InVivoMAb anti-mouse IL-2
Product Description
Specifications
| Isotype | Rat IgG2a |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 8.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse IL-2 |
| Reported Applications |
in vivo IL-2 neutralization in vivo IL-2 receptor stimulation (as a complex with IL-2) |
| Formulation |
PBS, pH 8.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo IL-2 neutralization
Baeyens, A., et al (2015). "Effector T cells boost regulatory T cell expansion by IL-2, TNF, OX40, and plasmacytoid dendritic cells depending on the immune context" J Immunol 194(3): 999-1010.
PubMed
CD4(+)CD25(+)Foxp3(+) regulatory T (Treg) cells play a major role in peripheral tolerance. Multiple environmental factors and cell types affect their biology. Among them, activated effector CD4(+) T cells can boost Treg cell expansion through TNF or IL-2. In this study, we further characterized this effector T (Teff) cell-dependent Treg cell boost in vivo in mice. This phenomenon was observed when both Treg and Teff cells were activated by their cognate Ag, with the latter being the same or different. Also, when Treg cells highly proliferated on their own, there was no additional Treg cell boost by Teff cells. In a condition of low inflammation, the Teff cell-mediated Treg cell boost involved TNF, OX40L, and plasmacytoid dendritic cells, whereas in a condition of high inflammation, it involved TNF and IL-2. Thus, this feedback mechanism in which Treg cells are highly activated by their Teff cell counterparts depends on the immune context for its effectiveness and mechanism. This Teff cell-dependent Treg cell boost may be crucial to limit inflammatory and autoimmune responses.
in vivo IL-2 neutralization
Clouthier, D. L., et al (2015). "GITR intrinsically sustains early type 1 and late follicular helper CD4 T cell accumulation to control a chronic viral infection" PLoS Pathog 11(1): e1004517.
PubMed
CD4 T cells are critical for control of persistent infections; however, the key signals that regulate CD4 T help during chronic infection remain incompletely defined. While several studies have addressed the role of inhibitory receptors and soluble factors such as PD-1 and IL-10, significantly less work has addressed the role of T cell co-stimulatory molecules during chronic viral infection. Here we show that during a persistent infection with lymphocytic choriomeningitis virus (LCMV) clone 13, mice lacking the glucocorticoid-induced tumor necrosis factor receptor related protein (GITR) exhibit defective CD8 T cell accumulation, increased T cell exhaustion and impaired viral control. Differences in CD8 T cells and viral control between GITR+/+ and GITR-/- mice were lost when CD4 T cells were depleted. Moreover, mixed bone marrow chimeric mice, as well as transfer of LCMV epitope-specific CD4 or CD8 T cells, demonstrated that these effects of GITR are largely CD4 T cell-intrinsic. GITR is dispensable for initial CD4 T cell proliferation and differentiation, but supports the post-priming accumulation of IFNgamma+IL-2+ Th1 cells, facilitating CD8 T cell expansion and early viral control. GITR-dependent phosphorylation of the p65 subunit of NF-kappaB as well as phosphorylation of the downstream mTORC1 target, S6 ribosomal protein, were detected at day three post-infection (p.i.), and defects in CD4 T cell accumulation in GITR-deficient T cells were apparent starting at day five p.i. Consistently, we pinpoint IL-2-dependent CD4 T cell help for CD8 T cells to between days four and eight p.i. GITR also increases the ratio of T follicular helper to T follicular regulatory cells and thereby enhances LCMV-specific IgG production. Together, these findings identify a CD4 T cell-intrinsic role for GITR in sustaining early CD8 and late humoral responses to collectively promote control of chronic LCMV clone 13 infection.
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Littwitz-Salomon, E., et al (2015). "Activated regulatory T cells suppress effector NK cell responses by an IL-2-mediated mechanism during an acute retroviral infection" Retrovirology 12: 66.
PubMed
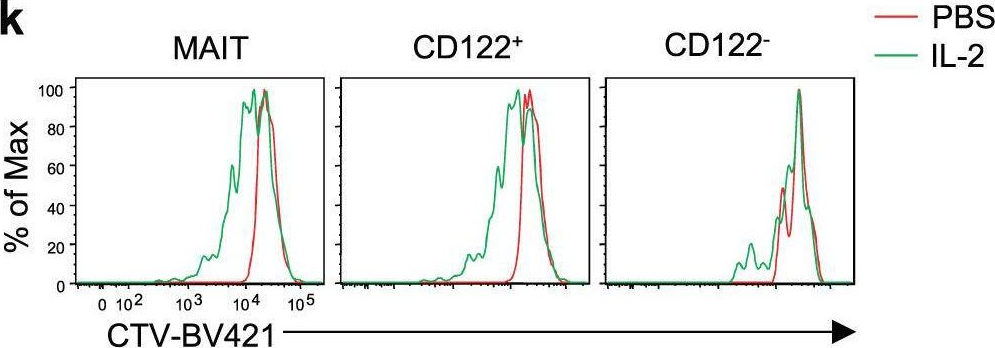
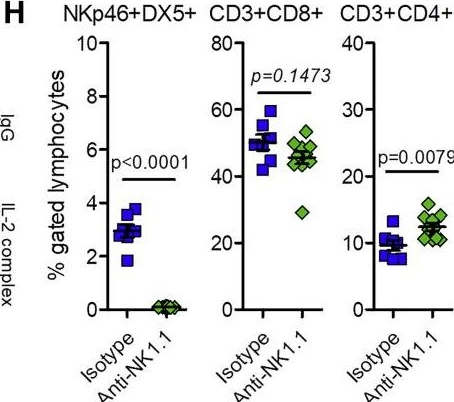
BACKGROUND: It is well established that effector T cell responses are crucial for the control of most virus infections, but they are often tightly controlled by regulatory T cells (Treg) to minimize immunopathology. NK cells also contribute to virus control but it is not known if their antiviral effect is influenced by virus-induced Tregs as well. We therefore analyzed whether antiretroviral NK cell functions are inhibited by Tregs during an acute Friend retrovirus infection of mice. RESULTS: Selective depletion of Tregs by using the transgenic DEREG mouse model resulted in improved NK cell proliferation, maturation and effector cell differentiation. Suppression of NK cell functions depended on IL-2 consumption by Tregs, which could be overcome by specific NK cell stimulation with an IL-2/anti-IL-2 mAb complex. CONCLUSIONS: The current study demonstrates that virus-induced Tregs indeed inhibit antiviral NK cell responses and describes a targeted immunotherapy that can abrogate the suppression of NK cells by Tregs.
in vivo IL-2 neutralization
in vivo IL-2 receptor stimulation (as a complex with IL-2)
McKinstry, K. K., et al (2014). "Effector CD4 T-cell transition to memory requires late cognate interactions that induce autocrine IL-2" Nat Commun 5: 5377.
PubMed
It is unclear how CD4 T-cell memory formation is regulated following pathogen challenge, and when critical mechanisms act to determine effector T-cell fate. Here, we report that following influenza infection most effectors require signals from major histocompatibility complex class II molecules and CD70 during a late window well after initial priming to become memory. During this timeframe, effector cells must produce IL-2 or be exposed to high levels of paracrine or exogenously added IL-2 to survive an otherwise rapid default contraction phase. Late IL-2 promotes survival through acute downregulation of apoptotic pathways in effector T cells and by permanently upregulating their IL-7 receptor expression, enabling IL-7 to sustain them as memory T cells. This new paradigm defines a late checkpoint during the effector phase at which cognate interactions direct CD4 T-cell memory generation.
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Mizui, M., et al (2014). "IL-2 protects lupus-prone mice from multiple end-organ damage by limiting CD4-CD8- IL-17-producing T cells" J Immunol 193(5): 2168-2177.
PubMed
IL-2, a cytokine with pleiotropic effects, is critical for immune cell activation and peripheral tolerance. Although the therapeutic potential of IL-2 has been previously suggested in autoimmune diseases, the mechanisms whereby IL-2 mitigates autoimmunity and prevents organ damage remain unclear. Using an inducible recombinant adeno-associated virus vector, we investigated the effect of low systemic levels of IL-2 in lupus-prone MRL/Fas(lpr/lpr) (MRL/lpr) mice. Treatment of mice after the onset of disease with IL-2-recombinant adeno-associated virus resulted in reduced mononuclear cell infiltration and pathology of various tissues, including skin, lungs, and kidneys. In parallel, we noted a significant decrease of IL-17-producing CD3(+)CD4(-)CD8(-) double-negative T cells and an increase in CD4(+)CD25(+)Foxp3(+) immunoregulatory T cells (Treg) in the periphery. We also show that IL-2 can drive double-negative (DN) T cell death through an indirect mechanism. Notably, targeted delivery of IL-2 to CD122(+) cytotoxic lymphocytes effectively reduced the number of DN T cells and lymphadenopathy, whereas selective expansion of Treg by IL-2 had no effect on DN T cells. Collectively, our data suggest that administration of IL-2 to lupus-prone mice protects against end-organ damage and suppresses inflammation by dually limiting IL-17-producing DN T cells and expanding Treg.
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Srivastava, S., et al (2014). "Type I interferons directly inhibit regulatory T cells to allow optimal antiviral T cell responses during acute LCMV infection" J Exp Med 211(5): 961-974.
PubMed
Regulatory T (T reg) cells play an essential role in preventing autoimmunity but can also impair clearance of foreign pathogens. Paradoxically, signals known to promote T reg cell function are abundant during infection and could inappropriately enhance T reg cell activity. How T reg cell function is restrained during infection to allow the generation of effective antiviral responses remains largely unclear. We demonstrate that the potent antiviral type I interferons (IFNs) directly inhibit co-stimulation-dependent T reg cell activation and proliferation, both in vitro and in vivo during acute infection with lymphocytic choriomeningitis virus (LCMV). Loss of the type I IFN receptor specifically in T reg cells results in functional impairment of virus-specific CD8(+) and CD4(+) T cells and inefficient viral clearance. Together, these data demonstrate that inhibition of T reg cells by IFNs is necessary for the generation of optimal antiviral T cell responses during acute LCMV infection.
in vivo IL-2 neutralization
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Gasteiger, G., et al (2013). "IL-2-dependent adaptive control of NK cell homeostasis" J Exp Med 210(6): 1179-1187.
PubMed
Activation and expansion of T and B lymphocytes and myeloid cells are controlled by Foxp3(+) regulatory T cells (T reg cells), and their deficiency results in a fatal lympho- and myeloproliferative syndrome. A role for T reg cells in the homeostasis of innate lymphocyte lineages remained unknown. Here, we report that T reg cells restrained the expansion of immature CD127(+) NK cells, which had the unique ability to up-regulate the IL2Ralpha (CD25) in response to the proinflammatory cytokine IL-12. In addition, we observed the preferential accumulation of CD127(+) NK cells in mice bearing progressing tumors or suffering from chronic viral infection. CD127(+) NK cells expanded in an IL-2-dependent manner upon T reg cell depletion and were able to give rise to mature NK cells, indicating that the latter can develop through a CD25(+) intermediate stage. Thus, T reg cells restrain the IL-2-dependent CD4(+) T cell help for CD127(+) immature NK cells. These findings highlight the adaptive control of innate lymphocyte homeostasis.
in vivo IL-2 neutralization
Gratz, I. K., et al (2013). "Cutting Edge: memory regulatory t cells require IL-7 and not IL-2 for their maintenance in peripheral tissues" J Immunol 190(9): 4483-4487.
PubMed
Thymic Foxp3-expressing regulatory T cells are activated by peripheral self-antigen to increase their suppressive function, and a fraction of these cells survive as memory regulatory T cells (mTregs). mTregs persist in nonlymphoid tissue after cessation of Ag expression and have enhanced capacity to suppress tissue-specific autoimmunity. In this study, we show that murine mTregs express specific effector memory T cell markers and localize preferentially to hair follicles in skin. Memory Tregs express high levels of both IL-2Ralpha and IL-7Ralpha. Using a genetic-deletion approach, we show that IL-2 is required to generate mTregs from naive CD4(+) T cell precursors in vivo. However, IL-2 is not required to maintain these cells in the skin and skin-draining lymph nodes. Conversely, IL-7 is essential for maintaining mTregs in skin in the steady state. These results elucidate the fundamental biology of mTregs and show that IL-7 plays an important role in their survival in skin.
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Smith, C., et al (2011). "Differential outcome of IL-2/anti-IL-2 complex therapy on effector and memory CD8+ T cells following vaccination with an adenoviral vector encoding EBV epitopes" J Immunol 186(10): 5784-5790.
PubMed
IL-2/anti-IL-2 complex-based therapy has been proposed as a potential adjunct therapeutic tool to enhance in vivo efficacy of T cell-based immunotherapeutic strategies for chronic viral infections and human cancers. In this study, we demonstrate that IL-2 complex therapy can have discerning effects on CD8(+) T cells depending on their stage of differentiation. To delineate the underlying mechanism for these opposing effects on CD8(+) T cells, we examined the effects of IL-2 therapy during early priming, effector, and memory phases of T cell responses generated following immunization with an adenoviral vector encoding multiple EBV CD8(+) epitopes. IL-2 complex treatment during the early priming phase, which coincided with low levels of IL-2Rbeta (CD122) and higher levels of IL-2Ralpha (CD25) on CD8(+) T cells, did not induce the expansion of effector T cells. In contrast, IL-2 complex treatment following the establishment of memory enhanced the expansion of Ag-specific T cells. Additionally, central memory T cells preferentially expanded following treatment at the expense of effector memory T cell populations. These studies demonstrate how differentiation status of the responding CD8(+) T cells impacts on their responsiveness to IL-2 complexes and highlight that timing of treatment should be considered before implementing this therapy in a clinical setting.
in vivo IL-2 receptor stimulation (as a complex with IL-2)
Hamilton, S. E., et al (2010). "IL-2 complex treatment can protect naive mice from bacterial and viral infection" J Immunol 185(11): 6584-6590.
PubMed
IL-2 complexes have substantial effects on the cellular immune system, and this approach is being explored for therapeutic application in infection and cancer. However, the impact of such treatments on subsequent encounter with pathogens has not been investigated. In this study, we report that naive mice treated with a short course of IL-2 complexes show enhanced protection from newly encountered bacterial and viral infections. IL-2 complex treatment expands both the NK and CD8 memory cell pool, including a recently described population of preexisting memory-phenotype T cells responsive to previously unencountered foreign Ags. Surprisingly, prolonged IL-2 complex treatment decreased CD8 T cell function and protective immunity. These data reveal the impact of cytokine complex treatment on the primary response to infection.
Product Citations
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
T-cell specific in vivo gene delivery with DART-AAVs targeted to CD8.
In Mol Ther on 2 October 2024 by Demircan, M. B., Zinser, L. J., et al.
PubMed
One of the biggest challenges for in vivo gene therapy are vectors mediating highly selective gene transfer into a defined population of therapy-relevant cells. Here we present DARPin-targeted AAVs (DART-AAVs) displaying DARPins specific for human and murine CD8. Insertion of DARPins into the GH2/GH3 loop of the capsid protein 1 (VP1) of AAV2 and AAV6 resulted in high selectivity for CD8-positive T cells with unimpaired gene delivery activity. Remarkably, the capsid core structure was unaltered with protruding DARPins detectable. In complex primary cell mixtures, including donor blood or systemic injections into mice, the CD8-targeted AAVs were by far superior to unmodified AAV2 and AAV6 in terms of selectivity, target cell viability, and gene transfer rates. In vivo, up to 80% of activated CD8+ T cells were hit upon a single vector injection into conditioned humanized or immunocompetent mice. While gene transfer rates decreased significantly under non-activated conditions, genomic modification selectively in CD8+ T cells was still detectable upon Cre delivery into indicator mice. In both mouse models, selectivity for CD8+ T cells was close to absolute with exceptional detargeting from liver. The CD8-AAVs described here expand strategies for immunological research and in vivo gene therapy options.
-
-
-
Immunology and Microbiology
-
Cancer Research
Interruption of the intratumor CD8+ T cell:Treg crosstalk improves the efficacy of PD-1 immunotherapy.
In Cancer Cell on 10 June 2024 by Geels, S. N., Moshensky, A., et al.
PubMed
PD-1 blockade unleashes potent antitumor activity in CD8+ T cells but can also promote immunosuppressive T regulatory (Treg) cells, which may worsen the response to immunotherapy. Tumor-Treg inhibition is a promising strategy to improve the efficacy of checkpoint blockade immunotherapy; however, our understanding of the mechanisms supporting tumor-Tregs during PD-1 immunotherapy is incomplete. Here, we show that PD-1 blockade increases tumor-Tregs in mouse models of melanoma and metastatic melanoma patients. Mechanistically, Treg accumulation is not caused by Treg-intrinsic inhibition of PD-1 signaling but depends on an indirect effect of activated CD8+ T cells. CD8+ T cells produce IL-2 and colocalize with Tregs in mouse and human melanomas. IL-2 upregulates the anti-apoptotic protein ICOS on tumor-Tregs, promoting their accumulation. Inhibition of ICOS signaling before PD-1 immunotherapy improves control over immunogenic melanoma. Thus, interrupting the intratumor CD8+ T cell:Treg crosstalk represents a strategy to enhance the therapeutic efficacy of PD-1 immunotherapy.
-
-
-
Immunology and Microbiology
-
Cancer Research
Spatial and functional targeting of intratumoral Tregs reverses CD8+ T cell exhaustion and promotes cancer immunotherapy.
In J Clin Invest on 23 May 2024 by Zhou, L., Velegraki, M., et al.
PubMed
Intratumoral Tregs are key mediators of cancer immunotherapy resistance, including anti-programmed cell death (ligand) 1 [anti-PD-(L)1] immune checkpoint blockade (ICB). The mechanisms driving Treg infiltration into the tumor microenvironment (TME) and the consequence on CD8+ T cell exhaustion remain elusive. Here, we report that heat shock protein gp96 (also known as GRP94) was indispensable for Treg tumor infiltration, primarily through the roles of gp96 in chaperoning integrins. Among various gp96-dependent integrins, we found that only LFA-1 (αL integrin), and not αV, CD103 (αE), or β7 integrin, was required for Treg tumor homing. Loss of Treg infiltration into the TME by genetic deletion of gp96/LFA-1 potently induced rejection of tumors in multiple ICB-resistant murine cancer models in a CD8+ T cell-dependent manner, without loss of self-tolerance. Moreover, gp96 deletion impeded Treg activation primarily by suppressing IL-2/STAT5 signaling, which also contributed to tumor regression. By competing for intratumoral IL-2, Tregs prevented the activation of CD8+ tumor-infiltrating lymphocytes, drove thymocyte selection-associated high mobility group box protein (TOX) induction, and induced bona fide CD8+ T cell exhaustion. By contrast, Treg ablation led to striking CD8+ T cell activation without TOX induction, demonstrating clear uncoupling of the 2 processes. Our study reveals that the gp96/LFA-1 axis plays a fundamental role in Treg biology and suggests that Treg-specific gp96/LFA-1 targeting represents a valuable strategy for cancer immunotherapy without inflicting autoinflammatory conditions.
-
-
-
Immunology and Microbiology
Activation of the aryl hydrocarbon receptor inhibits neuropilin-1 upregulation on IL-2-responding CD4+ T cells.
In Front Immunol on 30 November 2023 by Sandoval, S., Malany, K., et al.
PubMed
Neuropilin-1 (Nrp1), a transmembrane protein expressed on CD4+ T cells, is mostly studied in the context of regulatory T cell (Treg) function. More recently, there is increasing evidence that Nrp1 is also highly expressed on activated effector T cells and that increases in these Nrp1-expressing CD4+ T cells correspond with immunopathology across several T cell-dependent disease models. Thus, Nrp1 may be implicated in the identification and function of immunopathologic T cells. Nrp1 downregulation in CD4+ T cells is one of the strongest transcriptional changes in response to immunoregulatory compounds that act though the aryl hydrocarbon receptor (AhR), a ligand-activated transcription factor. To better understand the link between AhR and Nrp1 expression on CD4+ T cells, Nrp1 expression was assessed in vivo and in vitro following AhR ligand treatment. In the current study, we identified that the percentage of Nrp1 expressing CD4+ T cells increases over the course of activation and proliferation in vivo. The actively dividing Nrp1+Foxp3- cells express the classic effector phenotype of CD44hiCD45RBlo, and the increase in Nrp1+Foxp3- cells is prevented by AhR activation. In contrast, Nrp1 expression is not modulated by AhR activation in non-proliferating CD4+ T cells. The downregulation of Nrp1 on CD4+ T cells was recapitulated in vitro in cells isolated from C57BL/6 and NOD (non-obese diabetic) mice. CD4+Foxp3- cells expressing CD25, stimulated with IL-2, or differentiated into Th1 cells, were particularly sensitive to AhR-mediated inhibition of Nrp1 upregulation. IL-2 was necessary for AhR-dependent downregulation of Nrp1 expression both in vitro and in vivo. Collectively, the data demonstrate that Nrp1 is a CD4+ T cell activation marker and that regulation of Nrp1 could be a previously undescribed mechanism by which AhR ligands modulate effector CD4+ T cell responses.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Activation of the aryl hydrocarbon receptor inhibits neuropilin-1 upregulation on IL-2 responding CD4+T cells
In bioRxiv on 28 September 2023 by Sandoval, S., Malany, K., et al.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Robust IL-2-dependent antitumor immunotherapy requires targeting the high-affinity IL-2R on tumor-specific CD8+ T cells.
In J Immunother Cancer on 1 June 2023 by LaPorte, K. M., Hernandez, R., et al.
PubMed
Development of interleukin (IL)-2-dependent antitumor responses focus on targeting the intermediate affinity IL-2R to stimulate memory-phenotypic CD8+ T and natural killer (NK) cells while minimizing regulatory T cell (Treg) expansion. However, this approach may not effectively engage tumor-specific T effector cells. Since tumor-antigen specific T cells upregulate the high-affinity IL-2R, we tested an IL-2 biologic, mouse IL-2/CD25, with selectivity toward the high-affinity IL-2R to support antitumor responses to tumors that vary in their immunogenicity.
-
-
-
Immunology and Microbiology
Regulatory T cells suppress the formation of potent KLRK1 and IL-7R expressing effector CD8 T cells by limiting IL-2.
In Elife on 27 January 2023 by Tsyklauri, O., Chadimova, T., et al.
PubMed
Regulatory T cells (Tregs) are indispensable for maintaining self-tolerance by suppressing conventional T cells. On the other hand, Tregs promote tumor growth by inhibiting anticancer immunity. In this study, we identified that Tregs increase the quorum of self-reactive CD8+ T cells required for the induction of experimental autoimmune diabetes in mice. Their major suppression mechanism is limiting available IL-2, an essential T-cell cytokine. Specifically, Tregs inhibit the formation of a previously uncharacterized subset of antigen-stimulated KLRK1+ IL-7R+ (KILR) CD8+ effector T cells, which are distinct from conventional effector CD8+ T cells. KILR CD8+ T cells show superior cell-killing abilities in vivo. The administration of agonistic IL-2 immunocomplexes phenocopies the absence of Tregs, i.e., it induces KILR CD8+ T cells, promotes autoimmunity, and enhances antitumor responses in mice. Counterparts of KILR CD8+ T cells were found in the human blood, revealing them as a potential target for immunotherapy.
-
-
-
Cancer Research
-
Immunology and Microbiology
Tumor suppressor immune gene therapy to reverse immunotherapy resistance.
In Cancer Gene Ther on 1 June 2022 by Chada, S., Wiederhold, D., et al.
PubMed
While immune checkpoint inhibitors are becoming a standard of care for multiple types of cancer, the majority of patients do not respond to this form of immunotherapy. New approaches are required to overcome resistance to immunotherapies.
-
-
-
Immunology and Microbiology
Beneficial Effects of Celastrol on Immune Balance by Modulating Gut Microbiota in Experimental Ulcerative Colitis Mice.
In Genomics Proteomics Bioinformatics on 1 April 2022 by Li, M., Guo, W., et al.
PubMed
Ulcerative colitis (UC) is a chronic inflammatory bowel disease caused by many factors including colonic inflammation and microbiota dysbiosis. Previous studies have indicated that celastrol (CSR) has strong anti-inflammatory and immune-inhibitory effects. Here, we investigated the effects of CSR on colonic inflammation and mucosal immunity in an experimental colitis model, and addressed the mechanism by which CSR exerts the protective effects. We characterized the therapeutic effects and the potential mechanism of CSR on treating UC using histological staining, intestinal permeability assay, cytokine assay, flow cytometry, fecal microbiota transplantation (FMT), 16S rRNA sequencing, untargeted metabolomics, and cell differentiation. CSR administration significantly ameliorated the dextran sodium sulfate (DSS)-induced colitis in mice, which was evidenced by the recovered body weight and colon length as well as the decreased disease activity index (DAI) score and intestinal permeability. Meanwhile, CSR down-regulated the production of pro-inflammatory cytokines and up-regulated the amount of anti-inflammatory mediators at both mRNA and protein levels, and improved the balances of Treg/Th1 and Treg/Th17 to maintain the colonic immune homeostasis. Notably, all the therapeutic effects were exerted in a gut microbiota-dependent manner. Furthermore, CSR treatment increased the gut microbiota diversity and changed the compositions of the gut microbiota and metabolites, which is probably associated with the gut microbiota-mediated protective effects. In conclusion, this study provides the strong evidence that CSR may be a promising therapeutic drug for UC.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
IL-2/JES6-1 mAb complexes dramatically increase sensitivity to LPS through IFN-γ production by CD25+Foxp3- T cells.
In Elife on 21 December 2021 by Tomala, J., Weberova, P., et al.
PubMed
Complexes of IL-2 and JES6-1 mAb (IL-2/JES6) provide strong sustained IL-2 signal selective for CD25+ cells and thus they potently expand Treg cells. IL-2/JES6 are effective in the treatment of autoimmune diseases and in protecting against rejection of pancreatic islet allografts. However, we found that IL-2/JES6 also dramatically increase sensitivity to LPS-mediated shock in C57BL/6 mice. We demonstrate here that this phenomenon is dependent on endogenous IFN-γ and T cells, as it is not manifested in IFN-γ deficient and nude mice, respectively. Administration of IL-2/JES6 leads to the emergence of CD25+Foxp3-CD4+ and CD25+Foxp3-CD8+ T cells producing IFN-γ in various organs, particularly in the liver. IL-2/JES6 also increase counts of CD11b+CD14+ cells in the blood and the spleen with higher sensitivity to LPS in terms of TNF-α production and induce expression of CD25 in these cells. These findings indicate safety issue for potential use of IL-2/JES6 or similar IL-2-like immunotherapeutics.
-
-
-
Immunology and Microbiology
Regulatory T cells suppress the formation of potent KLRK1 and IL-7R expressing effector CD8 T cells by limiting IL-2
In bioRxiv on 12 November 2021 by Tsyklauri, O., Chadimova, T., et al.
-
-
-
Mus musculus (Mouse)
-
Biochemistry and Molecular biology
-
Cell Biology
-
Immunology and Microbiology
-
Neuroscience
PI3Kδ coordinates transcriptional, chromatin, and metabolic changes to promote effector CD8+ T cells at the expense of central memory.
In Cell Rep on 12 October 2021 by Cannons, J. L., Villarino, A. V., et al.
PubMed
Patients with activated phosphatidylinositol 3-kinase delta (PI3Kδ) syndrome (APDS) present with sinopulmonary infections, lymphadenopathy, and cytomegalvirus (CMV) and/or Epstein-Barr virus (EBV) viremia, yet why patients fail to clear certain chronic viral infections remains incompletely understood. Using patient samples and a mouse model (Pik3cdE1020K/+ mice), we demonstrate that, upon activation, Pik3cdE1020K/+ CD8+ T cells exhibit exaggerated features of effector populations both in vitro and after viral infection that are associated with increased Fas-mediated apoptosis due to sustained FoxO1 phosphorylation and Fasl derepression, enhanced mTORC1 and c-Myc signatures, metabolic perturbations, and an altered chromatin landscape. Conversely, Pik3cdE1020K/+ CD8+ cells fail to sustain expression of proteins critical for central memory, including TCF1. Strikingly, activated Pik3cdE1020K/+ CD8+ cells exhibit altered transcriptional and epigenetic circuits characterized by pronounced interleukin-2 (IL-2)/STAT5 signatures and heightened IL-2 responses that prevent differentiation to memory-like cells in IL-15. Our data position PI3Kδ as integrating multiple signaling nodes that promote CD8+ T cell effector differentiation, providing insight into phenotypes of patients with APDS.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Beneficial Effects of Celastrol on Immune Balance by Modulating Gut Microbiota in Dextran Sodium Sulfate-Induced Ulcerative Colitis
In bioRxiv on 28 September 2021 by Li, M., Guo, W., et al.
-
-
Delivery of membrane impermeable molecules to primary mouse T lymphocytes.
In STAR Protoc on 17 September 2021 by Xu, K., Li, M. O., et al.
PubMed
The pore-forming toxin streptolysin-O (SLO) enables intracellular delivery of molecules up to 100 kDa and has been used for short-term delivery of membrane-impermeable substances to assess their effects on cellular activities. A limitation of this technique is the loss of intracellular components and the potential unpredicted alterations of cellular metabolism and signaling. This protocol, optimized for primary mouse T lymphocytes, describes steps for SLO-mediated cell membrane permeabilization and substance supplementation, followed by immunoblotting and immunofluorescent microscopy for assessing cellular effects. For complete details on the use and execution of this protocol, please refer to Xu et al., 2021a, Xu et al., 2021b.
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
-
In vivo experiments
Identification of a Kupffer cell subset capable of reverting the T cell dysfunction induced by hepatocellular priming.
In Immunity on 14 September 2021 by De Simone, G., Andreata, F., et al.
PubMed
Kupffer cells (KCs) are highly abundant, intravascular, liver-resident macrophages known for their scavenger and phagocytic functions. KCs can also present antigens to CD8+ T cells and promote either tolerance or effector differentiation, but the mechanisms underlying these discrepant outcomes are poorly understood. Here, we used a mouse model of hepatitis B virus (HBV) infection, in which HBV-specific naive CD8+ T cells recognizing hepatocellular antigens are driven into a state of immune dysfunction, to identify a subset of KCs (referred to as KC2) that cross-presents hepatocellular antigens upon interleukin-2 (IL-2) administration, thus improving the antiviral function of T cells. Removing MHC-I from all KCs, including KC2, or selectively depleting KC2 impaired the capacity of IL-2 to revert the T cell dysfunction induced by intrahepatic priming. In summary, by sensing IL-2 and cross-presenting hepatocellular antigens, KC2 overcome the tolerogenic potential of the hepatic microenvironment, suggesting new strategies for boosting hepatic T cell immunity.
-
-
-
Immunology and Microbiology
Foxp3 enhancers synergize to maximize regulatory T cell suppressive capacity.
In J Exp Med on 2 August 2021 by Zong, X., Hao, X., et al.
PubMed
T reg cells bearing a diverse antigen receptor repertoire suppress pathogenic T cells and maintain immune homeostasis during their long lifespan. How their robust function is determined genetically remains elusive. Here, we investigate the regulatory space of the cis-regulatory elements of T reg lineage-specifying factor Foxp3. Foxp3 enhancers are known as distinct readers of environmental cues controlling T reg cell induction or lineage stability. However, their single deficiencies cause mild, if any, immune dysregulation, leaving the key transcriptional mechanisms determining Foxp3 expression and thereby T reg cell suppressive capacity uncertain. We examined the collective activities of Foxp3 enhancers and found that they coordinate to maximize T reg cell induction, Foxp3 expression level, or lineage stability through distinct modes and that ablation of synergistic enhancers leads to lethal autoimmunity in young mice. Thus, the induction and maintenance of a diverse, stable T reg cell repertoire rely on combinatorial Foxp3 enhancers, suggesting broad, stage-specific, synergistic activities of cell-intrinsic factors and cell-extrinsic cues in determining T reg cell suppressive capacity.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Immunology and Microbiology
Expansion of tumor-associated Treg cells upon disruption of a CTLA-4-dependent feedback loop.
In Cell on 22 July 2021 by Marangoni, F., Zhakyp, A., et al.
PubMed
Foxp3+ T regulatory (Treg) cells promote immunological tumor tolerance, but how their immune-suppressive function is regulated in the tumor microenvironment (TME) remains unknown. Here, we used intravital microscopy to characterize the cellular interactions that provide tumor-infiltrating Treg cells with critical activation signals. We found that the polyclonal Treg cell repertoire is pre-enriched to recognize antigens presented by tumor-associated conventional dendritic cells (cDCs). Unstable cDC contacts sufficed to sustain Treg cell function, whereas T helper cells were activated during stable interactions. Contact instability resulted from CTLA-4-dependent downregulation of co-stimulatory B7-family proteins on cDCs, mediated by Treg cells themselves. CTLA-4-blockade triggered CD28-dependent Treg cell hyper-proliferation in the TME, and concomitant Treg cell inactivation was required to achieve tumor rejection. Therefore, Treg cells self-regulate through a CTLA-4- and CD28-dependent feedback loop that adjusts their population size to the amount of local co-stimulation. Its disruption through CTLA-4-blockade may off-set therapeutic benefits in cancer patients.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Glycolytic ATP fuels phosphoinositide 3-kinase signaling to support effector T helper 17 cell responses.
In Immunity on 11 May 2021 by Xu, K., Yin, N., et al.
PubMed
Aerobic glycolysis-the Warburg effect-converts glucose to lactate via the enzyme lactate dehydrogenase A (LDHA) and is a metabolic feature of effector T cells. Cells generate ATP through various mechanisms and Warburg metabolism is comparatively an energy-inefficient glucose catabolism pathway. Here, we examined the effect of ATP generated via aerobic glycolysis in antigen-driven T cell responses. Cd4CreLdhafl/fl mice were resistant to Th17-cell-mediated experimental autoimmune encephalomyelitis and exhibited defective T cell activation, migration, proliferation, and differentiation. LDHA deficiency crippled cellular redox balance and inhibited ATP production, diminishing PI3K-dependent activation of Akt kinase and thereby phosphorylation-mediated inhibition of Foxo1, a transcriptional repressor of T cell activation programs. Th17-cell-specific expression of an Akt-insensitive Foxo1 recapitulated the defects seen in Cd4CreLdhafl/fl mice. Induction of LDHA required PI3K signaling and LDHA deficiency impaired PI3K-catalyzed PIP3 generation. Thus, Warburg metabolism augments glycolytic ATP production, fueling a PI3K-centered positive feedback regulatory circuit that drives effector T cell responses.
-
-
-
In vivo experiments
-
Homo sapiens (Human)
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
A distal Foxp3 enhancer enables interleukin-2 dependent thymic Treg cell lineage commitment for robust immune tolerance.
In Immunity on 11 May 2021 by Dikiy, S., Li, J., et al.
PubMed
Activation of the STAT5 transcription factor downstream of the Interleukin-2 receptor (IL-2R) induces expression of Foxp3, a critical step in the differentiation of regulatory T (Treg) cells. Due to the pleiotropic effects of IL-2R signaling, it is unclear how STAT5 acts directly on the Foxp3 locus to promote its expression. Here, we report that IL-2 - STAT5 signaling converged on an enhancer (CNS0) during Foxp3 induction. CNS0 facilitated the IL-2 dependent CD25+Foxp3- precursor to Treg cell transition in the thymus. Its deficiency resulted in impaired Treg cell generation in neonates, which was partially mitigated with age. While the thymic Treg cell paucity caused by CNS0 deficiency did not result in autoimmunity on its own, it exacerbated autoimmune manifestations caused by disruption of the Aire gene. Thus, CNS0 enhancer activity ensures robust Treg cell differentiation early in postnatal life and cooperatively with other tolerance mechanisms minimizes autoimmunity.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
CD8+ T cell self-tolerance permits responsiveness but limits tissue damage.
In Elife on 30 April 2021 by Truckenbrod, E. N., Burrack, K. S., et al.
PubMed
Self-specific CD8+T cells can escape clonal deletion, but the properties and capabilities of such cells in a physiological setting are unclear. We characterized polyclonal CD8+ T cells specific for the melanocyte antigen tyrosinase-related protein 2 (Trp2) in mice expressing or lacking this enzyme (due to deficiency in Dct, which encodes Trp2). Phenotypic and gene expression profiles of pre-immune Trp2/Kb-specific cells were similar; the size of this population was only slightly reduced in wild-type (WT) compared to Dct-deficient (Dct-/-) mice. Despite comparable initial responses to Trp2 immunization, WT Trp2/Kb-specific cells showed blunted expansion and less readily differentiated into a CD25+proliferative population. Functional self-tolerance clearly emerged when assessing immunopathology: adoptively transferred WT Trp2/Kb-specific cells mediated vitiligo much less efficiently. Hence, CD8+ T cell self-specificity is poorly predicted by precursor frequency, phenotype, or even initial responsiveness, while deficient activation-induced CD25 expression and other gene expression characteristics may help to identify functionally tolerant cells.
-