InVivoMAb anti-mouse IL-10R (CD210)
Product Description
Bio X Cell is pleased to offer two recombinant, murine chimeric versions of the original 1B1.3A antibody, 1B1.3A-CP060 and 1B1.3A-CP073. The variable region sequences are identical to the original 1B1.3A but the constant region sequences have been switched from Rat IgG1, κ to mouse IgG2a, κ for use in murine models. Species-matched chimeric antibodies exhibit regulated effector functions—including Fc receptor binding and complement activation—and cause less immunogenicity and formation of anti-drug antibodies (ADAs) than xenogenic antibodies in animal models. Additionally, 1B1.3A-CP073 contains LALA-PG Fc-silencing mutations in the heavy chain rendering it unable to bind endogenous murine FcγR or C1q to induce antibody-dependent, cell-mediated cytotoxicity (ADCC) or complement-dependent cytotoxicity (CDC). Antibodies with active Fc regions can engage immune cells via FcγRs, leading to the depletion of antigen expressing cells through mechanisms like ADCC or complement activation. Fc-silenced antibodies do not trigger these pathways and can block signaling without killing or depleting target cells. The highly controlled sequence and lack of genetic drift in recombinant antibodies provide more reliable and reproducible results over hybridoma derived antibodies.
Specifications
| Isotype | Rat IgG1, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG1 isotype control, anti-horseradish peroxidase |
| Recommended Dilution Buffer | InVivoPure pH 6.5T Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant ligand-binding domain of mouse IL-10R |
| Reported Applications |
in vivo blocking of IL-10/IL-10R signaling in vitro blocking of IL-10R signaling Flow cytometry Western Blot |
| Formulation |
PBS, pH 6.5 0.01% Tween Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
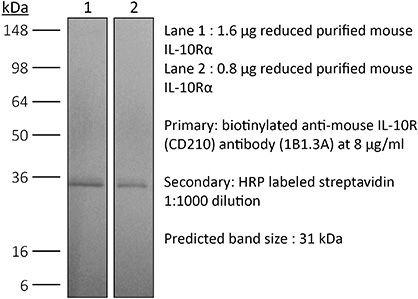
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_1107611 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo blocking of IL-10/IL-10R signaling
Burrack, K. S., et al (2018). "Interleukin-15 Complex Treatment Protects Mice from Cerebral Malaria by Inducing Interleukin-10-Producing Natural Killer Cells" Immunity 48(4): 760-772 e764.
PubMed
Cerebral malaria is a deadly complication of Plasmodium infection and involves blood brain barrier (BBB) disruption following infiltration of white blood cells. During experimental cerebral malaria (ECM), mice inoculated with Plasmodium berghei ANKA-infected red blood cells develop a fatal CM-like disease caused by CD8(+) T cell-mediated pathology. We found that treatment with interleukin-15 complex (IL-15C) prevented ECM, whereas IL-2C treatment had no effect. IL-15C-expanded natural killer (NK) cells were necessary and sufficient for protection against ECM. IL-15C treatment also decreased CD8(+) T cell activation in the brain and prevented BBB breakdown without influencing parasite load. IL-15C induced NK cells to express IL-10, which was required for IL-15C-mediated protection against ECM. Finally, we show that ALT-803, a modified human IL-15C, mediates similar induction of IL-10 in NK cells and protection against ECM. These data identify a regulatory role for cytokine-stimulated NK cells in the prevention of a pathogenic immune response.
in vivo blocking of IL-10/IL-10R signaling
Sun, M., et al (2018). "Microbiota-derived short-chain fatty acids promote Th1 cell IL-10 production to maintain intestinal homeostasis" Nat Commun 9(1): 3555.
PubMed
T-cells are crucial in maintanence of intestinal homeostasis, however, it is still unclear how microbiota metabolites regulate T-effector cells. Here we show gut microbiota-derived short-chain fatty acids (SCFAs) promote microbiota antigen-specific Th1 cell IL-10 production, mediated by G-protein coupled receptors 43 (GPR43). Microbiota antigen-specific Gpr43(-/-) CBir1 transgenic (Tg) Th1 cells, specific for microbiota antigen CBir1 flagellin, induce more severe colitis compared with wide type (WT) CBir1 Tg Th1 cells in Rag(-/-) recipient mice. Treatment with SCFAs limits colitis induction by promoting IL-10 production, and administration of anti-IL-10R antibody promotes colitis development. Mechanistically, SCFAs activate Th1 cell STAT3 and mTOR, and consequently upregulate transcription factor B lymphocyte-induced maturation protein 1 (Blimp-1), which mediates SCFA-induction of IL-10. SCFA-treated Blimp1(-/-) Th1 cells produce less IL-10 and induce more severe colitis compared to SCFA-treated WT Th1 cells. Our studies, thus, provide insight into how microbiota metabolites regulate Th1 cell functions to maintain intestinal homeostasis.
in vivo blocking of IL-10/IL-10R signaling
Xu, M., et al (2018). "c-MAF-dependent regulatory T cells mediate immunological tolerance to a gut pathobiont" Nature 554(7692): 373-377.
PubMed
Both microbial and host genetic factors contribute to the pathogenesis of autoimmune diseases. There is accumulating evidence that microbial species that potentiate chronic inflammation, as in inflammatory bowel disease, often also colonize healthy individuals. These microorganisms, including the Helicobacter species, can induce pathogenic T cells and are collectively referred to as pathobionts. However, how such T cells are constrained in healthy individuals is not yet understood. Here we report that host tolerance to a potentially pathogenic bacterium, Helicobacter hepaticus, is mediated by the induction of RORgammat(+)FOXP3(+) regulatory T (iTreg) cells that selectively restrain pro-inflammatory T helper 17 (TH17) cells and whose function is dependent on the transcription factor c-MAF. Whereas colonization of wild-type mice by H. hepaticus promoted differentiation of RORgammat-expressing microorganism-specific iTreg cells in the large intestine, in disease-susceptible IL-10-deficient mice, there was instead expansion of colitogenic TH17 cells. Inactivation of c-MAF in the Treg cell compartment impaired differentiation and function, including IL-10 production, of bacteria-specific iTreg cells, and resulted in the accumulation of H. hepaticus-specific inflammatory TH17 cells and spontaneous colitis. By contrast, RORgammat inactivation in Treg cells had only a minor effect on the bacteria-specific Treg and TH17 cell balance, and did not result in inflammation. Our results suggest that pathobiont-dependent inflammatory bowel disease is driven by microbiota-reactive T cells that have escaped this c-MAF-dependent mechanism of iTreg-TH17 homeostasis.
in vivo blocking of IL-10/IL-10R signaling
Christensen, A. D., et al (2015). "Depletion of regulatory T cells in a hapten-induced inflammation model results in prolonged and increased inflammation driven by T cells" Clin Exp Immunol 179(3): 485-499.
PubMed
Regulatory T cells (Tregs ) are known to play an immunosuppressive role in the response of contact hypersensitivity (CHS), but neither the dynamics of Tregs during the CHS response nor the exaggerated inflammatory response after depletion of Tregs has been characterized in detail. In this study we show that the number of Tregs in the challenged tissue peak at the same time as the ear-swelling reaches its maximum on day 1 after challenge, whereas the number of Tregs in the draining lymph nodes peaks at day 2. As expected, depletion of Tregs by injection of a monoclonal antibody to CD25 prior to sensitization led to a prolonged and sustained inflammatory response which was dependent upon CD8 T cells, and co-stimulatory blockade with cytotoxic T lymphocyte antigen-4-immunoglobulin (CTLA-4-Ig) suppressed the exaggerated inflammation. In contrast, blockade of the interleukin (IL)-10-receptor (IL-10R) did not further increase the exaggerated inflammatory response in the Treg -depleted mice. In the absence of Tregs , the response changed from a mainly acute reaction with heavy infiltration of neutrophils to a sustained response with more chronic characteristics (fewer neutrophils and dominated by macrophages). Furthermore, depletion of Tregs enhanced the release of cytokines and chemokines locally in the inflamed ear and augmented serum levels of the systemic inflammatory mediators serum amyloid (SAP) and haptoglobin early in the response.
in vivo blocking of IL-10/IL-10R signaling
Liu, G., et al (2015). "IL-27 Signaling Is Crucial for Survival of Mice Infected with African Trypanosomes via Preventing Lethal Effects of CD4+ T Cells and IFN-gamma" PLoS Pathog 11(7): e1005065.
PubMed
African trypanosomes are extracellular protozoan parasites causing a chronic debilitating disease associated with a persistent inflammatory response. Maintaining the balance of the inflammatory response via downregulation of activation of M1-type myeloid cells was previously shown to be crucial to allow prolonged survival. Here we demonstrate that infection with African trypanosomes of IL-27 receptor-deficient (IL-27R-/-) mice results in severe liver immunopathology and dramatically reduced survival as compared to wild-type mice. This coincides with the development of an exacerbated Th1-mediated immune response with overactivation of CD4+ T cells and strongly enhanced production of inflammatory cytokines including IFN-gamma. What is important is that IL-10 production was not impaired in infected IL-27R-/- mice. Depletion of CD4+ T cells in infected IL-27R-/- mice resulted in a dramatically reduced production of IFN-gamma, preventing the early mortality of infected IL-27R-/- mice. This was accompanied by a significantly reduced inflammatory response and a major amelioration of liver pathology. These results could be mimicked by treating IL-27R-/- mice with a neutralizing anti-IFN-gamma antibody. Thus, our data identify IL-27 signaling as a novel pathway to prevent early mortality via inhibiting hyperactivation of CD4+ Th1 cells and their excessive secretion of IFN-gamma during infection with African trypanosomes. These data are the first to demonstrate the essential role of IL-27 signaling in regulating immune responses to extracellular protozoan infections.
in vivo blocking of IL-10/IL-10R signaling
Dolina, J. S., et al (2014). "Liver-primed CD8+ T cells suppress antiviral adaptive immunity through galectin-9-independent T-cell immunoglobulin and mucin 3 engagement of high-mobility group box 1 in mice" Hepatology 59(4): 1351-1365.
PubMed
The liver is a tolerogenic environment exploited by persistent infections, such as hepatitis B (HBV) and C (HCV) viruses. In a murine model of intravenous hepatotropic adenovirus infection, liver-primed antiviral CD8(+) T cells fail to produce proinflammatory cytokines and do not display cytolytic activity characteristic of effector CD8(+) T cells generated by infection at an extrahepatic, that is, subcutaneous, site. Importantly, liver-generated CD8(+) T cells also appear to have a T-regulatory (Treg) cell function exemplified by their ability to limit proliferation of antigen-specific T-effector (Teff ) cells in vitro and in vivo via T-cell immunoglobulin and mucin 3 (Tim-3) expressed by the CD8(+) Treg cells. Regulatory activity did not require recognition of the canonical Tim-3 ligand, galectin-9, but was dependent on CD8(+) Treg cell-surface Tim-3 binding to the alarmin, high-mobility group box 1 (HMGB-1). CONCLUSION: Virus-specific Tim-3(+) CD8(+) T cells operating through HMGB-1 recognition in the setting of acute and chronic viral infections of the liver may act to dampen hepatic T-cell responses in the liver microenvironment and, as a consequence, limit immune-mediated tissue injury or promote the establishment of persistent infections.
in vitro blocking of IL-10R signaling
Verhagen, J. and D. C. Wraith (2014). "Blockade of LFA-1 augments in vitro differentiation of antigen-induced Foxp3(+) Treg cells" J Immunol Methods 414: 58-64.
PubMed
Adoptive transfer of antigen-specific, in vitro-induced Foxp3(+) Treg (iTreg) cells protects against autoimmune disease. To generate antigen-specific iTreg cells at high purity, however, remains a challenge. Whereas polyclonal T cell stimulation with anti-CD3 and anti-CD28 antibody yields Foxp3(+) iTreg cells at a purity of 90-95%, antigen-induced iTreg cells typically do not exceed a purity of 65-75%, even in a TCR-transgenic model. In a similar vein to thymic Treg cell selection, iTreg cell differentiation is influenced not only by antigen recognition and the availability of TGF-beta but also by co-factors including costimulation and adhesion molecules. In this study, we demonstrate that blockade of the T cell integrin Leukocyte Function-associated Antigen-1 (LFA-1) during antigen-mediated iTreg cell differentiation augments Foxp3 induction, leading to approximately 90% purity of Foxp3(+) iTreg cells. This increased efficacy not only boosts the yield of Foxp3(+) iTreg cells, it also reduces contamination with activated effector T cells, thus improving the safety of adoptive transfer immunotherapy.
in vivo blocking of IL-10/IL-10R signaling
Ruffell, B., et al (2014). "Macrophage IL-10 blocks CD8+ T cell-dependent responses to chemotherapy by suppressing IL-12 expression in intratumoral dendritic cells" Cancer Cell 26(5): 623-637.
PubMed
Blockade of colony-stimulating factor-1 (CSF-1) limits macrophage infiltration and improves response of mammary carcinomas to chemotherapy. Herein we identify interleukin (IL)-10 expression by macrophages as the critical mediator of this phenotype. Infiltrating macrophages were the primary source of IL-10 within tumors, and therapeutic blockade of IL-10 receptor (IL-10R) was equivalent to CSF-1 neutralization in enhancing primary tumor response to paclitaxel and carboplatin. Improved response to chemotherapy was CD8(+) T cell-dependent, but IL-10 did not directly suppress CD8(+) T cells or alter macrophage polarization. Instead, IL-10R blockade increased intratumoral dendritic cell expression of IL-12, which was necessary for improved outcomes. In human breast cancer, expression of IL12A and cytotoxic effector molecules were predictive of pathological complete response rates to paclitaxel.
in vivo blocking of IL-10/IL-10R signaling
Lin, C. C., et al (2014). "Bhlhe40 controls cytokine production by T cells and is essential for pathogenicity in autoimmune neuroinflammation" Nat Commun 5: 3551.
PubMed
TH1 and TH17 cells mediate neuroinflammation in experimental autoimmune encephalomyelitis (EAE), a mouse model of multiple sclerosis. Pathogenic TH cells in EAE must produce the pro-inflammatory cytokine granulocyte-macrophage colony stimulating factor (GM-CSF). TH cell pathogenicity in EAE is also regulated by cell-intrinsic production of the immunosuppressive cytokine interleukin 10 (IL-10). Here we demonstrate that mice deficient for the basic helix-loop-helix (bHLH) transcription factor Bhlhe40 (Bhlhe40(-/-)) are resistant to the induction of EAE. Bhlhe40 is required in vivo in a T cell-intrinsic manner, where it positively regulates the production of GM-CSF and negatively regulates the production of IL-10. In vitro, GM-CSF secretion is selectively abrogated in polarized Bhlhe40(-/-) TH1 and TH17 cells, and these cells show increased production of IL-10. Blockade of IL-10 receptor in Bhlhe40(-/-) mice renders them susceptible to EAE. These findings identify Bhlhe40 as a critical regulator of autoreactive T-cell pathogenicity.
in vivo blocking of IL-10/IL-10R signaling
Masson, F., et al (2014). "Id2 represses E2A-mediated activation of IL-10 expression in T cells" Blood 123(22): 3420-3428.
PubMed
Interleukin-10 (IL-10) is a key immunoregulatory cytokine that functions to prevent inflammatory and autoimmune diseases. Despite the critical role for IL-10 produced by effector CD8(+) T cells during pathogen infection and autoimmunity, the mechanisms regulating its production are poorly understood. We show that loss of the inhibitor of DNA binding 2 (Id2) in T cells resulted in aberrant IL-10 expression in vitro and in vivo during influenza virus infection and in a model of acute graft-versus-host disease (GVHD). Furthermore, IL-10 overproduction substantially reduced the immunopathology associated with GVHD. We demonstrate that Id2 acts to repress the E2A-mediated trans-activation of the Il10 locus. Collectively, our findings uncover a key regulatory role of Id2 during effector T cell differentiation necessary to limit IL-10 production by activated T cells and minimize their suppressive activity during the effector phase of disease control.
in vitro blocking of IL-10R signaling
Flow Cytometry
Hu, Z., et al (2013). "Regulatory CD8+ T cells associated with erosion of immune surveillance in persistent virus infection suppress in vitro and have a reversible proliferative defect" J Immunol 191(1): 312-322.
PubMed
CD4(+) T cell help is critical for CD8(+) T cell memory and immune surveillance against persistent virus infections. Our recent data have showed the lack of CD4(+) T cells leads to the generation of an IL-10-producing CD8(+) T cell population during persistent murine gamma-herpesvirus-68 (MHV-68) infection. IL-10 from these cells is partly responsible for erosion in immune surveillance, leading to spontaneous virus reactivation in lungs. In this study, we further characterized the generation, phenotype, and function of these IL-10-producing CD8(+) T cells by comparing with a newly identified IL-10-producing CD8(+) T cell population present during the acute stage of the infection. The IL-10-producing CD8(+) populations in acute and chronic stages differed in their requirement for CD4(+) T cell help, the dependence on IL-2/CD25 and CD40-CD40L pathways, and the ability to proliferate in vitro in response to anti-CD3 stimulation. IL-10-producing CD8(+) T cells in the chronic stage showed a distinct immunophenotypic profile, sharing partial overlap with the markers of previously reported regulatory CD8(+) T cells, and suppressed the proliferation of naive CD8(+) T cells. Notably, they retained the ability to produce effector cytokines and cytotoxic activity. In addition, the proliferative defect of the cells could be restored by addition of exogenous IL-2 or blockade of IL-10. These data suggest that the IL-10-producing CD8(+) T cells arising in chronic MHV-68 infection in the absence of CD4(+) T cell help belong to a subset of CD8(+) regulatory T cells.
in vivo blocking of IL-10/IL-10R signaling
Mishra, P. K., et al (2013). "Prevention of type 1 diabetes through infection with an intestinal nematode parasite requires IL-10 in the absence of a Th2-type response" Mucosal Immunol 6(2): 297-308.
PubMed
Helminth infection can prevent type 1 diabetes (T1D); however, the regulatory mechanisms inhibiting disease remain largely undefined. In these studies, nonobese diabetic (NOD) IL-4(-/-) mice were infected with the strictly enteric nematode parasite, Heligmosomoides polygyrus. Short-term infection, 5-7 weeks of age, inhibited T1D onset, as late as 40 weeks of age. CD4(+) T-cell STAT6 phosphorylation was inhibited, while suppressed signal transducer and activator of transcription 1 phosphorylation was sustained, as were increases in FOXP3(-), CD4(+) T-cell interleukin (IL)-10 production. Blockade of IL-10 signaling in NOD-IL-4(-/-), but not in NOD, mice during this short interval abrogated protective effects resulting in pancreatic beta-cell destruction and ultimately T1D. Transfer of CD4(+) T cells from H. polygyrus (Hp)-inoculated NOD IL-4(-/-) mice to NOD mice blocked the onset of T1D. These studies indicate that Hp infection induces non-T-regulatory cells to produce IL-10 independently of STAT6 signaling and that in this Th2-deficient environment IL-10 is essential for T1D inhibition.
in vivo blocking of IL-10/IL-10R signaling
Richter, K. and A. Oxenius (2013). "Non-neutralizing antibodies protect from chronic LCMV infection independently of activating FcgammaR or complement" Eur J Immunol 43(9): 2349-2360.
PubMed
Chronic viral infections lead to CD8(+) T cell exhaustion, characterized by impaired cytokine secretion. The presence of the immune-regulatory cytokine IL-10 promotes chronic lymphocytic choriomeningitis virus (LCMV) Clone 13 infection in mice, whereas the absence of IL-10/IL-10R signaling early during infection results in viral clearance and higher percentages and numbers of antiviral, cytokine-producing T cells. However, it is currently unclear which cell populations and effector molecules are crucial to protect against chronic infection. In this study, we demonstrate that antiviral, LCMV-binding, non-neutralizing antibodies are needed, in addition to CD4(+) and CD8(+) T cells, to clear a high-dose LCMV infection in mice, in the absence of IL-10. The interaction between CD4(+) T cells and B cells in B-cell follicles via CD40/CD40L, in addition to class switch and/or somatic hypermutation, is crucial for viral control in the absence of IL-10. Interestingly, transfer of LCMV-binding non-neutralizing antibodies protected recipients from chronic infection. In addition, viral clearance in the absence of IL-10R signaling was independent of activating Fcgamma receptors and complement. These data highlight that non-neutralizing antibodies effectively contribute to the control of LCMV infection when present prior to infection, suggesting that the induction of neutralizing antibodies is not implicitly necessary for the generation of successful vaccines.
in vivo blocking of IL-10/IL-10R signaling
Kastenmuller, W., et al (2011). "Regulatory T cells selectively control CD8+ T cell effector pool size via IL-2 restriction" J Immunol 187(6): 3186-3197.
PubMed
Regulatory T cells (Treg) are key players in maintaining immune homeostasis but have also been shown to regulate immune responses against infectious pathogens. Therefore, Treg are a promising target for modulating immune responses to vaccines to improve their efficacy. Using a viral vector system, we found that Treg act on the developing immune response early postinfection by reducing the extent of dendritic cell costimulatory molecule expression. Due to this change and the lower IL-2 production that results, a substantial fraction of CD8(+) effector T cells lose CD25 expression several days after activation. Surprisingly, such Treg-dependent limitations in IL-2 signaling by Ag-activated CD8(+) T cells prevent effector differentiation without interfering with memory cell formation. In this way, Treg fine-tune the numbers of effector T cells generated while preserving the capacity for a rapid recall response upon pathogen re-exposure. This selective effect of Treg on a subpopulation of CD8(+) T cells indicates that although manipulation of the Treg compartment might not be optimal for prophylactic vaccinations, it can be potentially exploited to optimize vaccine efficacy for therapeutic interventions.
in vivo blocking of IL-10/IL-10R signaling
Wilson, M. S., et al (2011). "IL-10 blocks the development of resistance to re-infection with Schistosoma mansoni" PLoS Pathog 7(8): e1002171.
PubMed
Despite effective chemotherapy to treat schistosome infections, re-infection rates are extremely high. Resistance to reinfection can develop, however it typically takes several years following numerous rounds of treatment and re-infection, and often develops in only a small cohort of individuals. Using a well-established and highly permissive mouse model, we investigated whether immunoregulatory mechanisms influence the development of resistance. Following Praziquantel (PZQ) treatment of S. mansoni infected mice we observed a significant and mixed anti-worm response, characterized by Th1, Th2 and Th17 responses. Despite the elevated anti-worm response in PBMC’s, liver, spleen and mesenteric lymph nodes, this did not confer any protection from a secondary challenge infection. Because a significant increase in IL-10-producing CD4(+)CD44(+)CD25(+)GITR(+) lymphocytes was observed, we hypothesised that IL-10 was obstructing the development of resistance. Blockade of IL-10 combined with PZQ treatment afforded a greater than 50% reduction in parasite establishment during reinfection, compared to PZQ treatment alone, indicating that IL-10 obstructs the development of acquired resistance. Markedly enhanced Th1, Th2 and Th17 responses, worm-specific IgG1, IgG2b and IgE and circulating eosinophils characterized the protection. This study demonstrates that blocking IL-10 signalling during PZQ treatment can facilitate the development of protective immunity and provide a highly effective strategy to protect against reinfection with S. mansoni.
Product Citations
-
-
Immunology and Microbiology
Antigen choice determines vaccine-induced generation of immunogenic versus tolerogenic dendritic cells that are marked by differential expression of pancreatic enzymes.
In The Journal of Immunology on 1 April 2013 by Farkas, A. M., Marvel, D. M., et al.
PubMed
Dendritic cells (DC) elicit immunity to pathogens and tumors while simultaneously preserving tolerance to self. Efficacious cancer vaccines have been a challenge because they are based on tumor Ags, some of which are self-Ags and thus subject to self-tolerance. One such Ag is the tumor-associated mucin MUC1. Preclinical testing of MUC1 vaccines revealed existence of peripheral tolerance to MUC1 that compromises their efficacy. To identify mechanisms that act early postvaccination and might predict vaccine outcome, we immunized human MUC1 transgenic mice (MUC1.Tg) i.v. with a MUC1 peptide vaccine against which they generate weak immunity and wild-type (WT) mice that respond strongly to the same peptide. We analyzed differences in splenic DC phenotype and function between the two mouse strains at 24 and 72 h postvaccination and also performed unbiased total gene expression analysis of the spleen. Compared to WT, MUC1.Tg spleens had significantly fewer DC, and they exhibited significantly lower expression of costimulatory molecules, decreased motility, and preferential priming of Ag-specific Foxp3(+) regulatory T cells. This tolerogenic DC phenotype and function was marked by a new putative biomarker revealed by the microarray: a cohort of pancreatic enzymes (trypsin, carboxypeptidase, elastase, and others) not previously reported in DC. These enzymes were strongly upregulated in the splenic DC from vaccinated WT mice and suppressed in the splenic DC of vaccinated MUC1.Tg mice. Suppression of the enzymes was dependent on regulatory T cells and on signaling through the IL-10R and correlated with global downregulation of DC immunostimulatory phenotype and function.
-
-
TCF1 and LEF1 promote B-1a cell homeostasis and regulatory function.
In Nature on 1 October 2025 by Shen, Q., Wang, H., et al.
PubMed
B-1 cells are innate-like immune cells abundant in serosal cavities with antibodies enriched in bacterial recognition, yet their existence in humans has been controversial1-3. The CD5+ B-1a subset expresses anti-inflammatory molecules including IL-10, PDL1 and CTLA4 and can be immunoregulatory4-6. Unlike conventional B cells that are continuously replenished, B-1a cells are produced early in life and maintained through self-renewal7. Here we show that the transcription factors TCF1 and LEF1 are critical regulators of B-1a cells. LEF1 expression is highest in fetal and bone marrow B-1 progenitors, whereas the levels of TCF1 are higher in splenic and peritoneal B-1 cells than in B-1 progenitors. TCF1-LEF1 double deficient mice have reduced B-1a cells and defective B-1a cell maintenance. These transcription factors promote MYC-dependent metabolic pathways and induce a stem-like population upon activation, partly via IL-10 production. In the absence of TCF1 and LEF1, B-1 cells proliferate excessively and acquire an exhausted phenotype with reduced IL-10 and PDL1 expression. Furthermore, adoptive transfer of B-1 cells lacking TCF1 and LEF1 fails to suppress brain inflammation. These transcription factors are also expressed in human chronic lymphocytic leukaemia B cells and in a B-1-like population that is abundant in pleural fluid and circulation of some patients with pleural infection. Our findings define a TCF1-LEF1-driven transcriptional program that integrates stemness and regulatory function in B-1a cells.
-
-
Pathology
-
Immunology and Microbiology
Interleukin-10 limits immune-mediated pathology in chronic subclinical plasmodial infection.
In PLoS Negl Trop Dis on 1 September 2025 by Silva, L. S., Monks, B. G., et al.
PubMed
Subclinical parasitemia constitutes the predominant proportion of Plasmodium spp. infections in hyperendemic regions of the world. Elevated levels of serum interleukin-10 (IL-10) are observed in both acute symptomatic and chronic subclinical Plasmodium spp. infections. The role of IL-10 in acute infection has been extensively studied; however, the role of sustained elevated levels of IL-10 in chronic subclinical plasmodial infections remains to be determined. We investigated the role of IL-10 in a long-term subclinical and patent Plasmodium chabaudi chabaudi-AS (Pc) infection using mice lacking humoral immunity (µMT-/- mice). Pc-infected µMT-/- mice exhibit a long-term (99 days) chronic infection, with microscopic levels of parasitemia and without any outward signs of disease. We found that chronically infected mice have slightly elevated levels of tumor necrosis factor α (TNFα) and interferon-γ (IFNγ), and high levels of IL-10 in the circulation. The source of IL-10 was CD4+ T cells. We found that elevated IL-10 levels were mechanistically linked to subclinical Plasmodium infection by blocking IL-10 signaling. Anti-IL-10R resulted in a marked, albeit transient, reduction of the parasitemia that was accompanied by a robust pro-inflammatory response and death of chronically infected µMT-/- mice. A similar outcome was observed in infected µMT-/- mice after CD4+ T cell depletion with anti-CD4 antibody. CD4-depleted infected µMT-/- mice exhibited reduced IL-10 and rapid weight loss, succumbing to infection by day 6 after CD4 neutralization. Our results showed that IL-10 from CD4+ T cells limits immune-mediated pathology in chronic subclinical Pc infection in µMT-/- mice by protecting against excessive inflammatory responses to blood-stage parasites.
-
-
-
Immunology and Microbiology
Coupling IL-2 with IL-10 to mitigate toxicity and enhance antitumor immunity.
In Cell Rep Med on 19 August 2025 by Ahn, J. J., Dudics, S., et al.
PubMed
Wild-type interleukin (IL)-2 induces anti-tumor immunity and toxicity, predominated by vascular leak syndrome (VLS) leading to edema, hypotension, organ toxicity, and regulatory T cell (Treg) expansion. Efforts to uncouple IL-2 toxicity from its potency have failed in the clinic. We hypothesize that IL-2 toxicity is driven by cytokine release syndrome (CRS) followed by VLS and that coupling IL-2 with IL-10 will ameliorate toxicity. Our data, generated using human primary cells, mouse models, and non-human primates, suggest that coupling of these cytokines prevents toxicity while retaining cytotoxic T cell activation and limiting Treg expansion. In syngeneic murine tumor models, DK210 epidermal growth factor receptor (EGFR), an IL-2/IL-10 fusion molecule targeted to EGFR via an anti-EGFR single-chain variable fragment (scFV), potently activates T cells and natural killer (NK) cells and elicits interferon (IFN)γ-dependent anti-tumor function without peripheral inflammatory toxicity or Treg accumulation. Therefore, combining IL-2 with IL-10 uncouples toxicity from immune activation, leading to a balanced and pleiotropic anti-tumor immune response.
-
-
-
Cancer Research
-
Endocrinology and Physiology
-
Immunology and Microbiology
Caerin 1.1/1.9-mediated antitumor immunity depends on IFNAR-Stat1 signalling of tumour infiltrating macrophage by autocrine IFNα and is enhanced by CD47 blockade.
In Sci Rep on 30 January 2025 by Li, J., Luo, Y., et al.
PubMed
Previously, we demonstrated that natural host-defence peptide caerin 1.1/caerin 1.9 (F1/F3) increases the efficacy of anti-PD-1 and therapeutic vaccine, in a HPV16 + TC-1 tumour model, but the anti-tumor mechanism of F1/F3 is still unclear. In this study, we explored the impact of F1/F3 on the tumor microenvironment in a transplanted B16 melanoma model, and further investigated the mechanism of action of F1/F3 using monoclonal antibodies to deplete relevant cells, gene knockout mice and flow cytometry. We show that F1/F3 is able to inhibit the growth of melanoma B16 tumour cells both in vitro and in vivo. Depletion of macrophages, blockade of IFNα receptor, and Stat1 inhibition each abolishes F1/F3-mediated antitumor responses. Subsequent analysis reveals that F1/F3 increases the tumour infiltration of inflammatory macrophages, upregulates the level of IFNα receptor, and promotes the secretion of IFNα by macrophages. Interestingly, F1/F3 upregulates CD47 level on tumour cells; and blocking CD47 increases F1/F3-mediated antitumor responses. Furthermore, F1/F3 intratumor injection, CD47 blockade, and therapeutic vaccination significantly increases the survival time of B16 tumour-bearing mice. These results indicate that F1/F3 may be effective to improve the efficacy of ICB and therapeutic vaccine-based immunotherapy for human epithelial cancers and warrants consideration for clinical trials.
-
-
-
Mus musculus (Mouse)
-
Neuroscience
A pathogenic role for IL-10 signalling in capillary stalling and cognitive impairment in type 1 diabetes.
In Nat Metab on 1 November 2024 by Sharma, S., Cheema, M., et al.
PubMed
Vascular pathology is associated with cognitive impairment in diseases such as type 1 diabetes; however, how capillary flow is affected and the underlying mechanisms remain elusive. Here we show that capillaries in the diabetic mouse brain in both sexes are prone to stalling, with blocks consisting primarily of erythrocytes in branches off ascending venules. Screening for circulating inflammatory cytokines revealed persistently high levels of interleukin-10 (IL-10) in diabetic mice. Contrary to expectation, stimulating IL-10 signalling increased capillary obstruction, whereas inhibiting IL-10 receptors with neutralizing antibodies or endothelial specific knockdown in diabetic mice reversed these impairments. Chronic treatment of diabetic mice with IL-10 receptor neutralizing antibodies improved cerebral blood flow, increased capillary flux and diameter, downregulated haemostasis and cell adhesion-related gene expression, and reversed cognitive deficits. These data suggest that IL-10 signalling has an unexpected pathogenic role in cerebral microcirculatory defects and cognitive impairment associated with type 1 diabetes.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
In vitro experiments
Caerin 1.1 and 1.9 peptides halt B16 melanoma metastatic tumours via expanding cDC1 and reprogramming tumour macrophages.
In J Transl Med on 28 October 2024 by Fu, Q., Luo, Y., et al.
PubMed
Cancer immunotherapy, particularly immune checkpoint inhibitors (ICBs) such as anti-PD-1 antibodies, has revolutionised cancer treatment, although response rates vary among patients. Previous studies have demonstrated that caerin 1.1 and 1.9, host-defence peptides from the Australian tree frog, enhance the effectiveness of anti-PD-1 and therapeutic vaccines in a murine TC-1 model by activating tumour-associated macrophages intratumorally.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
Caerin 1.1 and 1.9 peptides halt B16 melanoma metastatic tumours via expanding cDC1 and reprogramming tumour macrophages
In Research Square on 10 August 2024 by Fu, Q., Luo, Y., et al.
-
-
-
Mus musculus (Mouse)
-
Neuroscience
A pathogenic role for IL-10 signalling in capillary stalling and cognitive impairment in type 1 diabetes
In bioRxiv on 2 April 2024 by Sharma, S., Cheema, M., et al.
-
-
-
Mus musculus (Mouse)
-
Biochemistry and Molecular biology
The transcription factors TCF1 and LEF1 drive B-1a cell development, self-renewal, and regulatory function.
In Research Square on 17 January 2024 by Vinuesa, C., Shen, Q., et al.
-
-
-
Immunology and Microbiology
-
Endocrinology and Physiology
-
Cancer Research
Caerin 1.1/1.9-mediated antitumor immunity depends on IFNAR-Stat1 signalling of tumour infiltrating macrophage by autocrine of IFNα and is enhanced by CD47 blockade
In Research Square on 13 December 2023 by Li, J., Luo, Y., et al.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Intestinal microbiota-specific Th17 cells possess regulatory properties and suppress effector T cells via c-MAF and IL-10.
In Immunity on 12 December 2023 by Brockmann, L., Tran, A., et al.
PubMed
Commensal microbes induce cytokine-producing effector tissue-resident CD4+ T cells, but the function of these T cells in mucosal homeostasis is not well understood. Here, we report that commensal-specific intestinal Th17 cells possess an anti-inflammatory phenotype marked by expression of interleukin (IL)-10 and co-inhibitory receptors. The anti-inflammatory phenotype of gut-resident commensal-specific Th17 cells was driven by the transcription factor c-MAF. IL-10-producing commensal-specific Th17 cells were heterogeneous and derived from a TCF1+ gut-resident progenitor Th17 cell population. Th17 cells acquired IL-10 expression and anti-inflammatory phenotype in the small-intestinal lamina propria. IL-10 production by CD4+ T cells and IL-10 signaling in intestinal macrophages drove IL-10 expression by commensal-specific Th17 cells. Intestinal commensal-specific Th17 cells possessed immunoregulatory functions and curbed effector T cell activity in vitro and in vivo in an IL-10-dependent and c-MAF-dependent manner. Our results suggest that tissue-resident commensal-specific Th17 cells perform regulatory functions in mucosal homeostasis.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Kruppel-like factor 2+ CD4 T cells avert microbiota-induced intestinal inflammation.
In Cell Rep on 28 November 2023 by Shao, T. Y., Jiang, T. T., et al.
PubMed
Intestinal colonization by antigenically foreign microbes necessitates expanded peripheral immune tolerance. Here we show commensal microbiota prime expansion of CD4 T cells unified by the Kruppel-like factor 2 (KLF2) transcriptional regulator and an essential role for KLF2+ CD4 cells in averting microbiota-driven intestinal inflammation. CD4 cells with commensal specificity in secondary lymphoid organs and intestinal tissues are enriched for KLF2 expression, and distinct from FOXP3+ regulatory T cells or other differentiation lineages. Mice with conditional KLF2 deficiency in T cells develop spontaneous rectal prolapse and intestinal inflammation, phenotypes overturned by eliminating microbiota or reconstituting with donor KLF2+ cells. Activated KLF2+ cells selectively produce IL-10, and eliminating IL-10 overrides their suppressive function in vitro and protection against intestinal inflammation in vivo. Together with reduced KLF2+ CD4 cell accumulation in Crohn's disease, a necessity for the KLF2+ subpopulation of T regulatory type 1 (Tr1) cells in sustaining commensal tolerance is demonstrated.
-
-
-
Immunology and Microbiology
-
Mus musculus (Mouse)
Deletion of Endogenous Neuregulin-4 Limits Adaptive Immunity During Interleukin-10 Receptor-Neutralizing Colitis.
In Inflamm Bowel Dis on 2 November 2023 by Bernard, J. K., Bucar, E. B., et al.
PubMed
Growth factors are essential for maintenance of intestinal health. We previously showed that exogenous neuregulin-4 (NRG4) promotes colonocyte survival during cytokine challenge and is protective against acute models of intestinal inflammation. However, the function(s) of endogenous NRG4 are not well understood. Using NRG4-/- mice, we tested the role of endogenous NRG4 in models of colitis skewed toward either adaptive (interleukin-10 receptor [IL-10R] neutralization) or innate (dextran sulfate sodium [DSS]) immune responses.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
The enteric nervous system relays psychological stress to intestinal inflammation.
In Cell on 22 June 2023 by Schneider, K. M., Blank, N., et al.
PubMed
Mental health profoundly impacts inflammatory responses in the body. This is particularly apparent in inflammatory bowel disease (IBD), in which psychological stress is associated with exacerbated disease flares. Here, we discover a critical role for the enteric nervous system (ENS) in mediating the aggravating effect of chronic stress on intestinal inflammation. We find that chronically elevated levels of glucocorticoids drive the generation of an inflammatory subset of enteric glia that promotes monocyte- and TNF-mediated inflammation via CSF1. Additionally, glucocorticoids cause transcriptional immaturity in enteric neurons, acetylcholine deficiency, and dysmotility via TGF-β2. We verify the connection between the psychological state, intestinal inflammation, and dysmotility in three cohorts of IBD patients. Together, these findings offer a mechanistic explanation for the impact of the brain on peripheral inflammation, define the ENS as a relay between psychological stress and gut inflammation, and suggest that stress management could serve as a valuable component of IBD care.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Early Life Stress in Mice Leads to Impaired Colonic Corticosterone Production and Prolonged Inflammation Following Induction of Colitis.
In Inflamm Bowel Dis on 1 June 2023 by Muir, R. Q., Klocke, B. J., et al.
PubMed
Early life stress (ELS) is an environmental trigger believed to promote increased risk of IBD. Our goal was to identify mechanisms whereby ELS in mice affects susceptibility to and/or severity of gut inflammation.
-
-
Distinct stimulus-dependent neutrophil dynamics revealed by real-time imaging of intestinal mucosa after acute injury.
In PNAS Nexus on 1 November 2022 by Azcutia, V., Kelm, M., et al.
PubMed
Clinical symptoms in many inflammatory diseases of the intestine are directly related to neutrophil (PMN) migration across colonic mucosa and into the intestinal lumen, yet in-vivo studies detailing this process are lacking. Using real-time intravital microscopy and a new distal colon loop model, we report distinct PMN migratory dynamics in response to several models of acute colonic injury. PMNs exhibited rapid swarming responses after mechanically induced intestinal wounds. Similar numbers of PMNs infiltrated colonic mucosa after wounding in germ-free mice, suggesting microbiota-independent mechanisms. By contrast, acute mucosal injury secondary to either a treatment of mice with dextran sodium sulfate or an IL-10 receptor blockade model of colitis resulted in lamina propria infiltration with PMNs that were largely immotile. Biopsy wounding of colonic mucosa in DSS-treated mice did not result in enhanced PMN swarming however, intraluminal application of the neutrophil chemoattractant LTB4 under such conditions resulted in enhanced transepithelial migration of PMNs. Analyses of PMNs that had migrated into the colonic lumen revealed that the majority of PMNs were directly recruited from the circulation and not from the immotile pool in the mucosa. Decreased PMN motility parallels upregulation of the receptor CXCR4 and apoptosis. Similarly, increased expression of CXCR4 on human PMNs was observed in colonic biopsies from people with active ulcerative colitis. This new approach adds an important tool to investigate mechanisms regulating PMN migration across mucosa within the distal intestine and will provide new insights for developing future anti-inflammatory and pro-repair therapies.
-
-
Immunology and Microbiology
-
Mus musculus (Mouse)
CD11c+ myeloid cell exosomes reduce intestinal inflammation during colitis.
In JCI Insight on 10 October 2022 by Bauer, K. M., Nelson, M. C., et al.
PubMed
Intercellular communication is critical for homeostasis in mammalian systems, including the gastrointestinal (GI) tract. Exosomes are nanoscale lipid extracellular vesicles that mediate communication between many cell types. Notably, the roles of immune cell exosomes in regulating GI homeostasis and inflammation are largely uncharacterized. By generating mouse strains deficient in cell-specific exosome production, we demonstrate deletion of the small GTPase Rab27A in CD11c+ cells exacerbated murine colitis, which was reversible through administration of DC-derived exosomes. Profiling RNAs within colon exosomes revealed a distinct subset of miRNAs carried by colon- and DC-derived exosomes. Among antiinflammatory exosomal miRNAs, miR-146a was transferred from gut immune cells to myeloid and T cells through a Rab27-dependent mechanism, targeting Traf6, IRAK-1, and NLRP3 in macrophages. Further, we have identified a potentially novel mode of exosome-mediated DC and macrophage crosstalk that is capable of skewing gut macrophages toward an antiinflammatory phenotype. Assessing clinical samples, RAB27A, select miRNAs, and RNA-binding proteins that load exosomal miRNAs were dysregulated in ulcerative colitis patient samples, consistent with our preclinical mouse model findings. Together, our work reveals an exosome-mediated regulatory mechanism underlying gut inflammation and paves the way for potential use of miRNA-containing exosomes as a novel therapeutic for inflammatory bowel disease.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
Unravelling the sex-specific diversity and functions of adrenal gland macrophages.
In Cell Rep on 14 June 2022 by Dolfi, B., Gallerand, A., et al.
PubMed
Despite the ubiquitous function of macrophages across the body, the diversity, origin, and function of adrenal gland macrophages remain largely unknown. We define the heterogeneity of adrenal gland immune cells using single-cell RNA sequencing and use genetic models to explore the developmental mechanisms yielding macrophage diversity. We define populations of monocyte-derived and embryonically seeded adrenal gland macrophages and identify a female-specific subset with low major histocompatibility complex (MHC) class II expression. In adulthood, monocyte recruitment dominates adrenal gland macrophage maintenance in female mice. Adrenal gland macrophage sub-tissular distribution follows a sex-dimorphic pattern, with MHC class IIlow macrophages located at the cortico-medullary junction. Macrophage sex dimorphism depends on the presence of the cortical X-zone. Adrenal gland macrophage depletion results in altered tissue homeostasis, modulated lipid metabolism, and decreased local aldosterone production during stress exposure. Overall, these data reveal the heterogeneity of adrenal gland macrophages and point toward sex-restricted distribution and functions of these cells.
-
-
-
Cancer Research
-
Immunology and Microbiology
Targeting SNORA38B attenuates tumorigenesis and sensitizes immune checkpoint blockade in non-small cell lung cancer by remodeling the tumor microenvironment via regulation of GAB2/AKT/mTOR signaling pathway.
In J Immunother Cancer on 1 May 2022 by Zhuo, Y., Li, S., et al.
PubMed
Non-coding RNAs (ncRNAs), including small nucleolar RNAs (snoRNAs), are widely involved in the physiological and pathological processes of human beings. While up to date, although considerable progress has been achieved in ncRNA-related pathogenesis of non-small cell lung cancer (NSCLC), the underlying mechanisms and biological significance of snoRNAs in NSCLC still need to be further clarified.
-