Catalog #BE0150
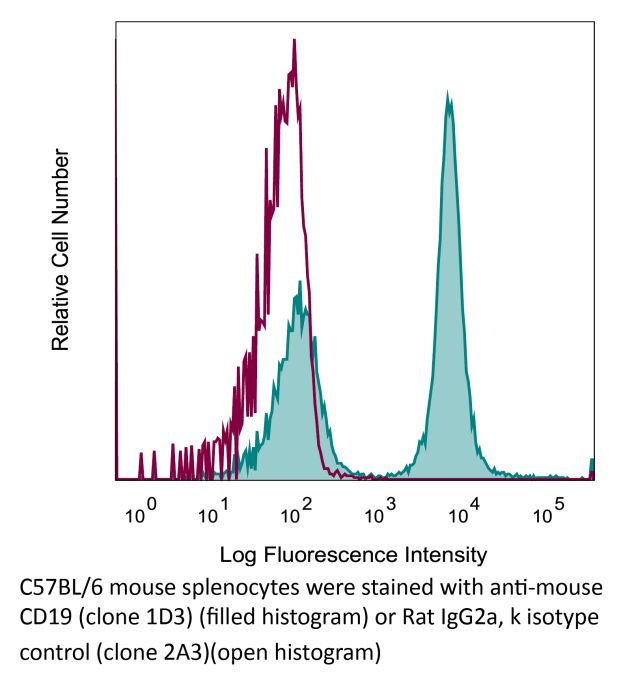
InVivoMAb anti-mouse CD19
Clone
1D3
Reactivities
Mouse
Product Citations
44
Isotype
Rat IgG2a, κ