InVivoMAb anti-mouse GM-CSF
Product Description
Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | Recombinant mouse GM-CSF |
| Reported Applications |
in vivo GM-CSF neutralization in vitro GM-CSF neutralization Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Endotoxin |
≤1EU/mg (≤0.001EU/μg) Determined by LAL assay |
| Purity |
≥95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Production | Purified from cell culture supernatant in an animal-free facility |
| Purification | Protein G |
| RRID | AB_2687738 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| Need a Custom Formulation? | See All Antibody Customization Options |
Application References
in vivo GM-CSF neutralization
Flow Cytometry
Kulcsar, K. A., et al (2014). "Interleukin 10 modulation of pathogenic Th17 cells during fatal alphavirus encephalomyelitis" Proc Natl Acad Sci U S A 111(45): 16053-16058.
PubMed
Mosquito-borne alphaviruses are important causes of epidemic encephalomyelitis. Neuronal cell death during fatal alphavirus encephalomyelitis is immune-mediated; however, the types of cells involved and their regulation have not been determined. We show that the virus-induced inflammatory response was accompanied by production of the regulatory cytokine IL-10, and in the absence of IL-10, paralytic disease occurred earlier and mice died faster. To determine the reason for accelerated disease in the absence of IL-10, immune responses in the CNS of IL-10(-/-) and wild-type (WT) mice were compared. There were no differences in the amounts of brain inflammation or peak virus replication; however, IL-10(-/-) animals had accelerated and increased infiltration of CD4(+)IL-17A(+) and CD4(+)IL-17A(+)IFNgamma(+) cells compared with WT animals. Th17 cells infiltrating the brain demonstrated a pathogenic phenotype with the expression of the transcription factor, Tbet, and the production of granzyme B, IL-22, and GM-CSF, with greater production of GM-CSF in IL-10(-/-) mice. Therefore, in fatal alphavirus encephalomyelitis, pathogenic Th17 cells enter the CNS at the onset of neurologic disease and, in the absence of IL-10, appear earlier, develop into Th1/Th17 cells more often, and have greater production of GM-CSF. This study demonstrates a role for pathogenic Th17 cells in fatal viral encephalitis.
in vivo GM-CSF neutralization
Samavedam, U. K., et al (2014). "GM-CSF modulates autoantibody production and skin blistering in experimental epidermolysis bullosa acquisita" J Immunol 192(2): 559-571.
PubMed
Across a variety of adverse life circumstances, such as social isolation and low socioeconomic status, mammalian immune cells have been found to show a conserved transcriptional response to adversity (CTRA) involving increased expression of proinflammatory genes. The present study examines whether such effects might stem in part from the selective up-regulation of a subpopulation of immature proinflammatory monocytes (Ly-6c(high) in mice, CD16(-) in humans) within the circulating leukocyte pool. Transcriptome representation analyses showed relative expansion of the immature proinflammatory monocyte transcriptome in peripheral blood mononuclear cells from people subject to chronic social stress (low socioeconomic status) and mice subject to repeated social defeat. Cellular dissection of the mouse peripheral blood mononuclear cell transcriptome confirmed these results, and promoter-based bioinformatic analyses indicated increased activity of transcription factors involved in early myeloid lineage differentiation and proinflammatory effector function (PU.1, NF-kappaB, EGR1, MZF1, NRF2). Analysis of bone marrow hematopoiesis confirmed increased myelopoietic output of Ly-6c(high) monocytes and Ly-6c(intermediate) granulocytes in mice subject to repeated social defeat, and these effects were blocked by pharmacologic antagonists of beta-adrenoreceptors and the myelopoietic growth factor GM-CSF. These results suggest that sympathetic nervous system-induced up-regulation of myelopoiesis mediates the proinflammatory component of the leukocyte CTRA dynamic and may contribute to the increased risk of inflammation-related disease associated with adverse social conditions.
in vivo GM-CSF neutralization
Powell, N. D., et al (2013). "Social stress up-regulates inflammatory gene expression in the leukocyte transcriptome via beta-adrenergic induction of myelopoiesis" Proc Natl Acad Sci U S A 110(41): 16574-16579.
PubMed
Across a variety of adverse life circumstances, such as social isolation and low socioeconomic status, mammalian immune cells have been found to show a conserved transcriptional response to adversity (CTRA) involving increased expression of proinflammatory genes. The present study examines whether such effects might stem in part from the selective up-regulation of a subpopulation of immature proinflammatory monocytes (Ly-6c(high) in mice, CD16(-) in humans) within the circulating leukocyte pool. Transcriptome representation analyses showed relative expansion of the immature proinflammatory monocyte transcriptome in peripheral blood mononuclear cells from people subject to chronic social stress (low socioeconomic status) and mice subject to repeated social defeat. Cellular dissection of the mouse peripheral blood mononuclear cell transcriptome confirmed these results, and promoter-based bioinformatic analyses indicated increased activity of transcription factors involved in early myeloid lineage differentiation and proinflammatory effector function (PU.1, NF-kappaB, EGR1, MZF1, NRF2). Analysis of bone marrow hematopoiesis confirmed increased myelopoietic output of Ly-6c(high) monocytes and Ly-6c(intermediate) granulocytes in mice subject to repeated social defeat, and these effects were blocked by pharmacologic antagonists of beta-adrenoreceptors and the myelopoietic growth factor GM-CSF. These results suggest that sympathetic nervous system-induced up-regulation of myelopoiesis mediates the proinflammatory component of the leukocyte CTRA dynamic and may contribute to the increased risk of inflammation-related disease associated with adverse social conditions.
in vivo GM-CSF neutralization
Subramanian Vignesh, K., et al (2013). "Granulocyte macrophage-colony stimulating factor induced Zn sequestration enhances macrophage superoxide and limits intracellular pathogen survival" Immunity 39(4): 697-710.
PubMed
Macrophages possess numerous mechanisms to combat microbial invasion, including sequestration of essential nutrients, like zinc (Zn). The pleiotropic cytokine granulocyte macrophage-colony stimulating factor (GM-CSF) enhances antimicrobial defenses against intracellular pathogens such as Histoplasma capsulatum, but its mode of action remains elusive. We have found that GM-CSF-activated infected macrophages sequestered labile Zn by inducing binding to metallothioneins (MTs) in a STAT3 and STAT5 transcription-factor-dependent manner. GM-CSF upregulated expression of Zn exporters, Slc30a4 and Slc30a7; the metal was shuttled away from phagosomes and into the Golgi apparatus. This distinctive Zn sequestration strategy elevated phagosomal H(+) channel function and triggered reactive oxygen species generation by NADPH oxidase. Consequently, H. capsulatum was selectively deprived of Zn, thereby halting replication and fostering fungal clearance. GM-CSF mediated Zn sequestration via MTs in vitro and in vivo in mice and in human macrophages. These findings illuminate a GM-CSF-induced Zn-sequestration network that drives phagocyte antimicrobial effector function.
in vivo GM-CSF neutralization
in vitro GM-CSF neutralization
Khajah, M., et al (2011). "Granulocyte-macrophage colony-stimulating factor (GM-CSF): a chemoattractive agent for murine leukocytes in vivo" J Leukoc Biol 89(6): 945-953.
PubMed
GM-CSF is well recognized as a proliferative agent for hematopoietic cells and exerts a priming function on neutrophils. The aim of this study was to determine if GM-CSF has a role as a neutrophil chemoattractant in vivo and if it can contribute to recruitment during intestinal inflammation. Initial studies in vitro, using the under-agarose gel assay, determined that GM-CSF can induce neutrophil migration at a much lower molar concentration than the fMLP-like peptide WKYMVm (33.5-134 nM vs. 1-10 muM). GM-CSF-induced neutrophil migration was ablated (<95%) using neutrophils derived from GMCSFRbeta(-/-) mice and significantly attenuated by 42% in PI3Kgamma(-/-)neutrophils. In vivo, a significant increase in leukocyte recruitment was observed using intravital microscopy 4 h post-GM-CSF (10 mug/kg) injection, which was comparable with leukocyte recruitment induced by KC (40 mug/kg). GM-CSF-induced recruitment was abolished, and KC-induced recruitment was maintained in GMCSFRbeta(-/-) mice. Furthermore, in vivo migration of extravascular leukocytes was observed toward a gel containing GM-CSF in WT but not GMCSFRbeta(-/-) mice. Finally, in a model of intestinal inflammation (TNBS-induced colitis), colonic neutrophil recruitment, assessed using the MPO assay, was attenuated significantly in anti-GM-CSF-treated mice or GMCSFRbeta(-/-) mice. These data demonstrate that GM-CSF is a potent chemoattractant in vitro and can recruit neutrophils from the microvasculature and induce extravascular migration in vivo in a beta subunit-dependent manner. This property of GM-CSF may contribute significantly to recruitment during intestinal inflammation.
Product Citations
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Genetics
Cancer cell genetics shaping of the tumor microenvironment reveals myeloid cell-centric exploitable vulnerabilities in hepatocellular carcinoma.
In Nat Commun on 22 March 2024 by Ramirez, C. F. A., Taranto, D., et al.
PubMed
Myeloid cells are abundant and plastic immune cell subsets in the liver, to which pro-tumorigenic, inflammatory and immunosuppressive roles have been assigned in the course of tumorigenesis. Yet several aspects underlying their dynamic alterations in hepatocellular carcinoma (HCC) progression remain elusive, including the impact of distinct genetic mutations in shaping a cancer-permissive tumor microenvironment (TME). Here, in newly generated, clinically-relevant somatic female HCC mouse models, we identify cancer genetics' specific and stage-dependent alterations of the liver TME associated with distinct histopathological and malignant HCC features. Mitogen-activated protein kinase (MAPK)-activated, NrasG12D-driven tumors exhibit a mixed phenotype of prominent inflammation and immunosuppression in a T cell-excluded TME. Mechanistically, we report a NrasG12D cancer cell-driven, MEK-ERK1/2-SP1-dependent GM-CSF secretion enabling the accumulation of immunosuppressive and proinflammatory monocyte-derived Ly6Clow cells. GM-CSF blockade curbs the accumulation of these cells, reduces inflammation, induces cancer cell death and prolongs animal survival. Furthermore, GM-CSF neutralization synergizes with a vascular endothelial growth factor (VEGF) inhibitor to restrain HCC outgrowth. These findings underscore the profound alterations of the myeloid TME consequential to MAPK pathway activation intensity and the potential of GM-CSF inhibition as a myeloid-centric therapy tailored to subsets of HCC patients.
-
-
-
Mus musculus (Mouse)
-
Cancer Research
-
Genetics
Cancer cell genetics shaping of the tumor microenvironment reveals myeloid cell-centric exploitable vulnerabilities in hepatocellular carcinoma
In bioRxiv on 1 November 2023 by Ramirez, C. F., Taranto, D., et al.
-
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Dampening type 2 properties of group 2 innate lymphoid cells by a gammaherpesvirus infection reprograms alveolar macrophages.
In Sci Immunol on 24 February 2023 by Loos, P., Baiwir, J., et al.
PubMed
Immunological dysregulation in asthma is associated with changes in exposure to microorganisms early in life. Gammaherpesviruses (γHVs), such as Epstein-Barr virus, are widespread human viruses that establish lifelong infection and profoundly shape host immunity. Using murid herpesvirus 4 (MuHV-4), a mouse γHV, we show that after infection, lung-resident and recruited group 2 innate lymphoid cells (ILC2s) exhibit a reduced ability to expand and produce type 2 cytokines in response to house dust mites, thereby contributing to protection against asthma. In contrast, MuHV-4 infection triggers GM-CSF production by those lung ILC2s, which orders the differentiation of monocytes (Mos) into alveolar macrophages (AMs) without promoting their type 2 functions. In the context of γHV infection, ILC2s are therefore essential cells within the pulmonary niche that imprint the tissue-specific identity of Mo-derived AMs and shape their function well beyond the initial acute infection.
-
-
-
Mus musculus (Mouse)
Continuous sensing of IFNα by hepatic endothelial cells shapes a vascular antimetastatic barrier.
In Elife on 25 October 2022 by Tran, N. L., Ferreira, L. M., et al.
PubMed
Hepatic metastases are a poor prognostic factor of colorectal carcinoma (CRC) and new strategies to reduce the risk of liver CRC colonization are highly needed. Herein, we used mouse models of hepatic metastatization to demonstrate that the continuous infusion of therapeutic doses of interferon-alpha (IFNα) controls CRC invasion by acting on hepatic endothelial cells (HECs). Mechanistically, IFNα promoted the development of a vascular antimetastatic niche characterized by liver sinusoidal endothelial cells (LSECs) defenestration extracellular matrix and glycocalyx deposition, thus strengthening the liver vascular barrier impairing CRC trans-sinusoidal migration, without requiring a direct action on tumor cells, hepatic stellate cells, hepatocytes, or liver dendritic cells (DCs), Kupffer cells (KCs) and liver capsular macrophages (LCMs). Moreover, IFNα endowed LSECs with efficient cross-priming potential that, along with the early intravascular tumor burden reduction, supported the generation of antitumor CD8+ T cells and ultimately led to the establishment of a protective long-term memory T cell response. These findings provide a rationale for the use of continuous IFNα therapy in perioperative settings to reduce CRC metastatic spreading to the liver.
-
-
-
Immunology and Microbiology
GM-CSF drives immune-mediated glomerular disease by licensing monocyte-derived cells to produce MMP12
In bioRxiv on 16 June 2022 by Paust, H., Song, N., et al.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Immunology and Microbiology
GM-CSF production by non-classical monocytes controls antagonistic LPS-driven functions in allergic inflammation.
In Cell Rep on 28 December 2021 by Kaur, K., Bachus, H., et al.
PubMed
Lipopolysaccharide (LPS) can either promote or prevent T helper 2 (Th2) cell allergic responses. However, the underlying mechanism remains unknown. We show here that LPS activity switches from pro-pathogenic to protective depending on the production of granulocyte-macrophage colony-stimulating factor (GM-CSF) by non-classical monocytes. In the absence of GM-CSF, LPS can favor pathogenic Th2 cell responses by supporting the trafficking of lung-migratory dendritic cells (mDC2s) into the lung-draining lymph node. However, when non-classical monocytes produce GM-CSF, LPS and GM-CSF synergize to differentiate monocyte-derived DCs from classical Ly6Chi monocytes that instruct mDC2s for Th2 cell suppression. Importantly, only allergens with cysteine protease activity trigger GM-CSF production by non-classical monocytes. Hence, the therapeutic effect of LPS is restricted to allergens with this enzymatic activity. Treatment with GM-CSF, however, restores the protective effects of LPS. Thus, GM-CSF produced by non-classical monocytes acts as a rheostat that fine-tunes the pathogenic and therapeutic functions of LPS.
-
-
-
Immunology and Microbiology
Biological Aging of CNS-Resident Cells Alters the Clinical Course and Immunopathology of Autoimmune Demyelinating Disease
In bioRxiv on 27 December 2021 by Atkinson, J. R., Jerome, A. D., et al.
-
-
-
Cancer Research
-
Immunology and Microbiology
All-trans retinoic acid overcomes solid tumor radioresistance by inducing inflammatory macrophages.
In Sci Immunol on 15 June 2021 by Rao, E., Hou, Y., et al.
PubMed
Radiotherapy (RT) is an important anti-cancer treatment modality that activates innate and adaptive immune responses. When all-trans retinoic acid (RA) was administered with radiation, we observed superior antitumor responses compared to ionizing radiation (IR) alone or RA alone. The superior antitumor effects of combination treatment were accompanied by a dramatic increase of TNF-α- and inducible nitric oxide synthase (iNOS)-producing inflammatory macrophages in local and distal non-irradiated (distal) tumors. Inflammatory macrophages are essential for the therapeutic efficacy of combination treatment by inducing effector T cell infiltration and enhancing the effector T cell to regulatory T cell ratio in local and distal tumors. T cells and T cell-derived IFN-γ are crucial for increasing inflammatory macrophage levels in IR and RA treated tumors. Notably, whereas CD8+ T cells are required for the antitumor response to IR, CD4+ T cells are required for the effectiveness of the IR and RA combination. Combination treatment with RA enhanced the abscopal response when radiation and PD-L1 blockade were used together. The synergistic positive feedback loop of inflammatory macrophages and adaptive immunity is required for the antitumor efficacy of IR plus RA combination treatment. Our findings provide a translational and relatively nontoxic strategy for enhancing the local and systemic antitumor effects of IR.
-
-
-
Cancer Research
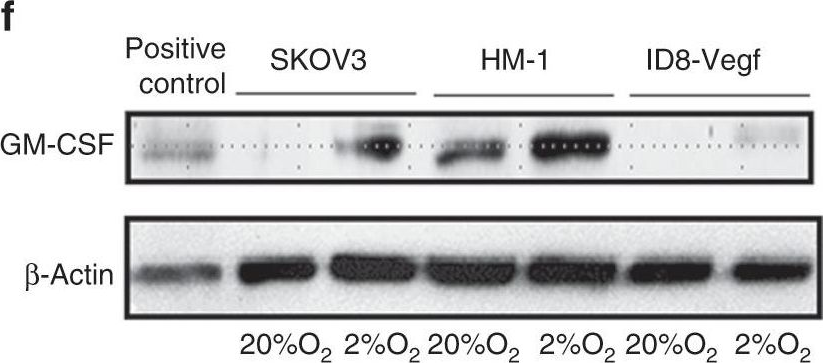
Genetically Defined, Syngeneic Organoid Platform for Developing Combination Therapies for Ovarian Cancer.
In Cancer Discov on 1 February 2021 by Zhang, S., Iyer, S., et al.
PubMed
The paucity of genetically informed, immunocompetent tumor models impedes evaluation of conventional, targeted, and immune therapies. By engineering mouse fallopian tube epithelial organoids using lentiviral gene transduction and/or CRISPR/Cas9 mutagenesis, we generated multiple high-grade serous tubo-ovarian cancer (HGSC) models exhibiting mutational combinations seen in patients with HGSC. Detailed analysis of homologous recombination (HR)-proficient (Trp53-/-;Ccne1OE;Akt2OE;KrasOE ), HR-deficient (Trp53-/-;Brca1-/-;MycOE ), and unclassified (Trp53-/-;Pten-/-;Nf1-/- ) organoids revealed differences in in vitro properties (proliferation, differentiation, and "secretome"), copy-number aberrations, and tumorigenicity. Tumorigenic organoids had variable sensitivity to HGSC chemotherapeutics, and evoked distinct immune microenvironments that could be modulated by neutralizing organoid-produced chemokines/cytokines. These findings enabled development of a chemotherapy/immunotherapy regimen that yielded durable, T cell-dependent responses in Trp53-/-;Ccne1OE;Akt2OE;Kras HGSC; in contrast, Trp53-/-;Pten-/-;Nf1-/- tumors failed to respond. Mouse and human HGSC models showed genotype-dependent similarities in chemosensitivity, secretome, and immune microenvironment. Genotype-informed, syngeneic organoid models could provide a platform for the rapid evaluation of tumor biology and therapeutics. SIGNIFICANCE: The lack of genetically informed, diverse, immunocompetent models poses a major barrier to therapeutic development for many malignancies. Using engineered fallopian tube organoids to study the cell-autonomous and cell-nonautonomous effects of specific combinations of mutations found in HGSC, we suggest an effective combination treatment for the currently intractable CCNE1-amplified subgroup.This article is highlighted in the In This Issue feature, p. 211.
-
-
Co-option of Neutrophil Fates by Tissue Environments.
In Cell on 25 November 2020 by Ballesteros, I., Rubio-Ponce, A., et al.
PubMed
Classically considered short-lived and purely defensive leukocytes, neutrophils are unique in their fast and moldable response to stimulation. This plastic behavior may underlie variable and even antagonistic functions during inflammation or cancer, yet the full spectrum of neutrophil properties as they enter healthy tissues remains unexplored. Using a new model to track neutrophil fates, we found short but variable lifetimes across multiple tissues. Through analysis of the receptor, transcriptional, and chromatin accessibility landscapes, we identify varying neutrophil states and assign non-canonical functions, including vascular repair and hematopoietic homeostasis. Accordingly, depletion of neutrophils compromised angiogenesis during early age, genotoxic injury, and viral infection, and impaired hematopoietic recovery after irradiation. Neutrophils acquired these properties in target tissues, a process that, in the lungs, occurred in CXCL12-rich areas and relied on CXCR4. Our results reveal that tissues co-opt neutrophils en route for elimination to induce programs that support their physiological demands.
-
-
Mus musculus (Mouse)
-
Immunology and Microbiology
Legionella-Infected Macrophages Engage the Alveolar Epithelium to Metabolically Reprogram Myeloid Cells and Promote Antibacterial Inflammation.
In Cell Host Microbe on 11 November 2020 by Liu, X., Boyer, M. A., et al.
PubMed
Alveolar macrophages are among the first immune cells that respond to inhaled pathogens. However, numerous pathogens block macrophage-intrinsic immune responses, making it unclear how robust antimicrobial responses are generated. The intracellular bacterium Legionella pneumophila inhibits host translation, thereby impairing cytokine production by infected macrophages. Nevertheless, Legionella-infected macrophages induce an interleukin-1 (IL-1)-dependent inflammatory cytokine response by recruited monocytes and other cells that controls infection. How IL-1 directs these cells to produce inflammatory cytokines is unknown. Here, we show that collaboration with the alveolar epithelium is critical for controlling infection. IL-1 induces the alveolar epithelium to produce granulocyte-macrophage colony-stimulating factor (GM-CSF). Intriguingly, GM-CSF signaling amplifies inflammatory cytokine production in recruited monocytes by enhancing Toll-like receptor (TLR)-induced glycolysis. Our findings reveal that alveolar macrophages engage alveolar epithelial signals to metabolically reprogram monocytes for antibacterial inflammation.
-
-
-
Cancer Research
-
Immunology and Microbiology
Selective inhibition of mTORC1 in tumor vessels increases antitumor immunity.
In JCI Insight on 6 August 2020 by Wang, S., Raybuck, A., et al.
PubMed
A tumor blood vessel is a key regulator of tissue perfusion, immune cell trafficking, cancer metastasis, and therapeutic responsiveness. mTORC1 is a signaling node downstream of multiple angiogenic factors in the endothelium. However, mTORC1 inhibitors have limited efficacy in most solid tumors, in part due to inhibition of immune function at high doses used in oncology patients and compensatory PI3K signaling triggered by mTORC1 inhibition in tumor cells. Here we show that low-dose RAD001/everolimus, an mTORC1 inhibitor, selectively targets mTORC1 signaling in endothelial cells (ECs) without affecting tumor cells or immune cells, resulting in tumor vessel normalization and increased antitumor immunity. Notably, this phenotype was recapitulated upon targeted inducible gene ablation of the mTORC1 component Raptor in tumor ECs (RaptorECKO). Tumors grown in RaptorECKO mice displayed a robust increase in tumor-infiltrating lymphocytes due to GM-CSF-mediated activation of CD103+ dendritic cells and displayed decreased tumor growth and metastasis. GM-CSF neutralization restored tumor growth and metastasis, as did T cell depletion. Importantly, analyses of human tumor data sets support our animal studies. Collectively, these findings demonstrate that endothelial mTORC1 is an actionable target for tumor vessel normalization, which could be leveraged to enhance antitumor immune therapies.
-
-
-
Immunology and Microbiology
-
Mus musculus (Mouse)
GM-CSF Calibrates Macrophage Defense and Wound Healing Programs during Intestinal Infection and Inflammation.
In Cell Rep on 7 July 2020 by Castro-Dopico, T., Fleming, A., et al.
PubMed
Macrophages play a central role in intestinal immunity, but inappropriate macrophage activation is associated with inflammatory bowel disease (IBD). Here, we identify granulocyte-macrophage colony stimulating factor (GM-CSF) as a critical regulator of intestinal macrophage activation in patients with IBD and mice with dextran sodium sulfate (DSS)-induced colitis. We find that GM-CSF drives the maturation and polarization of inflammatory intestinal macrophages, promoting anti-microbial functions while suppressing wound-healing transcriptional programs. Group 3 innate lymphoid cells (ILC3s) are a major source of GM-CSF in intestinal inflammation, with a strong positive correlation observed between ILC or CSF2 transcripts and M1 macrophage signatures in IBD mucosal biopsies. Furthermore, GM-CSF-dependent macrophage polarization results in a positive feedback loop that augmented ILC3 activation and type 17 immunity. Together, our data reveal an important role for GM-CSF-mediated ILC-macrophage crosstalk in calibrating intestinal macrophage phenotype to enhance anti-bacterial responses, while inhibiting pro-repair functions associated with fibrosis and stricturing, with important clinical implications.
-
-
-
Immunology and Microbiology
Infected macrophages engage alveolar epithelium to metabolically reprogram myeloid cells and promote antibacterial inflammation
In bioRxiv on 2 March 2020 by Liu, X., Boyer, M. A., et al.
-
-
-
In vivo experiments
-
Mus musculus (Mouse)
-
Cancer Research
-
In vivo experiments
Anti-VEGF therapy resistance in ovarian cancer is caused by GM-CSF-induced myeloid-derived suppressor cell recruitment.
In Br J Cancer on 1 March 2020 by Horikawa, N., Abiko, K., et al.
PubMed
The mechanism of resistance development to anti-VEGF therapy in ovarian cancer is unclear. We focused on the changes in tumour immunity post anti-VEGF therapy.
-
-
-
Immunology and Microbiology
Oncogenic kinase inhibition limits Batf3-dependent dendritic cell development and antitumor immunity.
In J Exp Med on 3 June 2019 by Medina, B. D., Liu, M., et al.
PubMed
Gastrointestinal stromal tumor (GIST) is driven by an activating mutation in the KIT proto-oncogene. Using a mouse model of GIST and human specimens, we show that intratumoral murine CD103+CD11b- dendritic cells (DCs) and human CD141+ DCs are associated with CD8+ T cell infiltration and differentiation. In mice, the antitumor effect of the Kit inhibitor imatinib is partially mediated by CD103+CD11b- DCs, and effector CD8+ T cells initially proliferate. However, in both mice and humans, chronic imatinib therapy decreases intratumoral DCs and effector CD8+ T cells. The mechanism in our mouse model depends on Kit inhibition, which reduces intratumoral GM-CSF, leading to the accumulation of Batf3-lineage DC progenitors. GM-CSF is produced by γδ T cells via macrophage IL-1β. Stimulants that expand and mature DCs during imatinib treatment improve antitumor immunity. Our findings identify the importance of tumor cell oncogene activity in modulating the Batf3-dependent DC lineage and reveal therapeutic limitations for combined checkpoint blockade and tyrosine kinase inhibition.
-
-
-
Immunology and Microbiology
Block of Granulocyte-Macrophage Colony-Stimulating Factor Prevents Inflammation-Induced Preterm Birth in a Mouse Model for Parturition.
In Reprod Sci on 1 April 2019 by Nold, C., Stone, J., et al.
PubMed
A multitude of factors promotes inflammation in the reproductive tract leading to preterm birth. Macrophages peak in the cervix prior to birth and their numbers are increased by the cytokine granulocyte-macrophage colony-stimulating factor (GM-CSF). We hypothesize GM-CSF is produced from multiple sites in the genital tract and is a key mediator in preterm birth.
-
-
-
Cancer Research
-
Immunology and Microbiology
Tumor Microenvironment Remodeling by Intratumoral Oncolytic Vaccinia Virus Enhances the Efficacy of Immune-Checkpoint Blockade.
In Clin Cancer Res on 1 March 2019 by Chon, H. J., Lee, W. S., et al.
PubMed
Cancer immunotherapy is a potent treatment modality, but its clinical benefit depends on the tumor's immune profile. Here, we used mJX-594 (JX), a targeted and GM-CSF-armed oncolytic vaccinia virus, as a strategy to remodel the tumor microenvironment (TME) and subsequently increase sensitivity to αPD-1 and/or αCTLA-4 immunotherapy.
-
-
-
Immunology and Microbiology
Regulation of Lymphatic GM-CSF Expression by the E3 Ubiquitin Ligase Cbl-b.
In Front Immunol on 24 October 2018 by Peer, S., Cappellano, G., et al.
PubMed
Genome-wide association studies as well as lymphatic expression analyses have linked both Cbl-b and GM-CSF to human multiple sclerosis as well as other autoimmune diseases. Both Cbl-b and GM-CSF have been shown to play a prominent role in the development of murine encephalomyelitis; however, no functional connection between the two has yet been established. In this study, we show that Cblb knockout mice demonstrated significantly exacerbated severity of experimental autoimmune encephalomyelitis (EAE), augmented T cell infiltration into the central nervous system (CNS) and strongly increased production of GM-CSF in T cells in vitro and in vivo.GM-CSF neutralization demonstrated that the increased susceptibility of Cblb-/- mice to EAE was dependent on GM-CSF. Mechanistically, p50 binding to the GM-CSF promoter and the IL-3/GM-CSF enhancer element "CNSa" was strongly increased in nuclear extracts from Cbl-b-deficient T cells. This study suggests that Cbl-b limits autoimmunity by preventing the pathogenic effects of GM-CSF overproduction in T cells.
-
-
-
Immunology and Microbiology
Skin-Specific CD301b+ Dermal Dendritic Cells Drive IL-17-Mediated Psoriasis-Like Immune Response in Mice.
In J Invest Dermatol on 1 April 2018 by Kim, T. G., Kim, S. H., et al.
PubMed
Conventional dendritic cells (cDCs) are composed of heterogeneous subsets commonly arising from dendritic cell (DC)-committed progenitors. A population of CD301b-expressing DCs has recently been identified in non-lymphoid barrier tissues such as skin. However, whether CD301b+ DCs in the skin represent an ontogenetically unique subpopulation of migratory cDCs has not been fully addressed. Here, we demonstrated that CD301b+ dermal DCs were distinct subpopulation of FMS-like tyrosine kinase 3 ligand (FLT3L)-dependent CD11b+ cDC2 lineage, which required an additional GM-CSF cue for the adequate development. Although the majority of lymphoid-resident cDC2 lacked CD301b expression, dermal migratory cDC2 contained a substantial fraction of CD301b+ subset. Similar to CD301b- population, CD301b+ dermal DC development was closely regulated by FLT3 signaling, suggesting their common origin from FLT3L-responsive cDC progenitors. However, FLT3L-driven cDC progenitor culture was not sufficient, but additional GM-CSF treatment was required to produce CD301b+ cDC2. In vivo development of CD301b+ cDC2 was significantly augmented by exogenous GM-CSF, while the repopulation of CD301b+ dermal cDC2 was abrogated by GM-CSF neutralization. Functionally, CD301b+ cDC2 was capable of producing a high level of IL-23, and the depletion of CD301b+ cDC2 effectively prevented IL-17-mediated psoriasiform dermatitis. Therefore, our findings highlight the differentiation program of a distinct CD301b+ dermal cDC2 subset in the skin and its involvement in psoriatic inflammation.
-