many cardiovascular diseases, such as myocardial infarction or stroke. B cells, and their production of pro- and anti-atherogenic antibodies, play an important role in atherosclerosis. In B cells, TRAF2 and NCK-interacting Kinase (TNIK), a germinal center kinase, was shown to bind to TNF-receptor associated factor 6 (TRAF6), and to be involved in JNK and NF-κB signaling in human B cells, a pathway associated with antibody production. We here investigate the role of TNIK-deficient B cells in atherosclerosis. ApoE-/-TNIKfl/fl (TNIKBWT) and ApoE-/-TNIKfl/flCD19-cre (TNIKBKO) mice received a high cholesterol diet for 10 weeks. Atherosclerotic plaque area did not differ between TNIKBKO and TNIKBWT mice, nor was there any difference in plaque necrotic core, macrophage, T cell, α-SMA and collagen content. B1 and B2 cell numbers did not change in TNIKBKO mice, and marginal zone, follicular or germinal center B cells were unaffected. Total IgM and IgG levels, as well as oxidation specific epitope (OSE) IgM and IgG levels, did not change in absence of B cell TNIK. In contrast, plasma IgA levels were decreased in TNIKBKO mice, whereas the number of IgA+ B cells in intestinal Peyer's patches increased. No effects could be detected on T cell or myeloid cell numbers or subsets. We here conclude that in hyperlipidemic ApoE-/- mice, B cell specific TNIK deficiency does not affect atherosclerosis. © 2023 van Os, Kusters, den Toom, Beckers, van Tiel, Vos, de Jong, Kieser, van Roomen, Binder, Reiche, de Winther, Bosmans and Lutgens.
- Cancer Research,
- Immunology and Microbiology
Generation of B-cell-based cellular vaccine for cancer in murine models.
In STAR Protocols on 20 April 2023 by Hou, D., Katz, J. L., et al.
PubMed
A B-cell-based cellular vaccine (BVax), produced from 4-1BBL+ B cells, can select tumor-specific B cells that, upon ex vivo culture, can generate tumor-specific antibodies and activate T cells. Here, we present a protocol to generate a B-cell-based vaccine in a CT2A orthotopic glioma murine model. We describe steps for BVax production involving glioma cell implantation, tissue harvesting, 4-1BBL+ B cell isolation, and activation. We also describe assessing BVax phenotype in vitro and in vivo functional status. For complete details on the use and execution of this protocol, please refer to Lee-Chang et al. (2021).1. Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
A neutrophil response linked to tumor control in immunotherapy.
In Cell on 30 March 2023 by Gungabeesoon, J., Gort-Freitas, N. A., et al.
PubMed
Neutrophils accumulate in solid tumors, and their abundance correlates with poor prognosis. Neutrophils are not homogeneous, however, and could play different roles in cancer therapy. Here, we investigate the role of neutrophils in immunotherapy, leading to tumor control. We show that successful therapies acutely expanded tumor neutrophil numbers. This expansion could be attributed to a Sellhi state rather than to other neutrophils that accelerate tumor progression. Therapy-elicited neutrophils acquired an interferon gene signature, also seen in human patients, and appeared essential for successful therapy, as loss of the interferon-responsive transcription factor IRF1 in neutrophils led to failure of immunotherapy. The neutrophil response depended on key components of anti-tumor immunity, including BATF3-dependent DCs, IL-12, and IFNγ. In addition, we found that a therapy-elicited systemic neutrophil response positively correlated with disease outcome in lung cancer patients. Thus, we establish a crucial role of a neutrophil state in mediating effective cancer therapy. Copyright © 2023 Elsevier Inc. All rights reserved.
Thymus antibody-secreting cells possess an interferon gene signature and are preferentially expanded in young female mice.
In IScience on 17 March 2023 by Pioli, K. T., Lau, K. H., et al.
PubMed
Antibody-secreting cells (ASCs) are key contributors to humoral immunity through immunoglobulin production and the potential to be long-lived. ASC persistence has been recognized in the autoimmune thymus (THY); however, only recently has this population been appreciated in healthy THY tissue. We showed that the young female THY was skewed toward higher production of ASCs relative to males. However, these differences disappeared with age. In both sexes, THY ASCs included Ki-67+ plasmablasts which required CD154(CD40L) signals for their propagation. Single cell RNA-sequencing revealed that THY ASCs were enriched for an interferon responsive transcriptional signature relative to those from bone marrow and spleen. Flow cytometry confirmed that THY ASCs had increased levels of Toll-like receptor 7 as well as CD69 and major histocompatibility complex class II. Overall, we identified fundamental aspects of THY ASC biology which may be leveraged for future in depth studies of this population in both health and disease. © 2023 The Author(s).
- FC/FACS,
- Mus musculus (House mouse),
- Biochemistry and Molecular biology,
- Cell Biology,
- Immunology and Microbiology
Combination CTLA4Ig and Anti-CD40 Ligand Treatment Modifies T and B Cell Metabolic Profiles and Promotes B Cell Receptor Remodeling in a Mouse Model of Systemic Lupus Erythematosus.
In The Journal of Immunology on 1 March 2023 by Raparia, C., Quach, T. D., et al.
PubMed
Systemic lupus erythematosus is a complex autoimmune disease with significant morbidity that demands further examination of tolerance-inducing treatments. Short-term treatment of lupus-prone NZB/WF1 mice with combination CTLA4Ig and anti-CD40 ligand, but not single treatment alone, suppresses disease for >6 mo via modulation of B and T cell function while maintaining immune responses to exogenous Ags. Three months after a 2-wk course of combination costimulatory blockade, we found a modest decrease in the number of activated T and B cells in both combination and single-treatment cohorts compared with untreated controls. However, only combination treatment mice showed a 50% decrease in spare respiratory capacity of splenic B and T cells. RNA sequencing and gene set enrichment analysis of germinal center (GC) B cells confirmed a reduction in the oxidative phosphorylation signature in the combination treatment cohort. This cohort also manifested increased expression of BCR-associated signaling molecules and increased phosphorylation of PLCγ in GC B cells after stimulation with anti-IgG and anti-CD40. GC B cells from combination treatment mice also displayed a signature involving remodeling of GPI-linked surface proteins. Accordingly, we found a decrease in cell surface expression of the inhibitory molecule CD24 on class-switched memory B cells from aged NZB/W mice that corrected in the combination treatment cohort. Because both a profound decrease in BCR signaling and remodeled immune cell metabolism enhance loss of tolerance in lupus-prone mice, our findings help to explain the restoration of tolerance observed after short-term combination costimulatory blockade.Copyright © 2023 by The American Association of Immunologists, Inc.
- Biochemistry and Molecular biology,
- Cell Biology,
- Immunology and Microbiology
Orai3 and Orai1 mediate CRAC channel function and metabolic reprogramming in B cells.
In eLife on 21 February 2023 by Emrich, S. J., Yoast, R. E., et al.
PubMed
The essential role of store-operated Ca2+ entry (SOCE) through Ca2+ release-activated Ca2+ (CRAC) channels in T cells is well established. In contrast, the contribution of individual Orai isoforms to SOCE and their downstream signaling functions in B cells are poorly understood. Here, we demonstrate changes in the expression of Orai isoforms in response to B cell activation. We show that both Orai3 and Orai1 mediate native CRAC channels in B cells. The combined loss of Orai1 and Orai3, but not Orai3 alone, impairs SOCE, proliferation and survival, nuclear factor of activated T cells (NFAT) activation, mitochondrial respiration, glycolysis, and the metabolic reprogramming of primary B cells in response to antigenic stimulation. Nevertheless, the combined deletion of Orai1 and Orai3 in B cells did not compromise humoral immunity to influenza A virus infection in mice, suggesting that other in vivo co-stimulatory signals can overcome the requirement of BCR-mediated CRAC channel function in B cells. Our results shed important new light on the physiological roles of Orai1 and Orai3 proteins in SOCE and the effector functions of B lymphocytes. © 2023, Emrich et al.
- In Vivo,
- Mus musculus (House mouse),
- Cancer Research
Neutrophil-activating therapy for the treatment of cancer.
In Cancer Cell on 13 February 2023 by Linde, I. L., Prestwood, T. R., et al.
PubMed
Despite their cytotoxic capacity, neutrophils are often co-opted by cancers to promote immunosuppression, tumor growth, and metastasis. Consequently, these cells have received little attention as potential cancer immunotherapeutic agents. Here, we demonstrate in mouse models that neutrophils can be harnessed to induce eradication of tumors and reduce metastatic seeding through the combined actions of tumor necrosis factor, CD40 agonist, and tumor-binding antibody. The same combination activates human neutrophils in vitro, enabling their lysis of human tumor cells. Mechanistically, this therapy induces rapid mobilization and tumor infiltration of neutrophils along with complement activation in tumors. Complement component C5a activates neutrophils to produce leukotriene B4, which stimulates reactive oxygen species production via xanthine oxidase, resulting in oxidative damage and T cell-independent clearance of multiple tumor types. These data establish neutrophils as potent anti-tumor immune mediators and define an inflammatory pathway that can be harnessed to drive neutrophil-mediated eradication of cancer. Copyright © 2023 Elsevier Inc. All rights reserved.
- Cancer Research,
- Immunology and Microbiology
Breast cancer progression and metastasis to lymph nodes reveals cancer cell plasticity and MHC class II-mediated immune regulation
Preprint on BioRxiv : the Preprint Server for Biology on 1 November 2022 by Lei, P., Pereira, E. R., et al.
PubMed
Summary Tumor-draining lymph nodes are critical sites for generating tumor antigen-specific T cells and are associated with durable immune responses. However, lymph nodes are often the first site of metastasis and lymph node metastases portend worse outcomes. Through cross-species single cell gene expression analysis of breast cancer progression and metastasis to lymph nodes, we uncovered features that define the heterogeneity, plasticity, and immune evasion of cancer cells. Notably, a subpopulation of metastatic cancer cells in the lymph node were marked by high levels of MHC class II (MHC-II) gene expression both in mice and humans. Mechanistically, the IFN-γ and JAK/STAT signaling pathways mediate MHC-II expression in cancer cells. Ablation of IFNGR1/2 or CIITA, the transactivator of MHC-II, in cancer cells prevented tumor progression. Interestingly, MHC-II+ cancer cells lacked co-stimulatory molecule expression, engendered the expansion of regulatory T cells and blunted CD4+ effector T cells in the tumor-draining lymph nodes and favor tumor progression. Overall, our data suggests that cancer cell plasticity during breast cancer progression and metastasis to lymph nodes endows metastatic cells with the ability to avoid immune surveillance. These data provide the basis for new opportunities to therapeutically stimulate anti-cancer immune responses against local and systemic metastases.
- FC/FACS,
- Immunology and Microbiology
Mechanisms of CD40-dependent cDC1 licensing beyond costimulation.
In Nature Immunology on 1 November 2022 by Wu, R., Ohara, R. A., et al.
PubMed
CD40 signaling in classical type 1 dendritic cells (cDC1s) is required for CD8 T cell-mediated tumor rejection, but the underlying mechanisms are incompletely understood. Here, we identified CD40-induced genes in cDC1s, including Cd70, Tnfsf9, Ptgs2 and Bcl2l1, and examined their contributions to anti-tumor immunity. cDC1-specific inactivation of CD70 and COX-2, and global CD27 inactivation, only partially impaired tumor rejection or tumor-specific CD8 T cell expansion. Loss of 4-1BB, alone or in Cd27-/- mice, did not further impair anti-tumor immunity. However, cDC1-specific CD40 inactivation reduced cDC1 mitochondrial transmembrane potential and increased caspase activation in tumor-draining lymph nodes, reducing migratory cDC1 numbers in vivo. Similar impairments occurred during in vitro antigen presentation by Cd40-/- cDC1s to CD8+ T cells, which were reversed by re-expression of Bcl2l1. Thus, CD40 signaling in cDC1s not only induces costimulatory ligands for CD8+ T cells but also induces Bcl2l1 that sustains cDC1 survival during priming of anti-tumor responses. © 2022. The Author(s), under exclusive licence to Springer Nature America, Inc.
- Cancer Research
Platelets control liver tumor growth through P2Y12-dependent CD40L release in NAFLD.
In Cancer Cell on 12 September 2022 by Ma, C., Fu, Q., et al.
PubMed
Platelets, the often-overlooked component of the immune system, have been shown to promote tumor growth. Non-alcoholic fatty liver disease (NAFLD) is a common disease in the Western world and rising risk for hepatocellular carcinoma (HCC). Unexpectedly, we observed that platelets can inhibit the growth of established HCC in NAFLD mice. Through pharmacological inhibition and genetic depletion of P2Y12 as well as in vivo transfusion of wild-type (WT) or CD40L-/- platelets, we demonstrate that the anti-tumor function of platelets is mediated through P2Y12-dependent CD40L release, which leads to CD8+ T cell activation by the CD40 receptor. Unlike P2Y12 inhibition, blocking platelets with aspirin does not prevent platelet CD40L release nor accelerate HCC in NAFLD mice. Similar findings were observed in liver metastasis models. All together, our study reveals a complex role of platelets in tumor regulation. Anti-platelet treatment without inhibiting CD40L release could be considered for liver cancer patients with NAFLD. Published by Elsevier Inc.
- Immunology and Microbiology
T cell receptor β-chain-targeting chimeric antigen receptor T cells against T cell malignancies.
In Nature Communications on 26 July 2022 by Li, F., Zhang, H., et al.
PubMed
The success of chimeric antigen receptor (CAR) T cells in treating B cell malignancies comes at the price of eradicating normal B cells. Even though T cell malignancies are aggressive and treatment options are limited, similar strategies for T cell malignancies are constrained by the severe immune suppression arising from bystander T cell aplasia. Here, we show the selective killing of malignant T cells without affecting normal T cell-mediated immune responses in vitro and in a mouse model of disseminated leukemia. Further, we develop a CAR construct that carries the single chain variable fragment of a subtype-specific antibody against the variable TCR β-chain region. We demonstrate that these anti-Vβ8 CAR-T cells are able to recognize and kill all Vβ8+ malignant T cells that arise from clonal expansion while sparing malignant or healthy Vβ8- T cells, allowing sufficient T cell-mediated cellular immunity. In summary, we present a proof of concept for a selective CAR-T cell therapy to eradicate T cell malignancies while maintaining functional adaptive immunity, which opens the possibility for clinical development. © 2022. The Author(s).
- Cancer Research,
- Genetics
The heterogeneous distribution of extracellular adenosine reveals a myeloid-dependent axis, shaping the immunosuppressive microenvironment in pancreatic ductal adenocarcinoma
Preprint on BioRxiv : the Preprint Server for Biology on 25 May 2022 by Graziano, V., Dannhorn, A., et al.
PubMed
The prognosis for patients with pancreatic ductal adenocarcinoma (PDAC) remains extremely poor. It has been suggested that the adenosine pathway contributes to the ability of PDAC to evade the immune system and its resistance to immunotherapies (Immuno-Oncology Therapy, IOT), by generating extracellular adenosine (eAdo). Using syngeneic genetically engineered mouse allograft models of PDAC with differential immune infiltration and response to IOT, we showed enrichment of the adenosine pathway in tumour-infiltrating immune cells (in particular, myeloid populations). Extracellular adenosine distribution is heterogeneous in tumours, with high concentrations in hypoxic margins that surround necrotic areas, associated with a rich myeloid infiltration. Pro-tumorigenic M2 macrophages express high levels of the Adora2a receptor; particularly in the IOT resistant model. Blocking the in vivo formation and function of eAdo (Adoi), using a combination of anti-CD73 antibody and an Adora2a inhibitor slowed tumour growth and reduced metastatic burden. In addition, blocking the adenosine pathway improved the efficacy of combinations of cytotoxic agents or immunotherapy. Finally, Adoi remodelled the tumour microenvironment (TME), as evidenced by reduced infiltration of M2 macrophages and Tregs. RNAseq analysis showed that genes related to immune modulation, hypoxia and tumour stroma were downregulated following Adoi and a specific adenosine signature derived from this is associated with a poorer prognosis in PDAC patients. The formation of eAdo appears to promote the development of the immunosuppressive TME in PDAC, contributing to its resistance to conventional and novel therapies. Therefore, inhibition of the adenosine pathway may represent a strategy to modulate the stroma and improve therapy response in patients with PDAC.
- In Vivo,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology
Distinct myeloid antigen-presenting cells dictate differential fates of tumor-specific CD8+ T cells in pancreatic cancer.
In JCI Insight on 8 April 2022 by Burrack, A. L., Schmiechen, Z. C., et al.
PubMed
We investigate how myeloid subsets differentially shape immunity to pancreatic ductal adenocarcinoma (PDA). We show that tumor antigenicity sculpts myeloid cell composition and functionality. Antigenicity promotes accumulation of type 1 dendritic cells (cDC1), which is driven by Xcr1 signaling, and overcomes macrophage-mediated suppression. The therapeutic activity of adoptive T cell therapy or programmed cell death ligand 1 blockade required cDC1s, which sustained splenic Klrg1+ cytotoxic antitumor T cells and functional intratumoral T cells. KLRG1 and cDC1 genes correlated in human tumors, and PDA patients with high intratumoral KLRG1 survived longer than patients with low intratumoral KLRG1. The immunotherapy CD40 agonist also required host cDC1s for maximal therapeutic benefit. However, CD40 agonist exhibited partial therapeutic benefit in cDC1-deficient hosts and resulted in priming of tumor-specific yet atypical CD8+ T cells with a regulatory phenotype and that failed to participate in tumor control. Monocyte/macrophage depletion using clodronate liposomes abrogated T cell priming yet enhanced the antitumor activity of CD40 agonist in cDC1-deficient hosts via engagement of innate immunity. In sum, our study supports that cDC1s are essential for sustaining effective antitumor T cells and supports differential roles for cDC1s and monocytes/macrophages in instructing T cell fate and immunotherapy response.
- Immunology and Microbiology
Krüppel-like factor 2 controls IgA plasma cell compartmentalization and IgA responses.
In Mucosal Immunology on 1 April 2022 by Wittner, J., Schulz, S. R., et al.
PubMed
Krüppel-like factor 2 (KLF2) is a potent regulator of lymphocyte differentiation, activation and migration. However, its functional role in adaptive and humoral immunity remains elusive. Therefore, by using mice with a B cell-specific deletion of KLF2, we investigated plasma cell differentiation and antibody responses. We revealed that the deletion of KLF2 resulted in perturbed IgA plasma cell compartmentalization, characterized by the absence of IgA plasma cells in the bone marrow, their reductions in the spleen, the blood and the lamina propria of the colon and the small intestine, concomitant with their accumulation and retention in mesenteric lymph nodes and Peyer's patches. Most intriguingly, secretory IgA in the intestinal lumen was almost absent, dimeric serum IgA was drastically reduced and antigen-specific IgA responses to soluble Salmonella flagellin were blunted in KLF2-deficient mice. Perturbance of IgA plasma cell localization was caused by deregulation of CCR9, Integrin chains αM, α4, β7, and sphingosine-1-phosphate receptors. Hence, KLF2 not only orchestrates the localization of IgA plasma cells by fine-tuning chemokine receptors and adhesion molecules but also controls IgA responses to Salmonella flagellin. © 2022. The Author(s).
- Immunology and Microbiology
Intratumoral Recall of Childhood Vaccine-Specific CD4sup>+/sup> T cells Coordinates Type I and II Antitumor Immunity
Preprint on BioRxiv : the Preprint Server for Biology on 14 March 2022 by Brown, M. C., McKay, Z. P., et al.
PubMed
h4>ABSTRACT/h4> CD4 + T cells are key contributors to cancer immune surveillance. Here we report that childhood vaccine associated antigens engage simultaneous antitumor functions of CD8 + T cells and eosinophils via intratumor vaccine-specific CD4 + T cell recall. Prior vaccination against poliovirus potentiates antitumor efficacy of polio virotherapy in mice, and intratumor recall of poliovirus or tetanus immunity delayed tumor growth. Antitumor effects of recall antigens were mediated by CD4 + T cells, independent of CD40L signaling, and were dependent on eosinophils and CD8 + T cells. Recall antigen therapy caused marked tumor infiltration of type 2 innate lymphoid cells (ILC2s) expressing granzyme B and PD1 and eosinophils, coinciding with decreased proportions of intratumor Tregs. A pan-cancer analysis revealed an inverse relationship between intratumor eosinophils and Tregs, but not CD4 + or CD8 + T cells. This work defines cancer immunotherapy potential of childhood vaccines and implicates type II immunity in CD4 + T cell cancer immune surveillance.
- Mus musculus (House mouse)
Immuno-PET Imaging of Atherosclerotic Plaques with [89Zr]Zr-Anti-CD40 mAb-Proof of Concept.
In Biology on 6 March 2022 by Poels, K., Schreurs, M., et al.
PubMed
Non-invasive imaging of atherosclerosis can help in the identification of vulnerable plaque lesions. CD40 is a co-stimulatory molecule present on various immune and non-immune cells in the plaques and is linked to inflammation and plaque instability. We hypothesize that a 89Zr-labeled anti-CD40 monoclonal antibody (mAb) tracer has the potential to bind to cells present in atherosclerotic lesions and that CD40 Positron Emission Tomography (PET) can contribute to the detection of vulnerable atherosclerotic plaque lesions. To study this, wild-type (WT) and ApoE-/- mice were fed a high cholesterol diet for 14 weeks to develop atherosclerosis. Mice were injected with [89Zr]Zr-anti-CD40 mAb and the aortic uptake was evaluated and quantified using PET/Computed Tomography (CT) imaging. Ex vivo biodistribution was performed post-PET imaging and the uptake in the aorta was assessed with autoradiography and compared with Oil red O staining to determine the tracer potential to detect atherosclerotic plaques. On day 3 and 7 post injection, analysis of [89Zr]Zr-anti-CD40 mAb PET/CT scans showed a more pronounced aortic signal in ApoE-/- compared to WT mice with an increased aorta-to-blood uptake ratio. Autoradiography revealed [89Zr]Zr-anti-CD40 mAb uptake in atherosclerotic plaque areas in ApoE-/- mice, while no signal was found in WT mice. Clear overlap was observed between plaque areas as identified by Oil red O staining and autoradiography signal of [89Zr]Zr-anti-CD40 mAb in ApoE-/- mice. In this proof of concept study, we showed that PET/CT with [89Zr]Zr-anti-CD40 mAb can detect atherosclerotic plaques. As CD40 is associated with plaque vulnerability, [89Zr]Zr-anti-CD40 mAb has the potential to become a tracer to detect vulnerable atherosclerotic plaques.